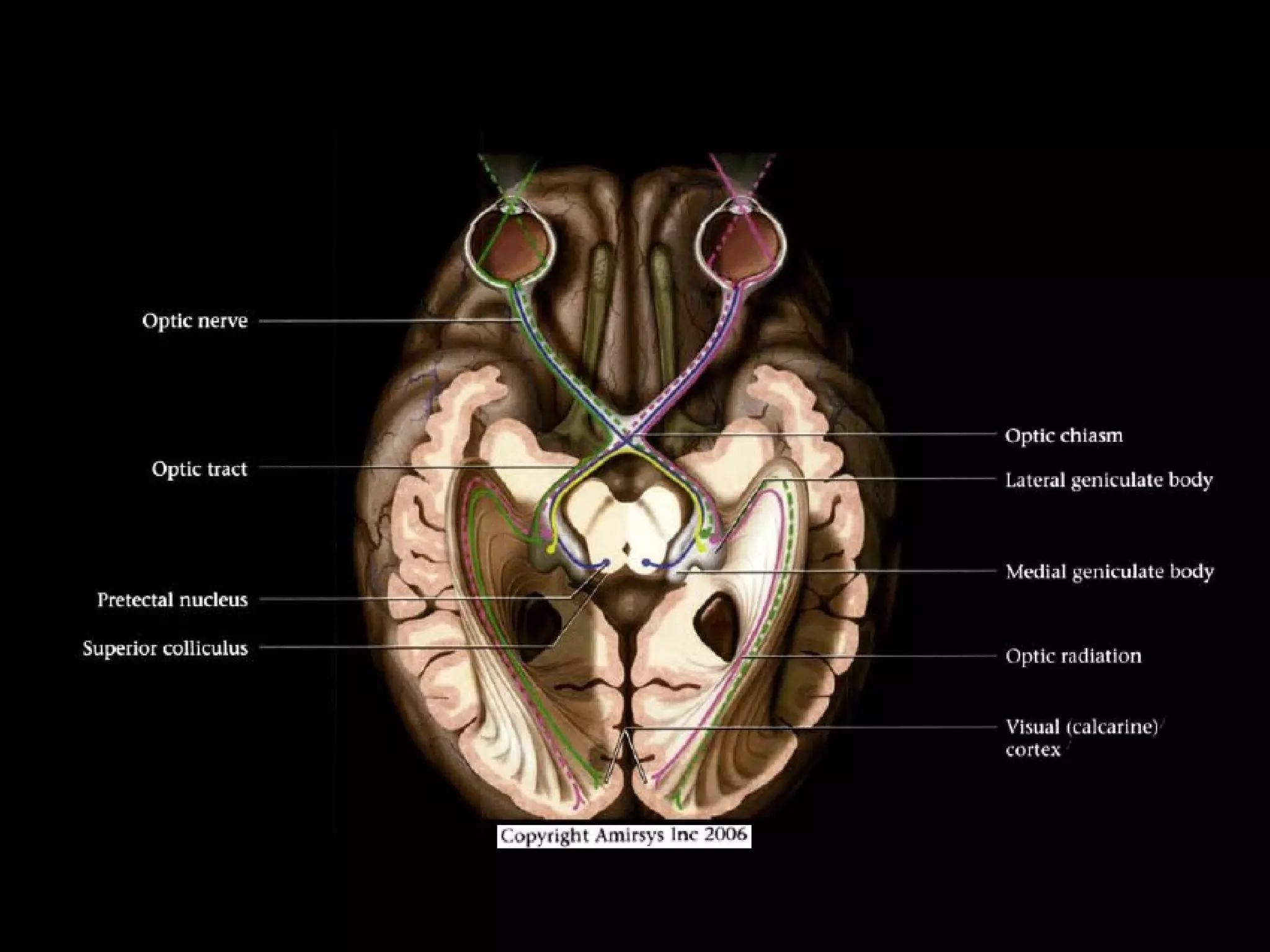
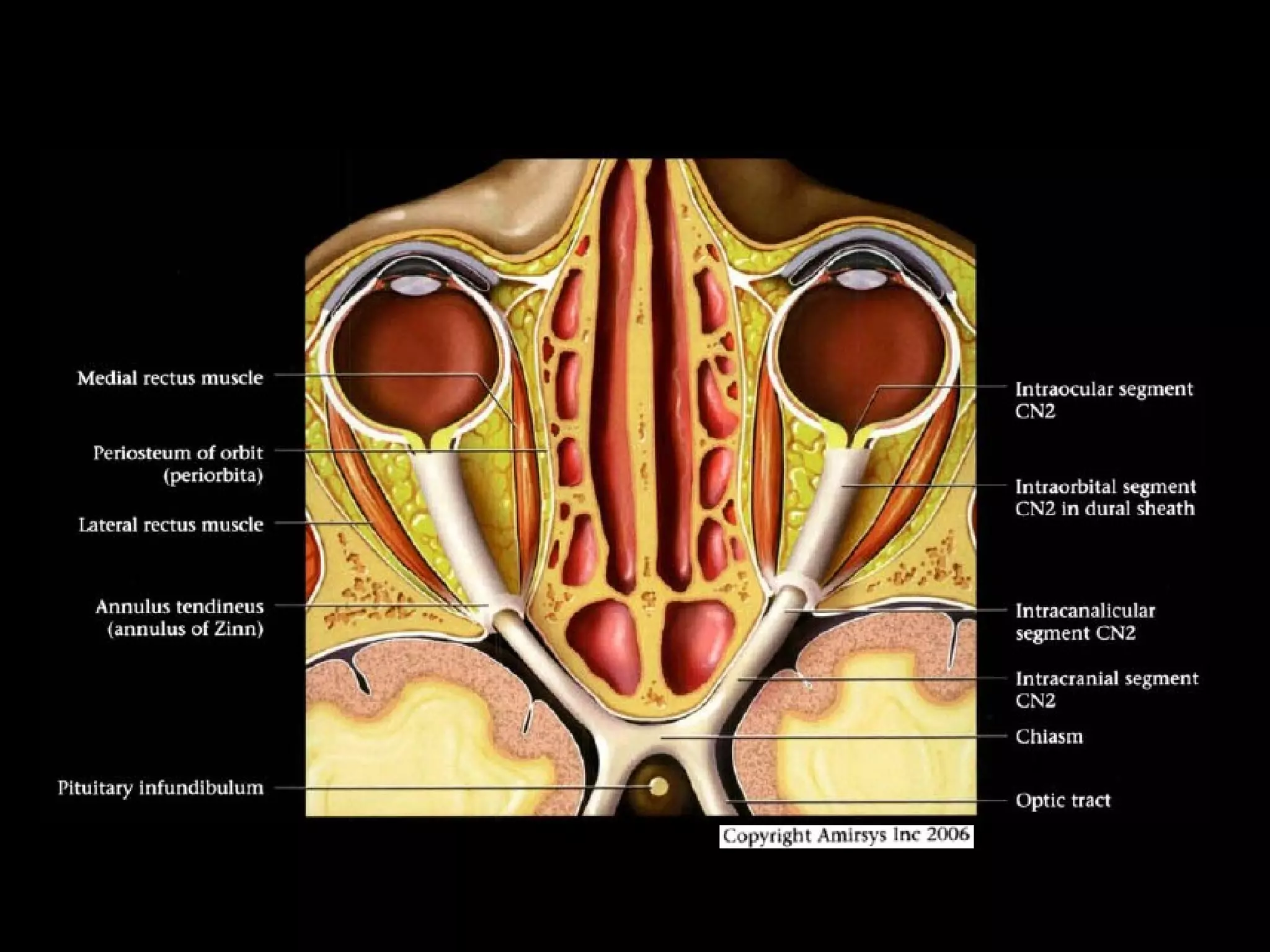
