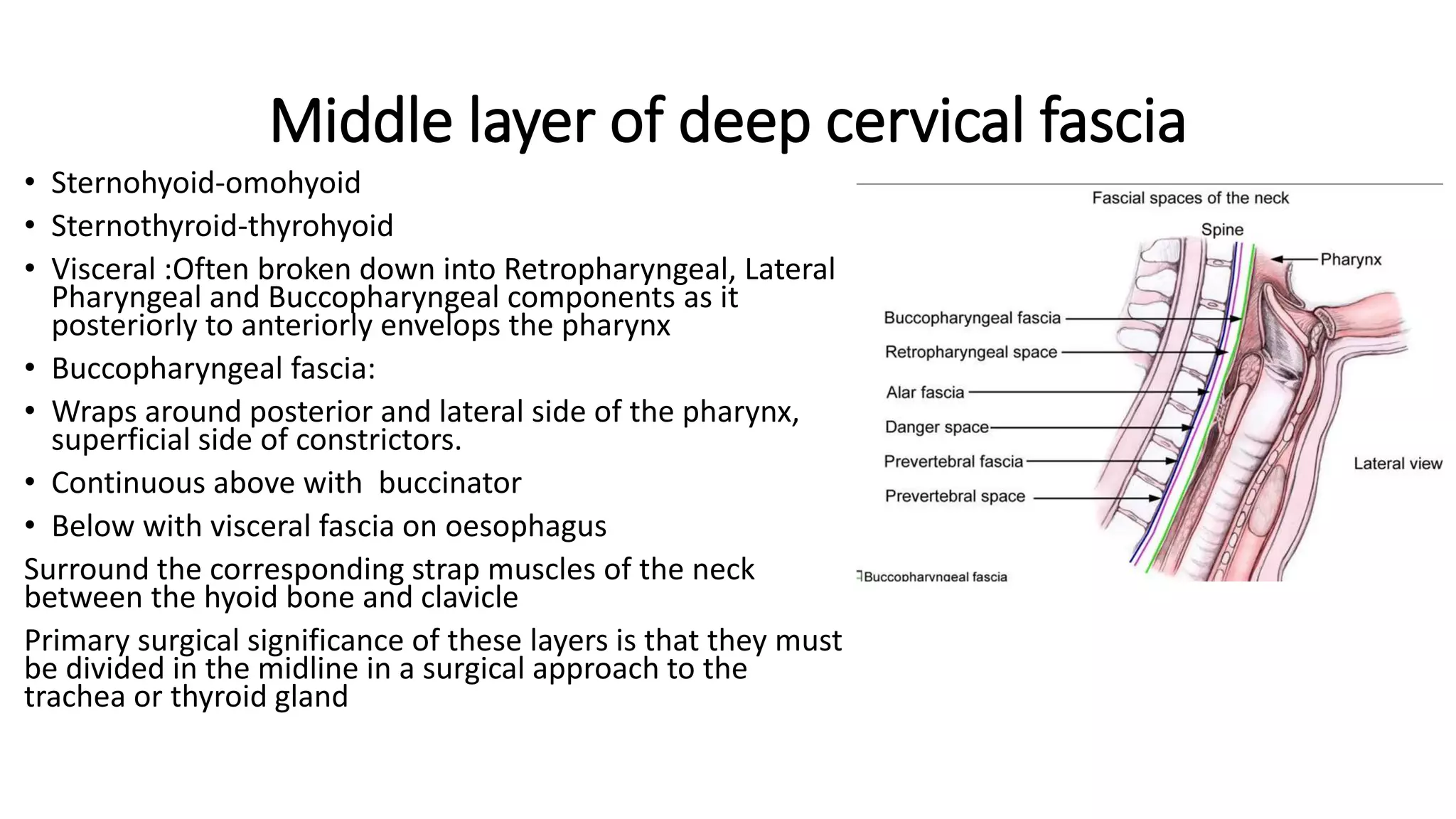
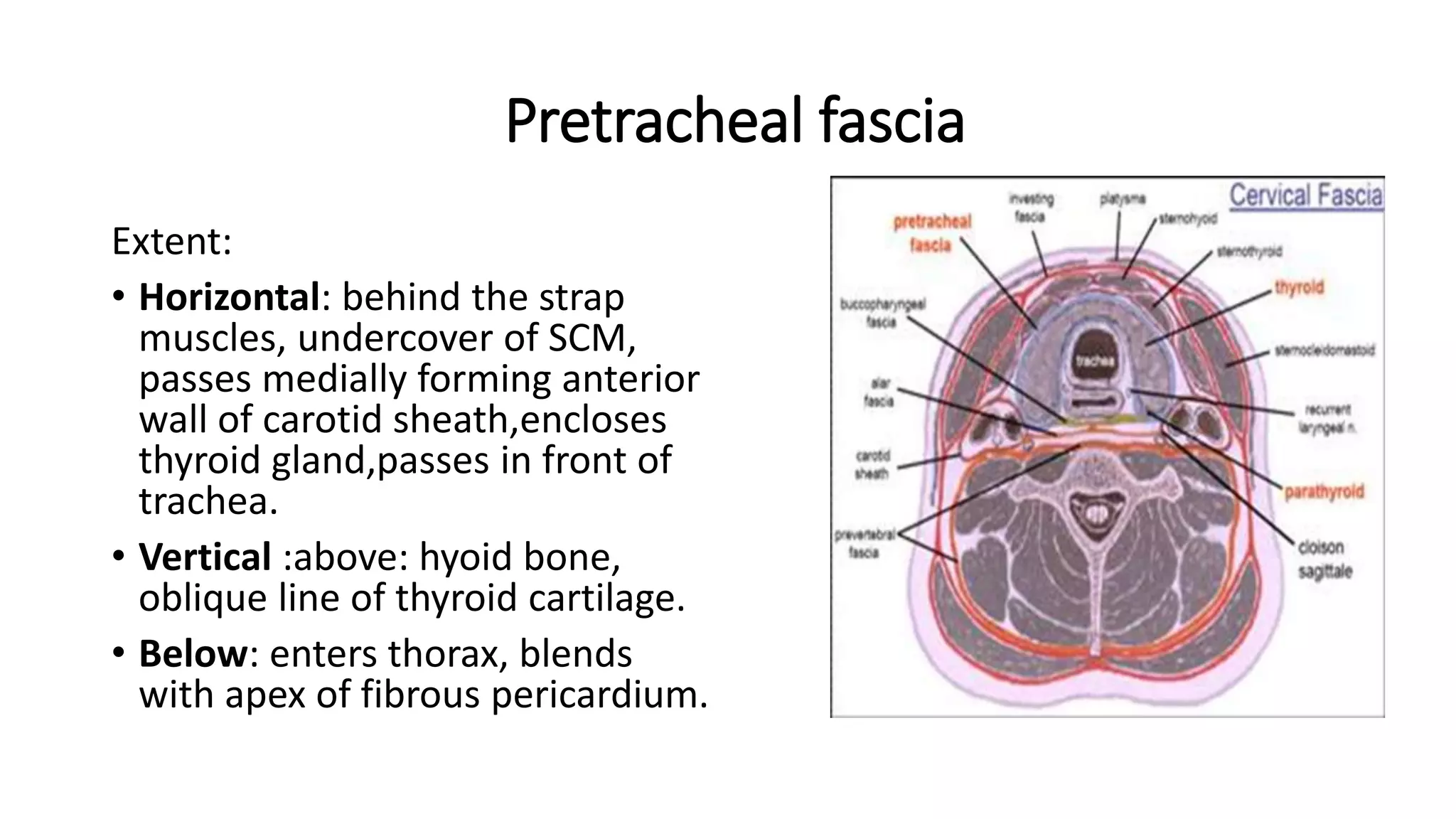
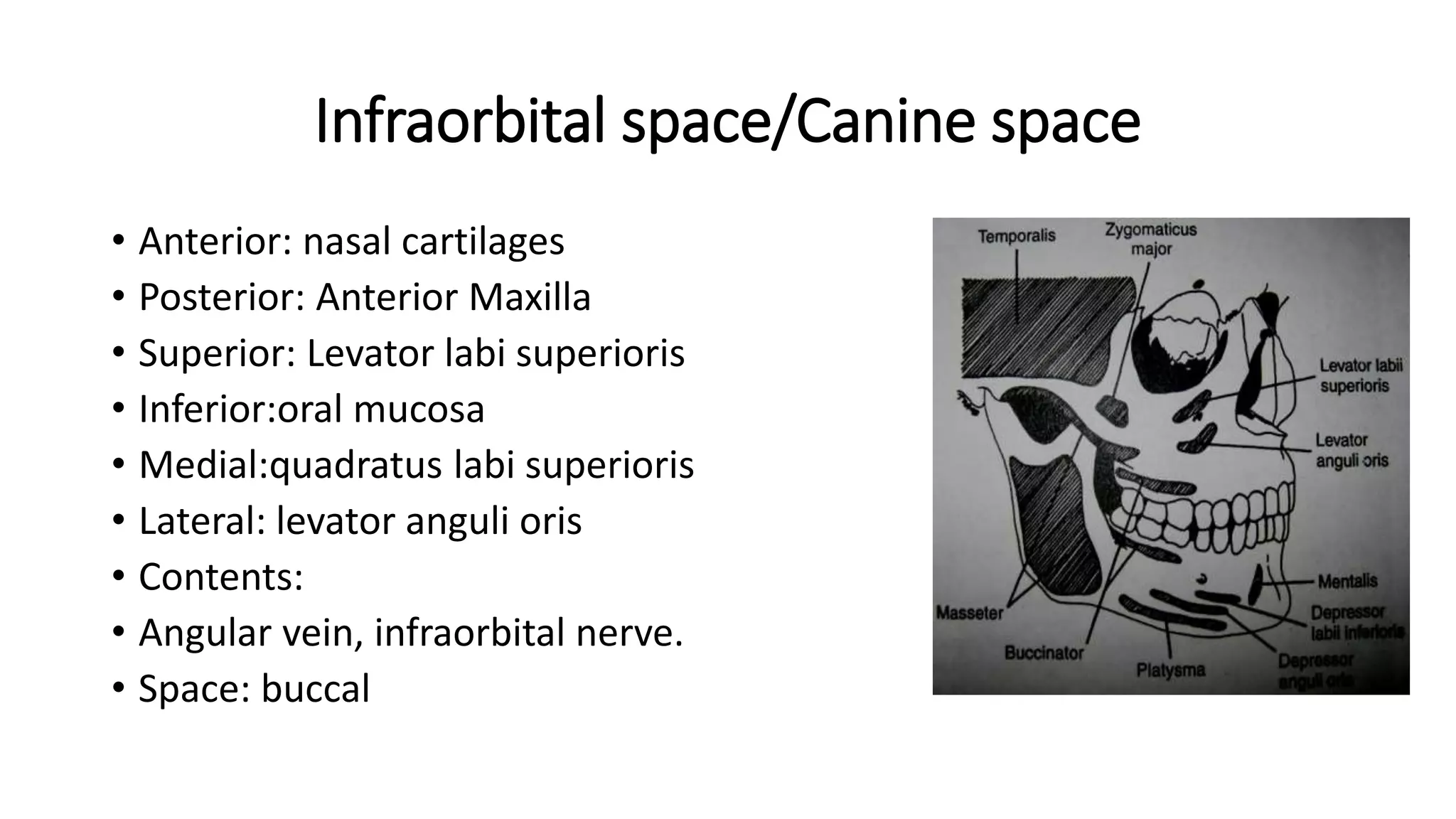
