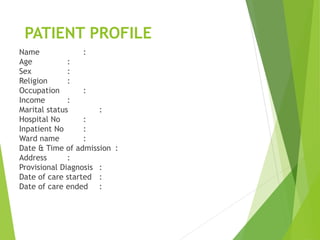
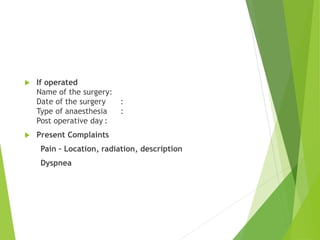
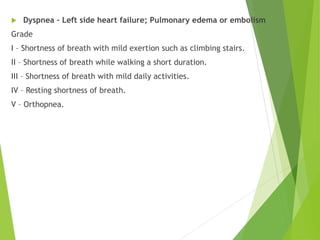
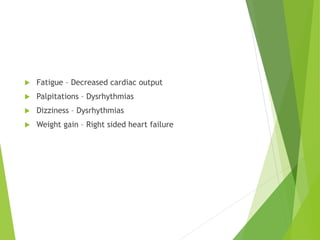
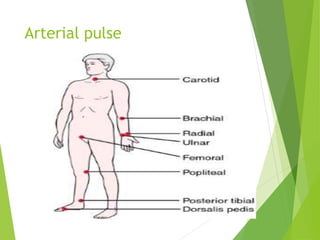
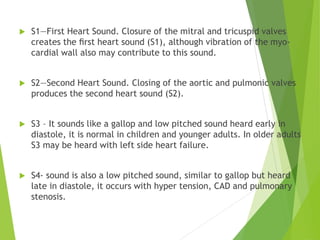
This document provides information on assessing the cardiovascular system, including history taking and physical examination. It discusses taking a patient's history, including socioeconomic status, family history, personal history, and present health status. For the physical exam, it describes assessing vital signs, inspecting the head, eyes, ears, nose, mouth, respiratory system, and cardiovascular system. It provides details on palpating and auscultating the heart. The document is intended as a guide for healthcare providers on evaluating the cardiovascular system.