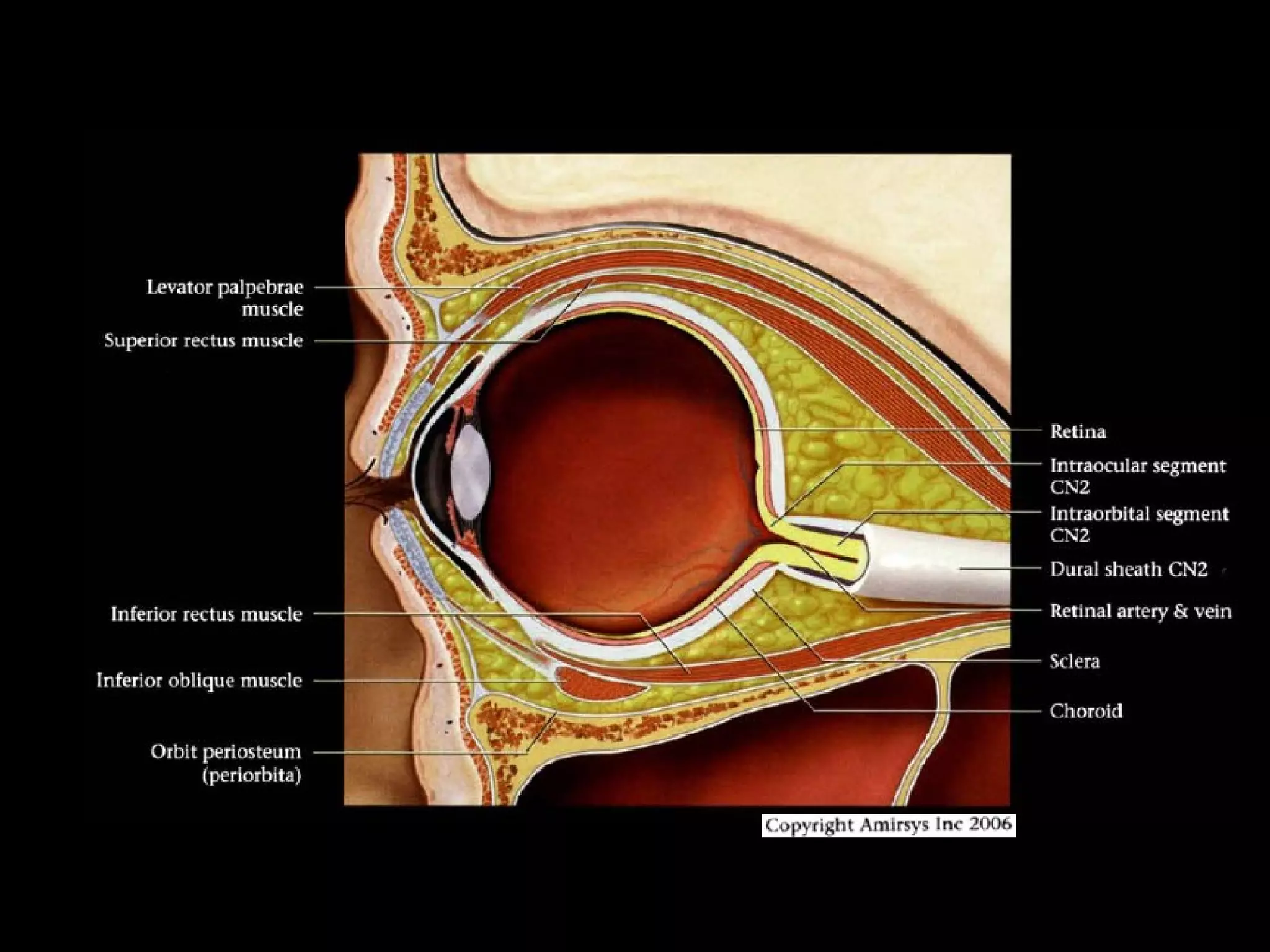
