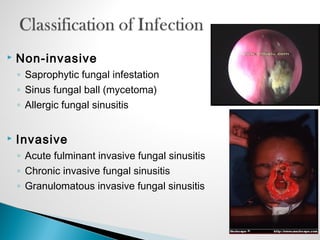
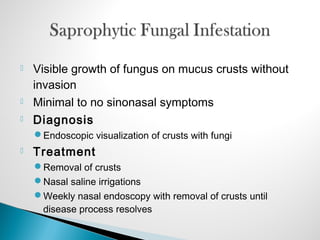
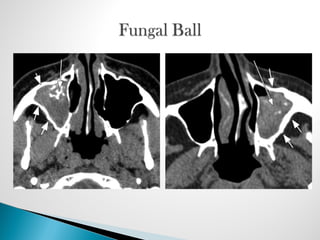
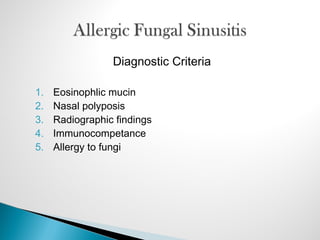
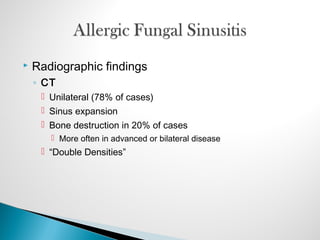
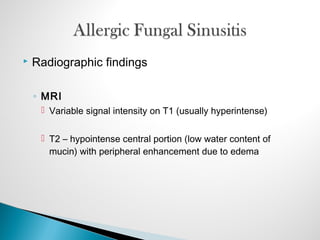
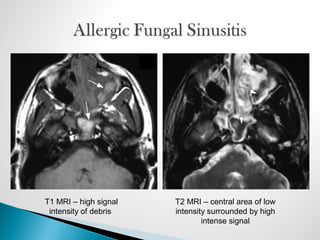
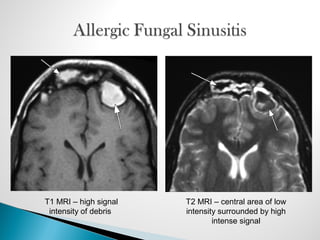
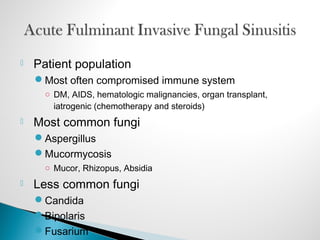
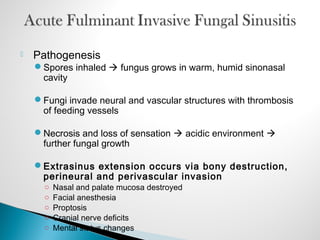
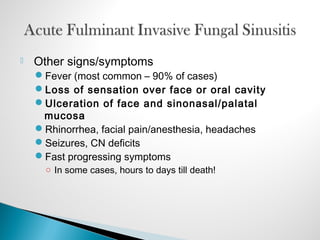
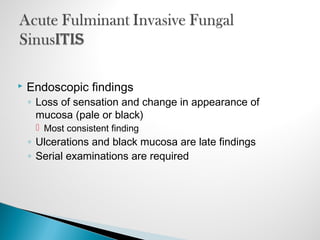
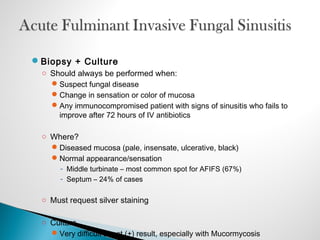
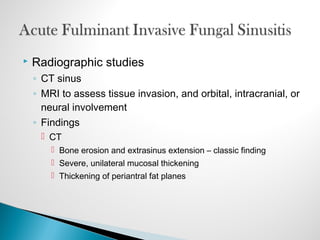
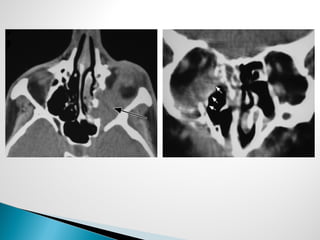
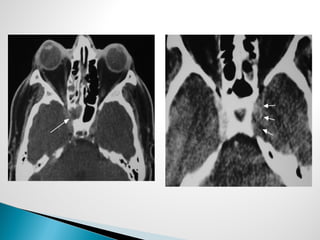
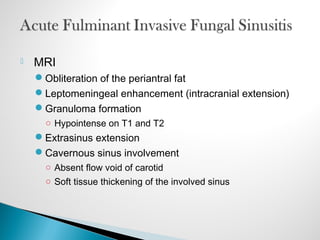
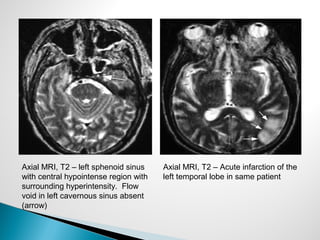
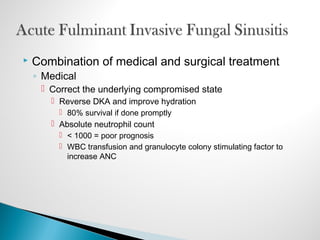
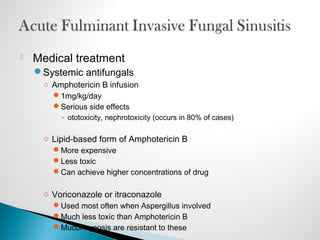
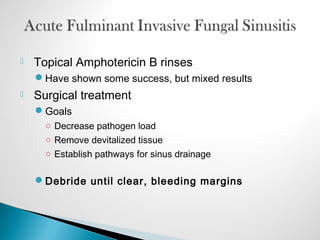
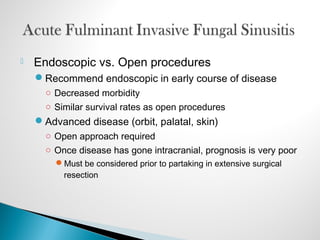
