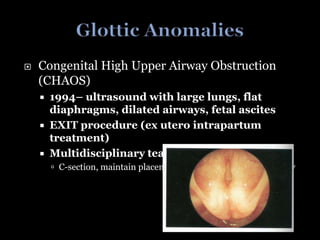
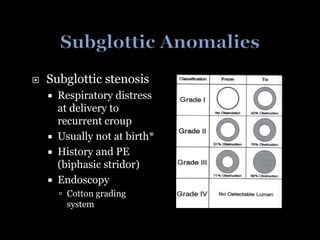
The document discusses various medical conditions and procedures related to respiratory obstruction, including stridor, dyspnea, and congenital high upper airway obstruction. It also covers topics such as subglottic stenosis, ear infections, and symptoms of herpes simplex virus infections in children. Treatment recommendations and complications associated with these conditions are highlighted throughout.