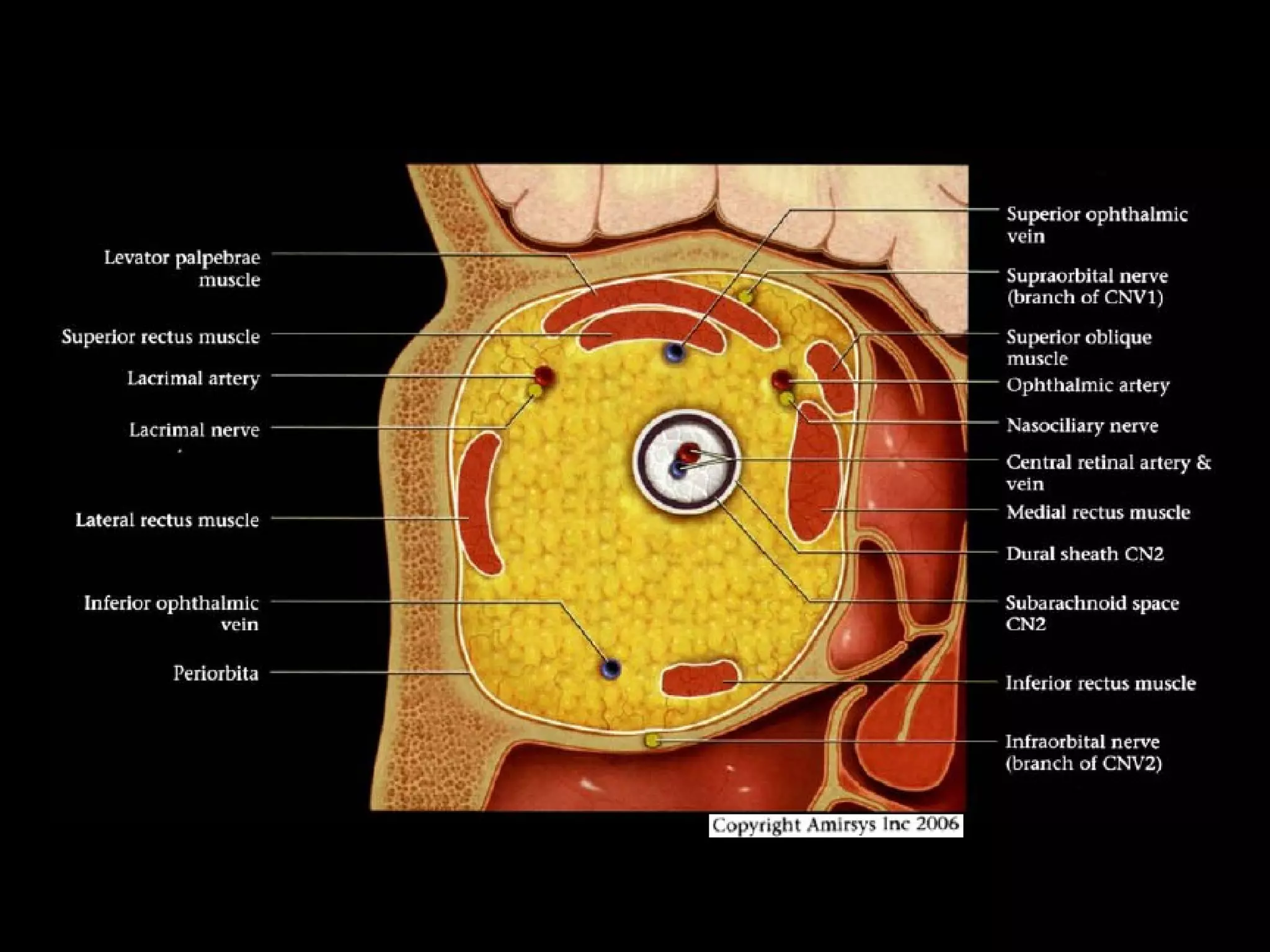