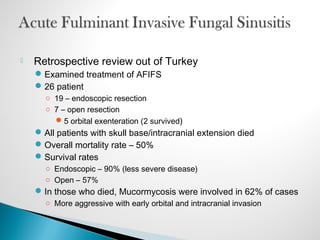
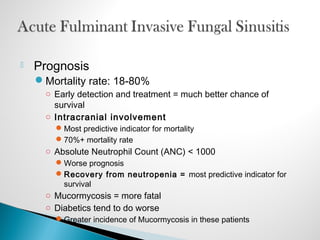
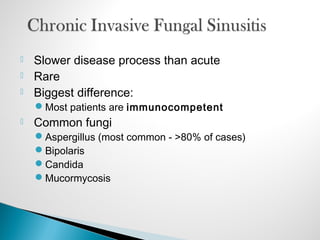
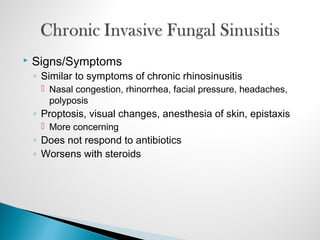
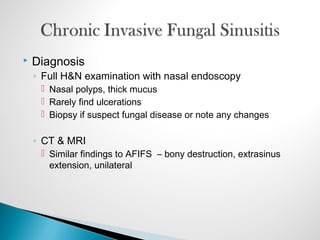
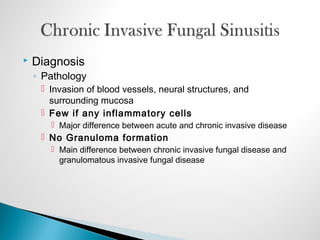
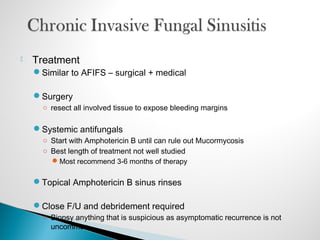
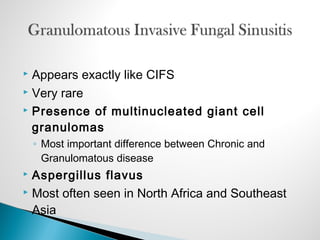
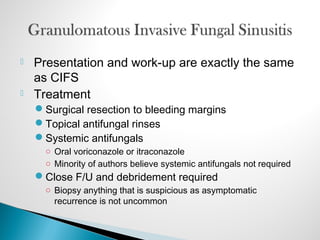
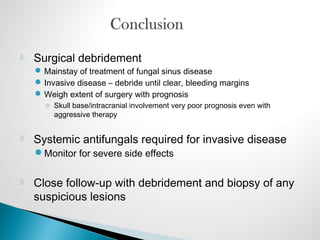
Fungi can cause both non-invasive and invasive sinus disease. Non-invasive types include fungal balls and allergic fungal sinusitis, treated with surgery and antifungals. Invasive fungal sinusitis occurs in immunocompromised patients and can be acute or chronic. It involves fungal invasion and tissue destruction. Diagnosis involves biopsy and imaging of bone erosion and extrasinus spread. Treatment requires surgical debridement and antifungals, with a poor prognosis if the infection spreads intracranially.