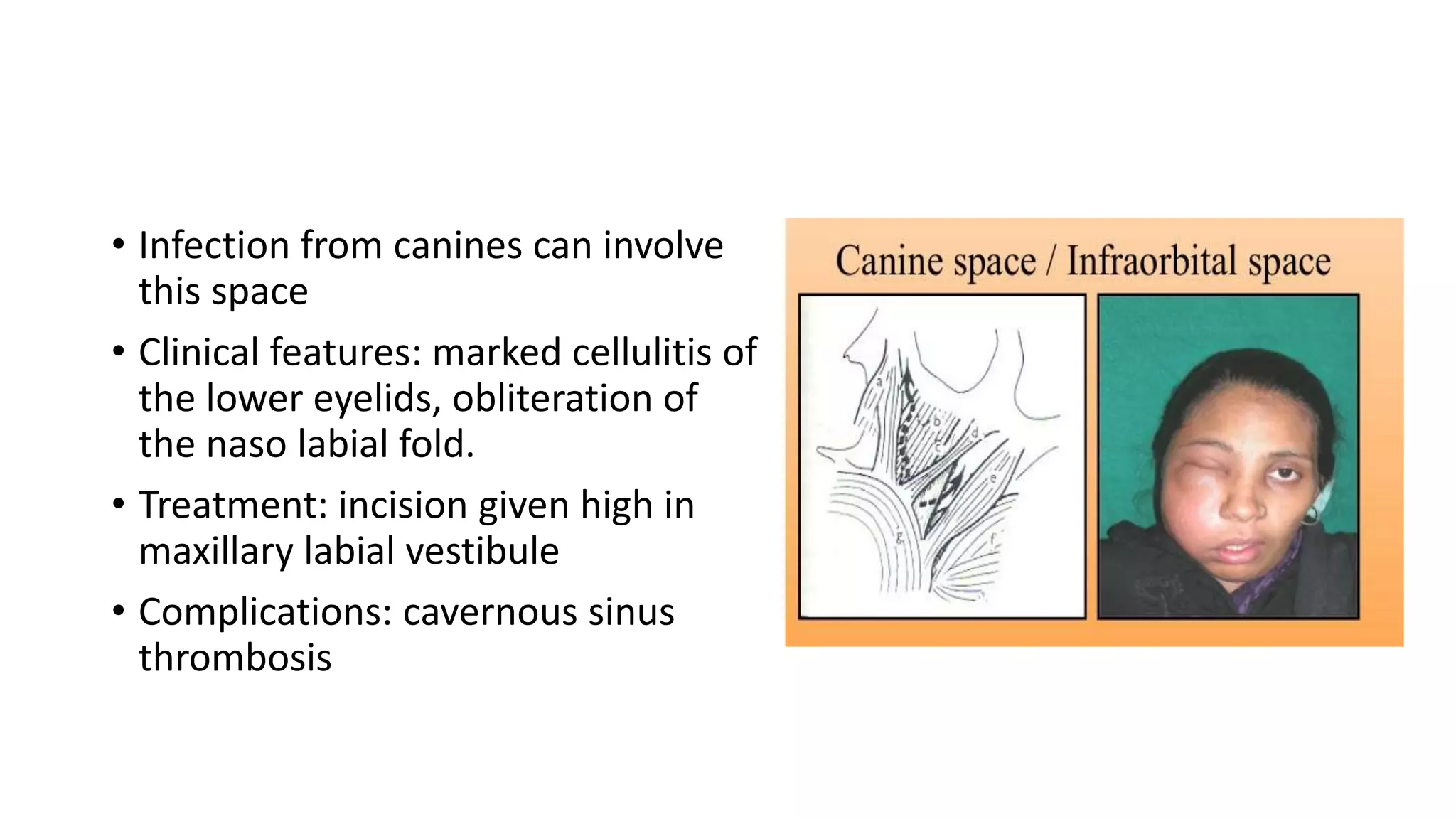
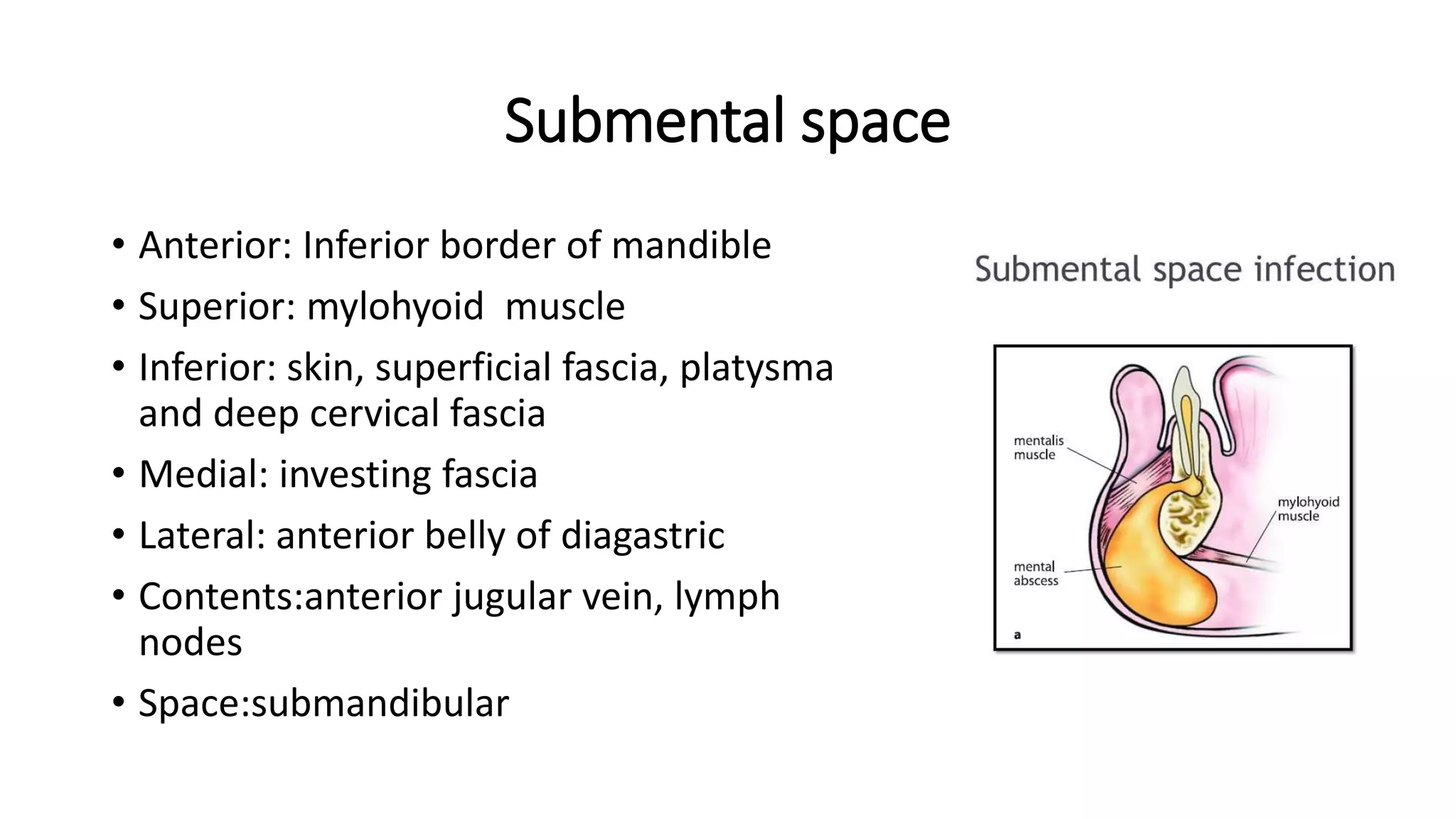