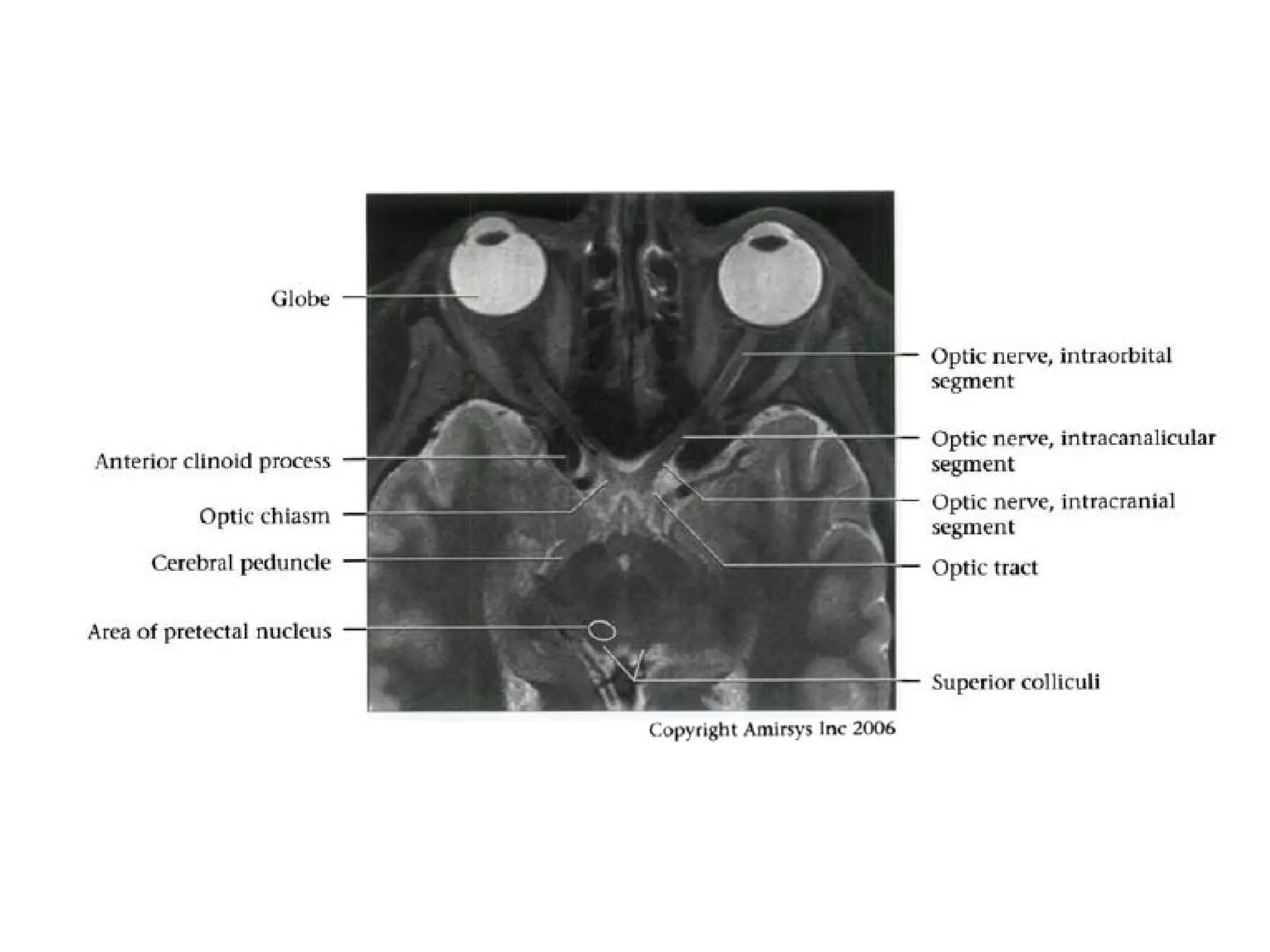
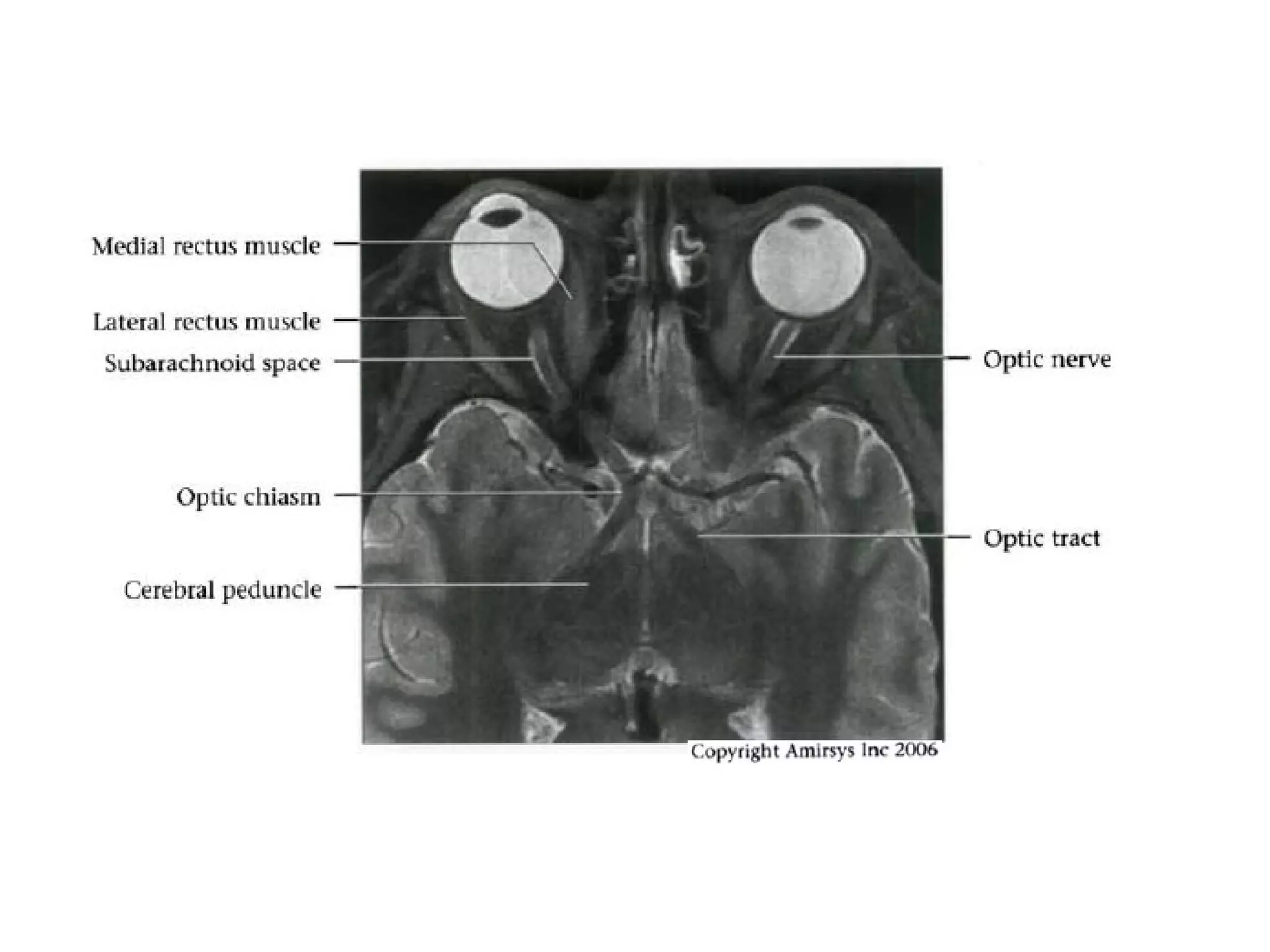
