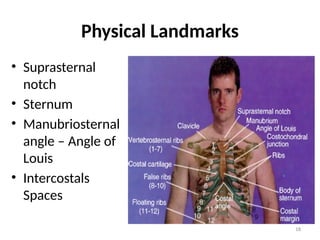
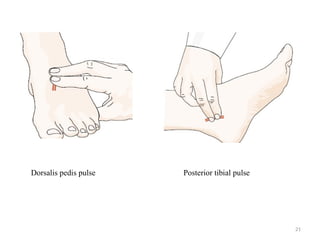
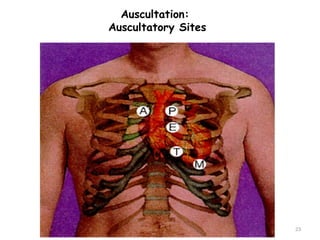
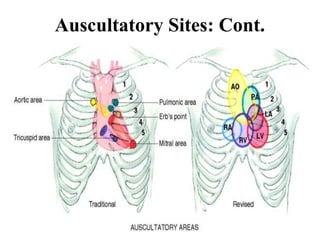
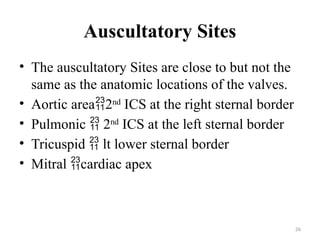
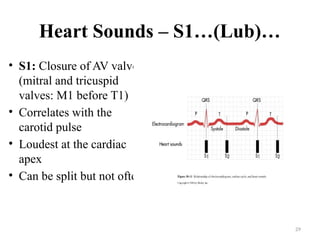
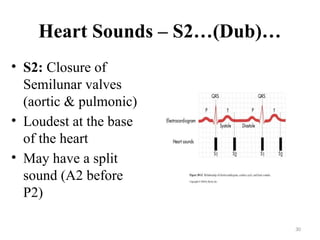
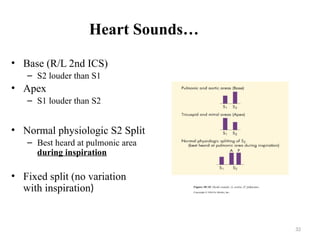
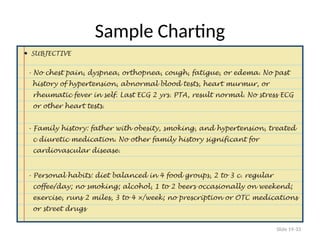
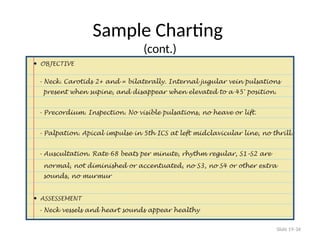
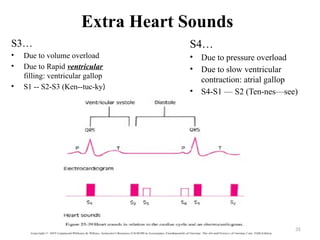
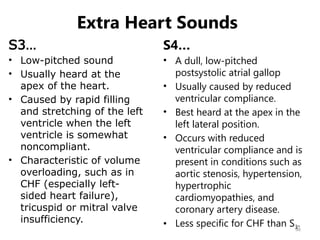
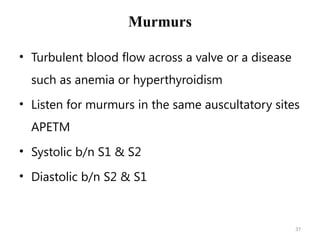
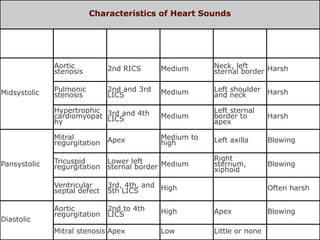
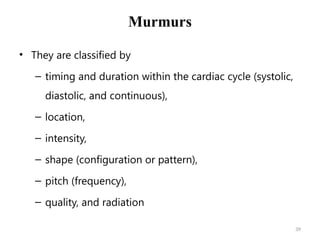
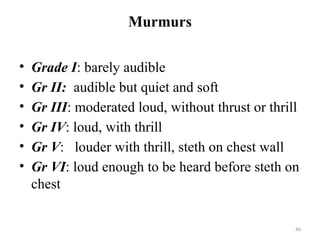
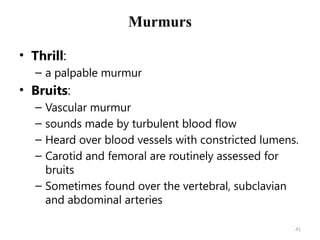
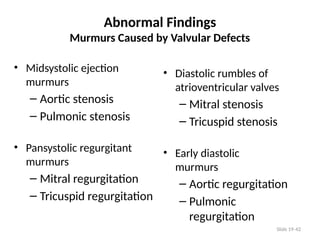
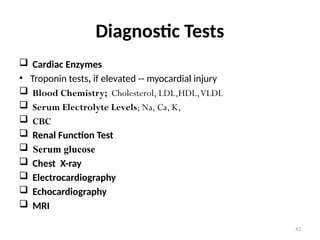
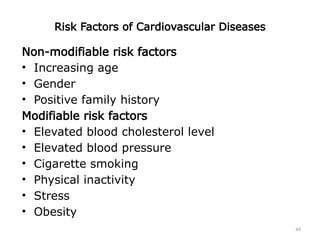
The document outlines a comprehensive nursing health assessment of the cardiovascular system, detailing the purpose, subjective and objective data collection methods, and examination techniques. It covers various assessment techniques such as palpation, auscultation, and observation of heart sounds, including identification of abnormal findings like murmurs and extra heart sounds. Additionally, it discusses relevant diagnostic tests and risk factors associated with cardiovascular diseases.