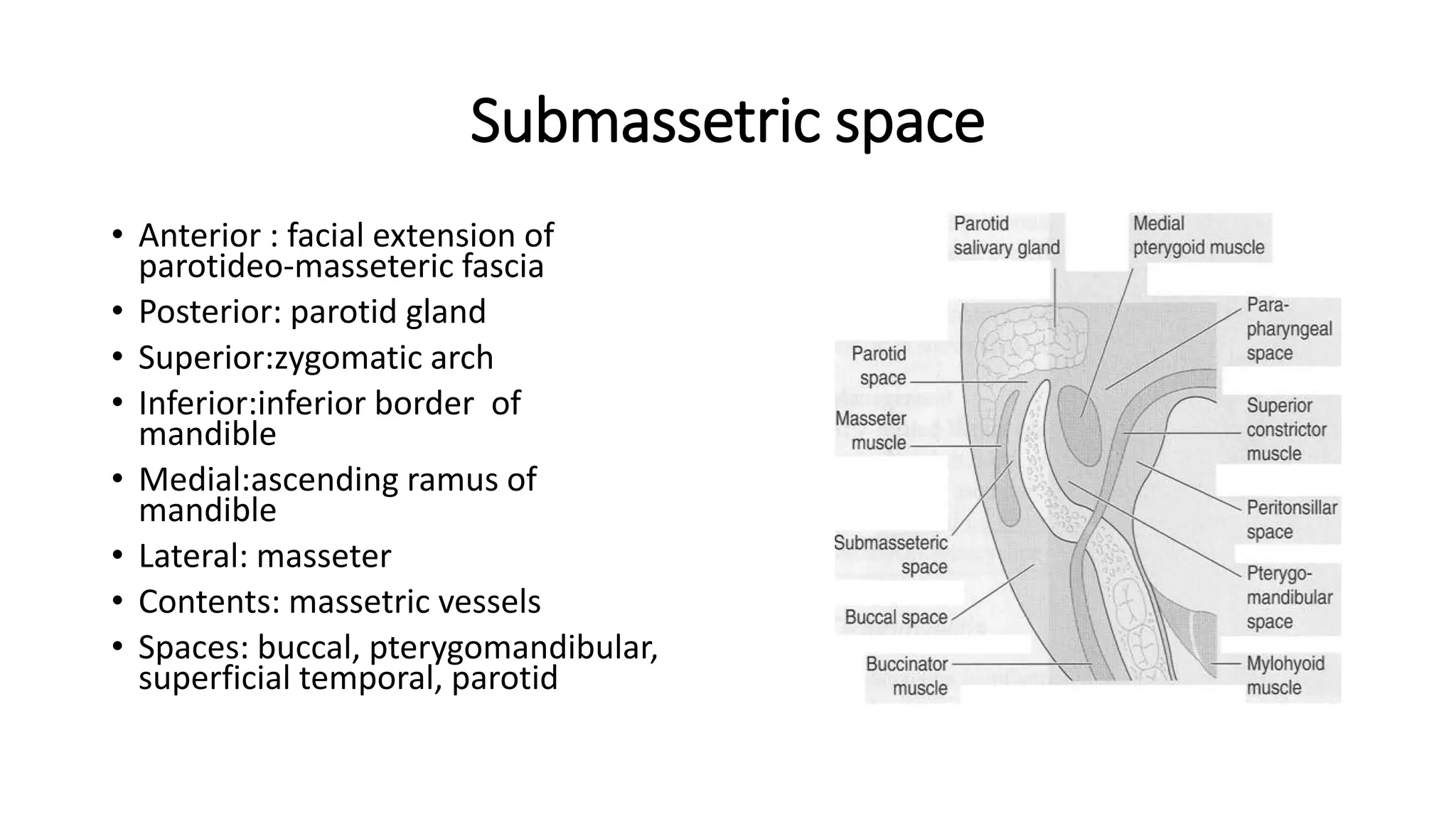
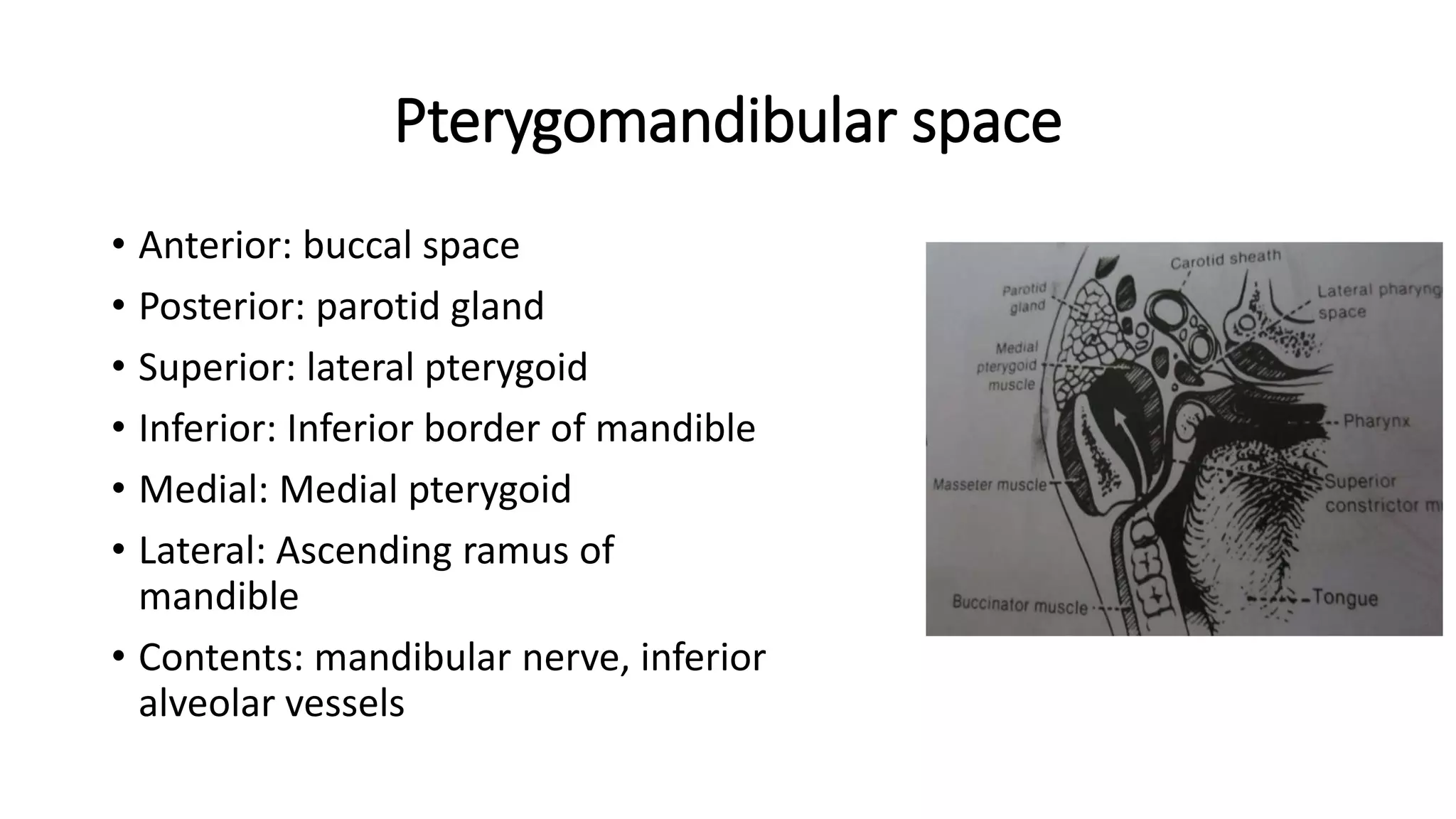
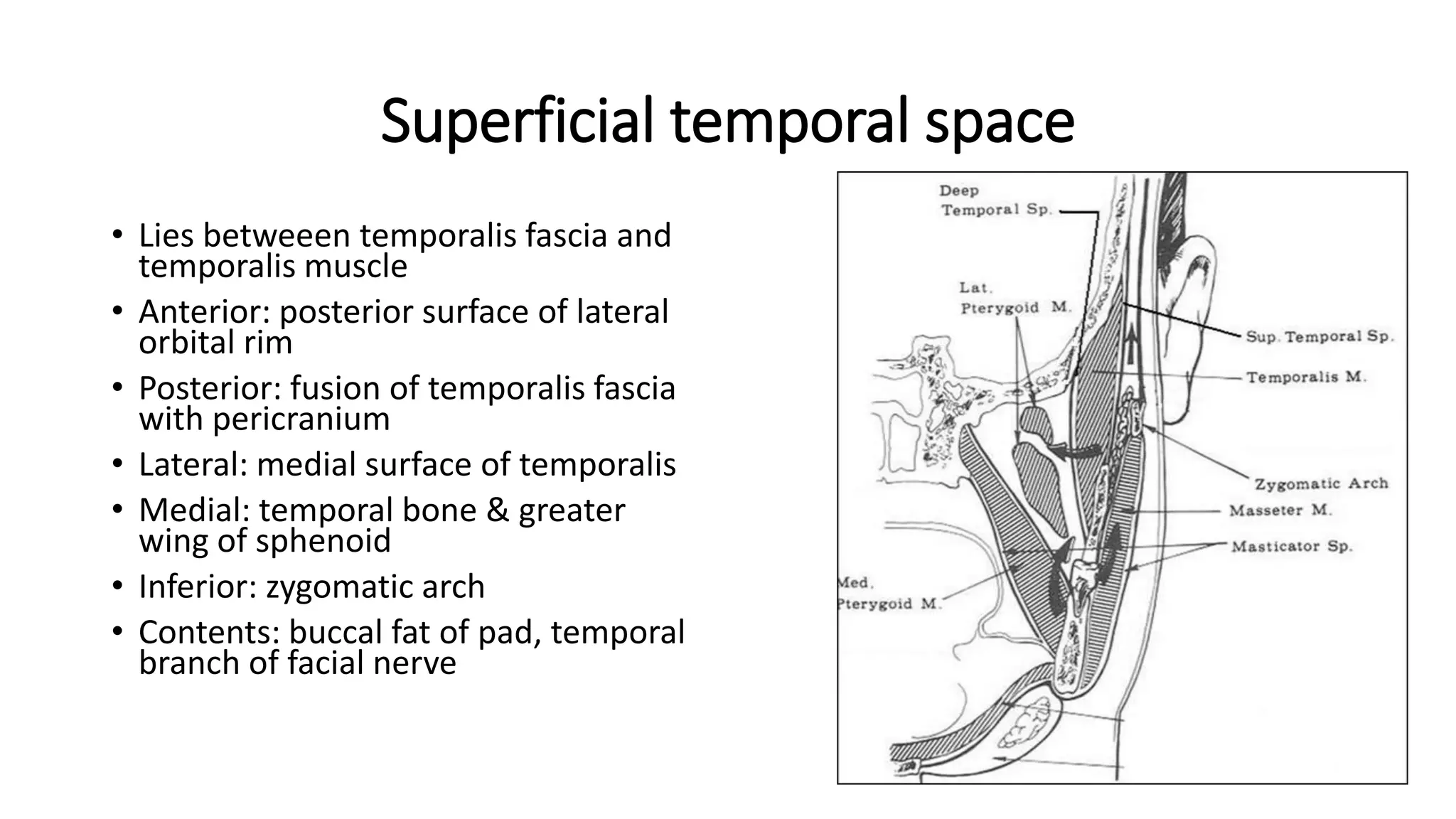