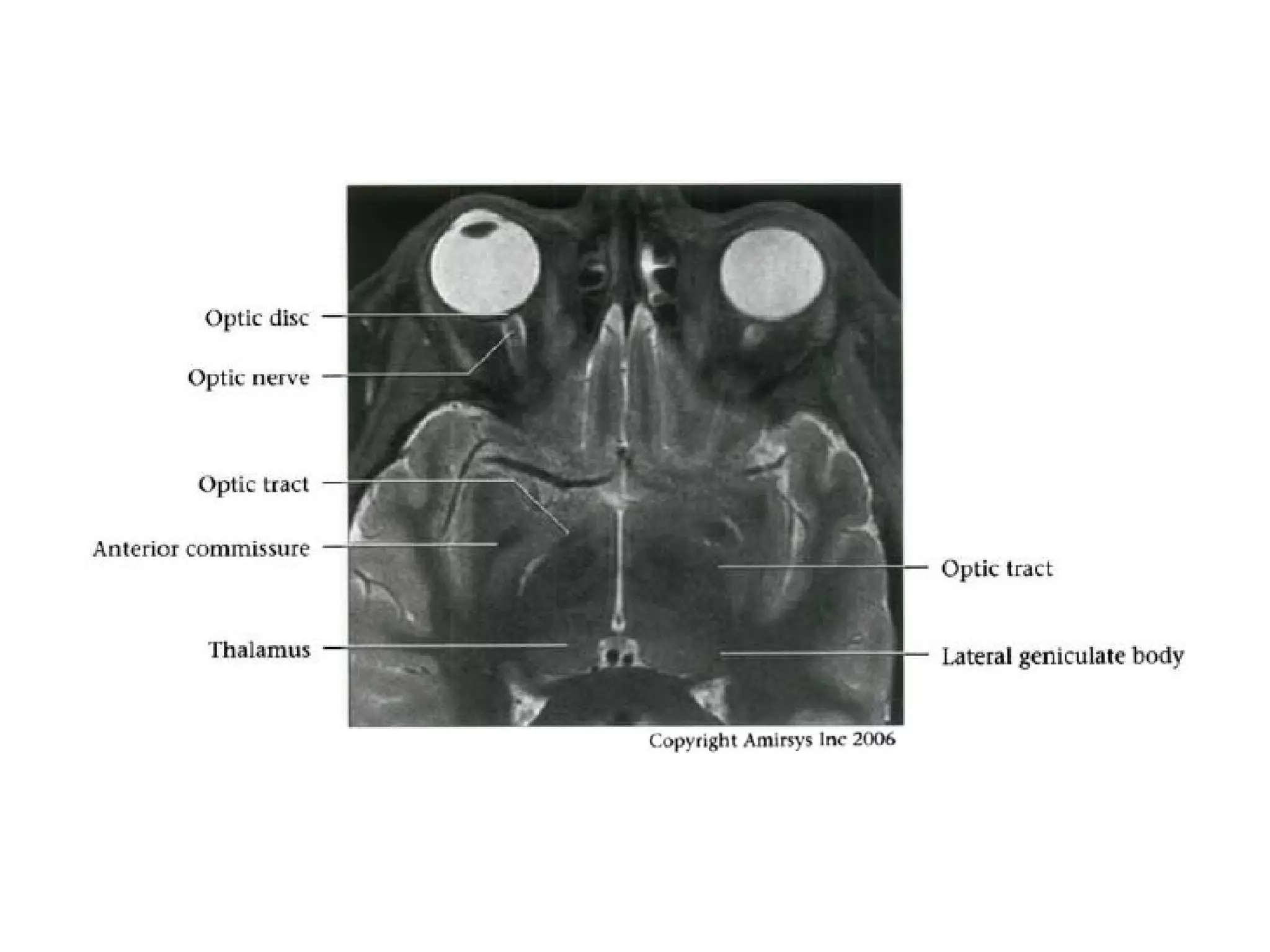
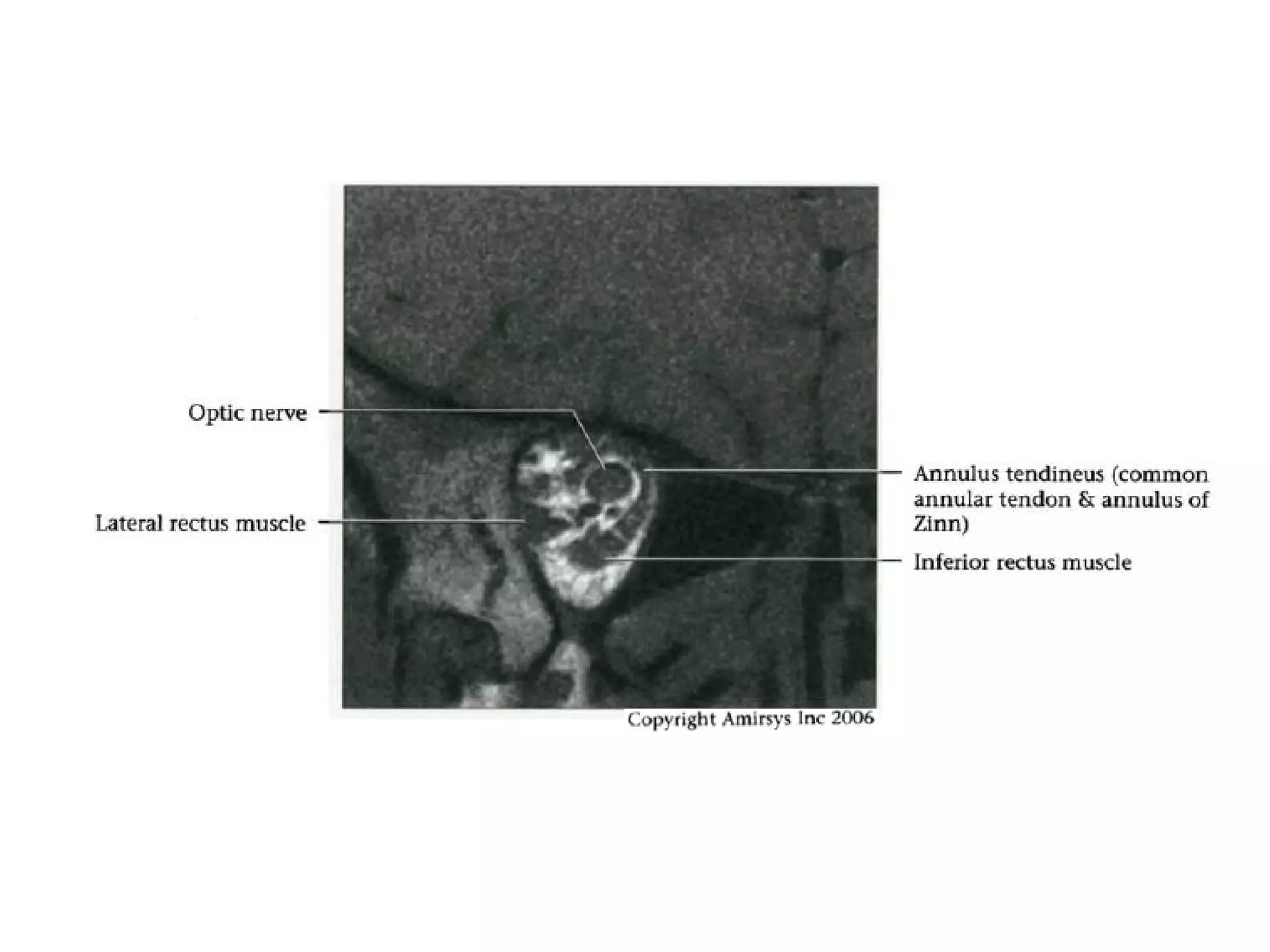
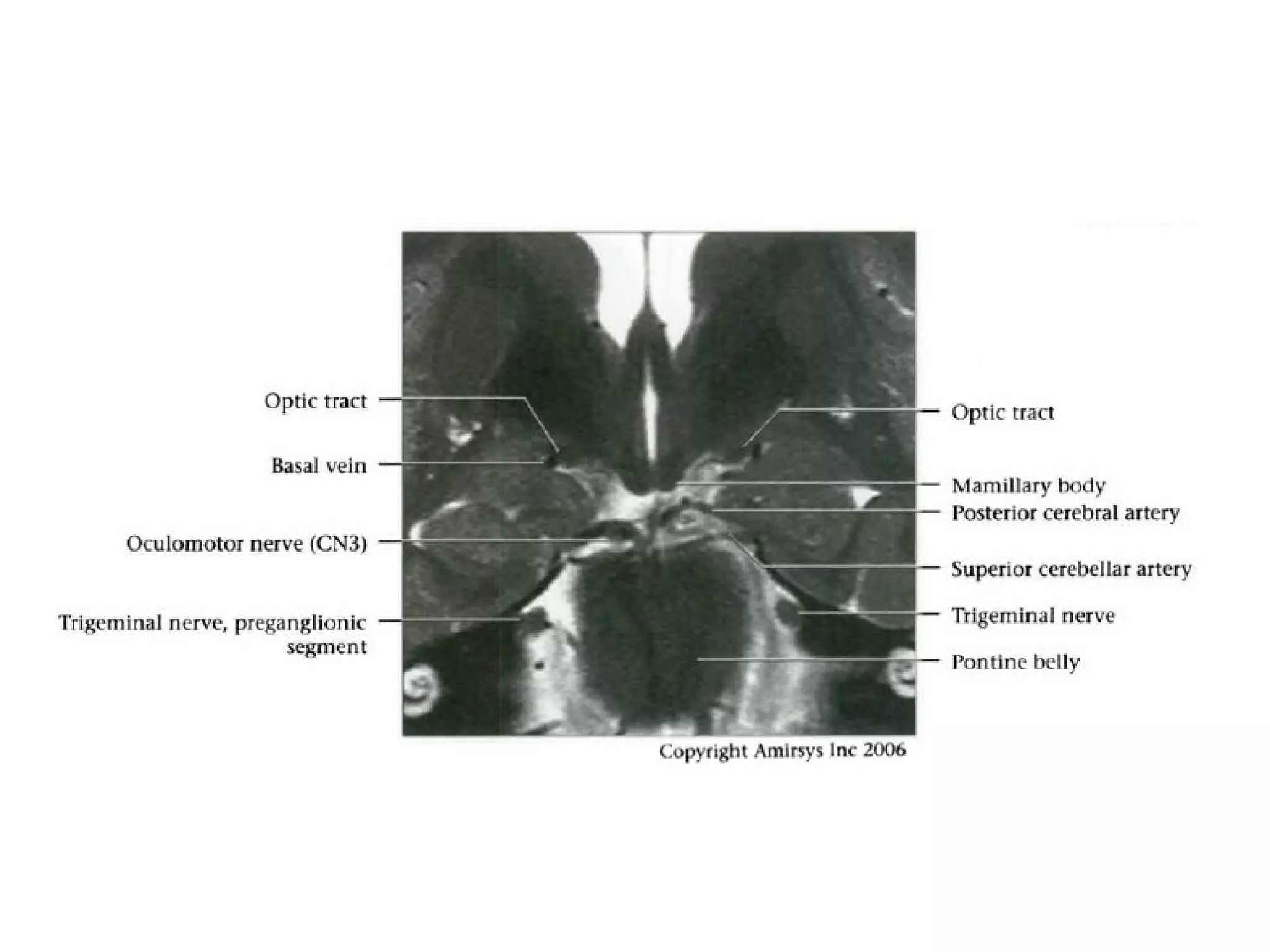