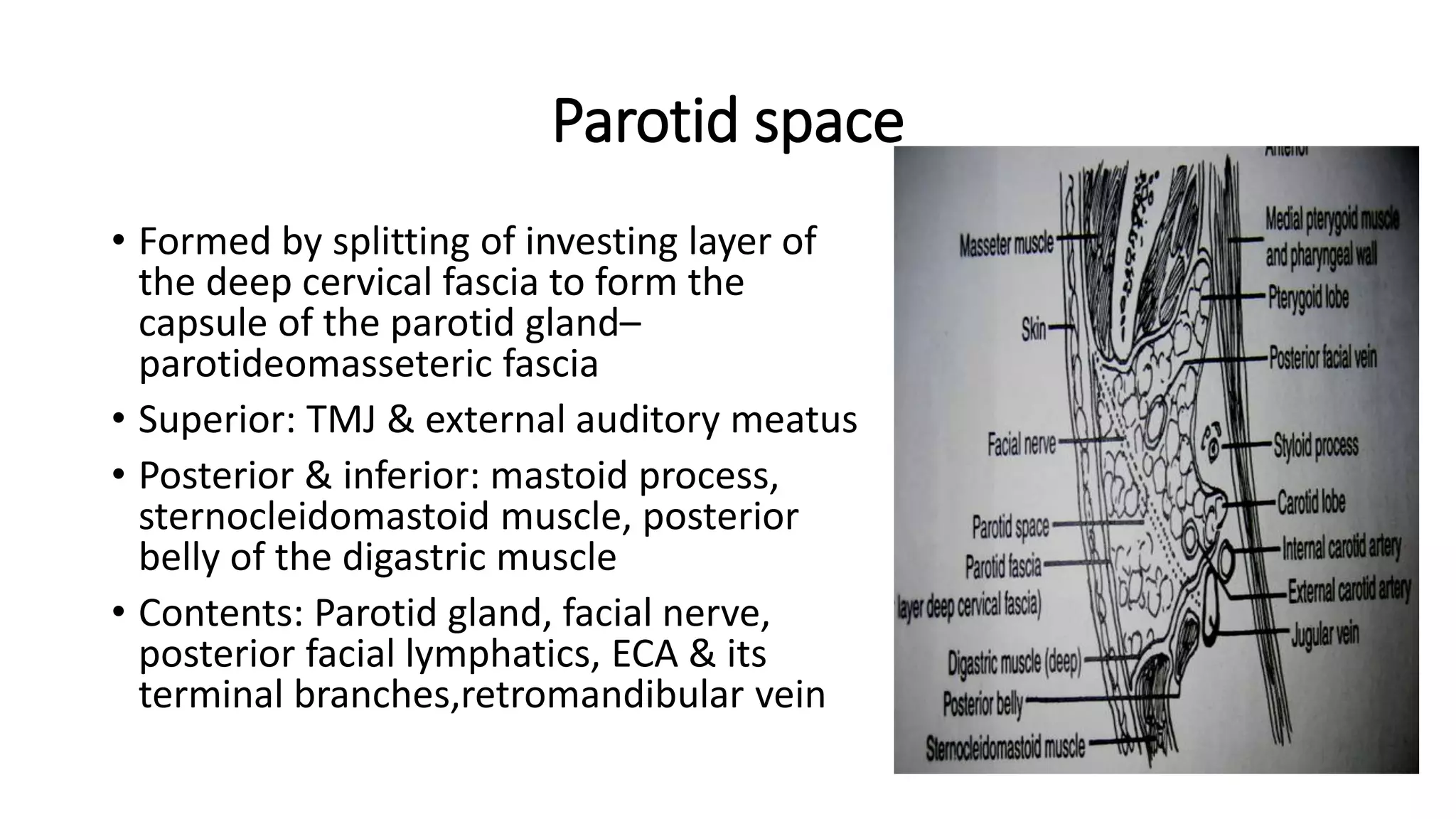
The document provides an extensive overview of fascial spaces in the head and neck, including their definitions, classification, and roles in infections. It details various fascial layers such as superficial and deep fascia, along with specific spaces and their clinical significance in terms of infection spread and surgical approaches. The document also outlines treatment options for conditions arising from these spaces, emphasizing the importance of anatomical knowledge for effective management.