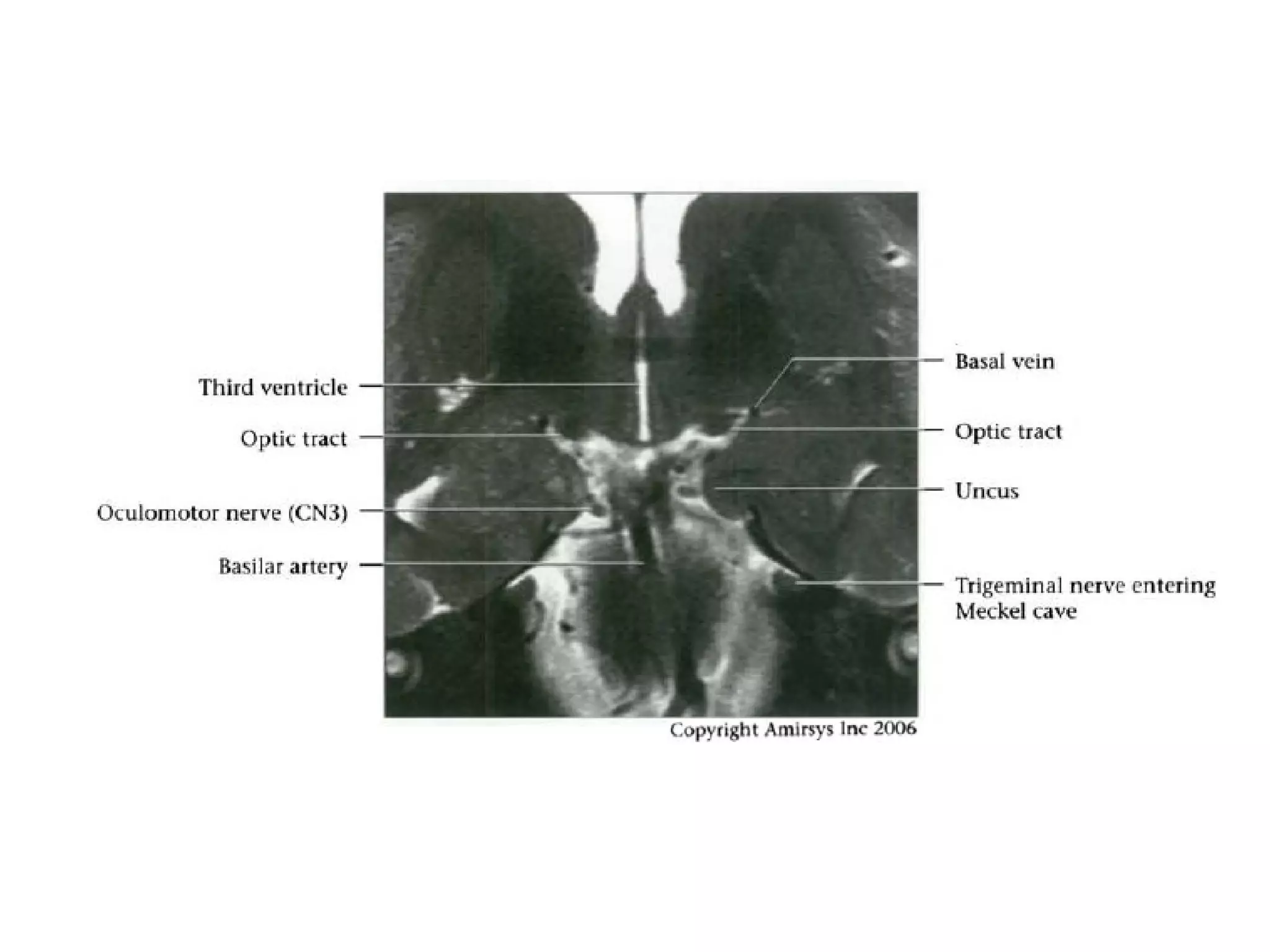
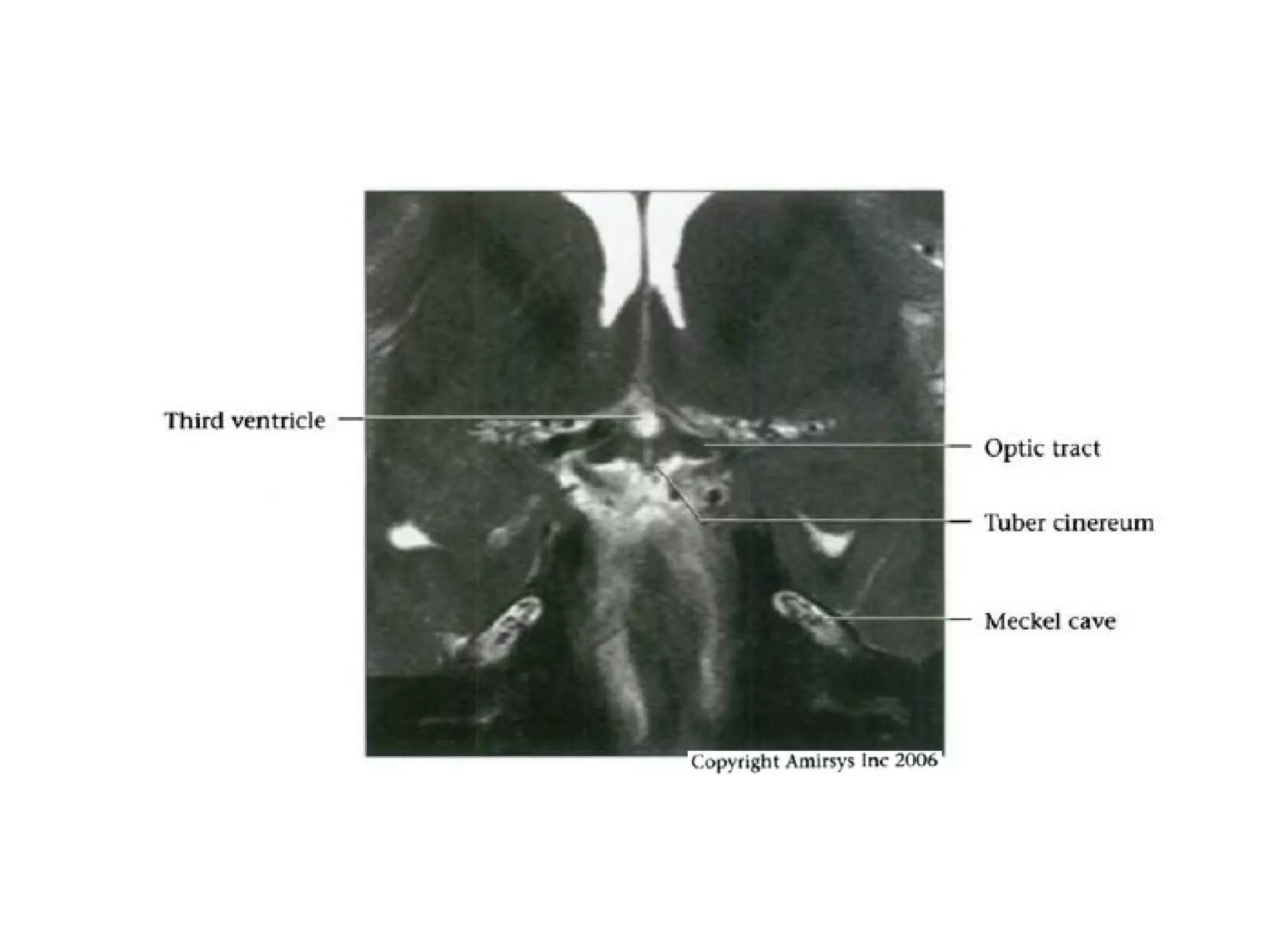
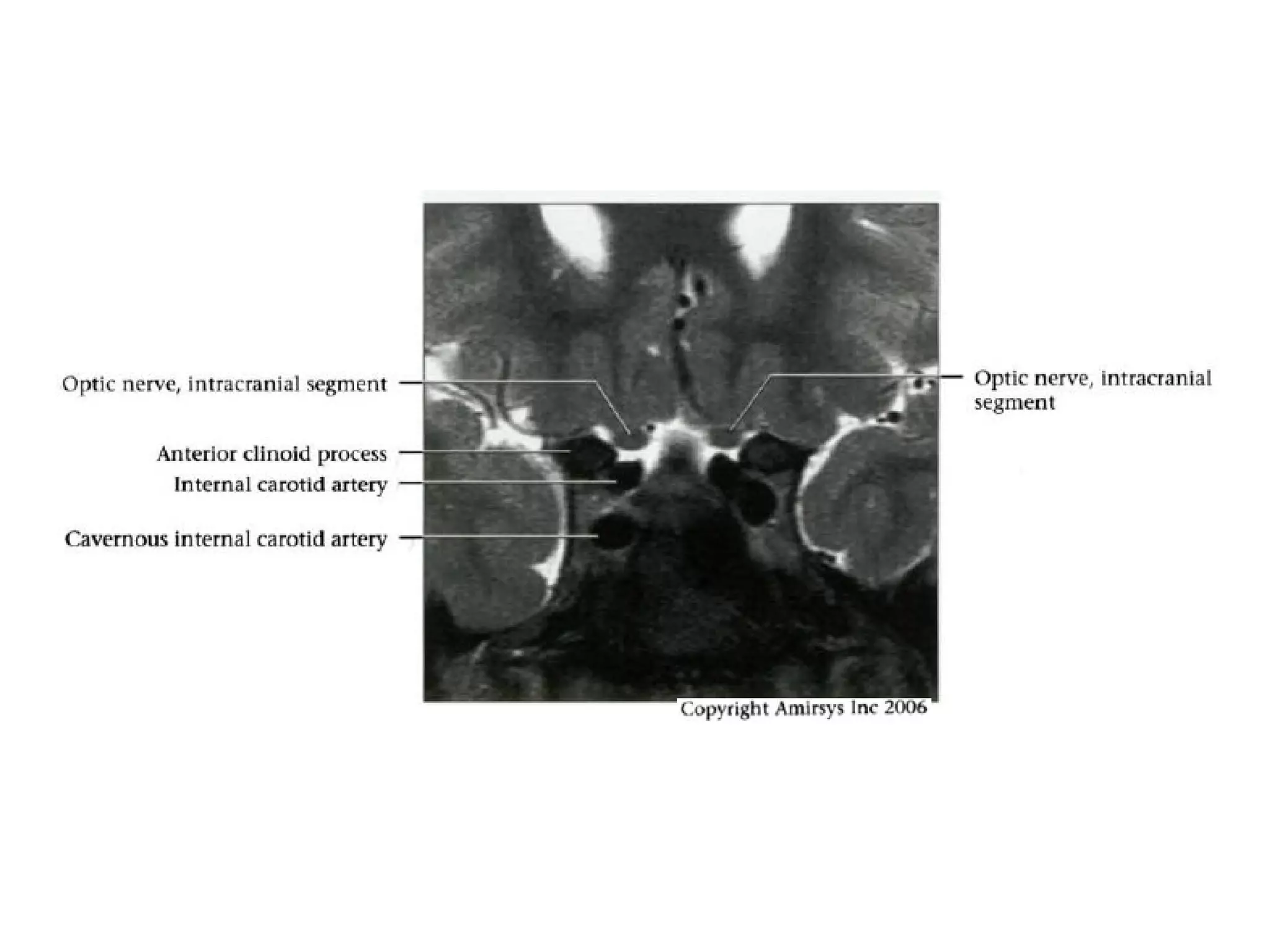
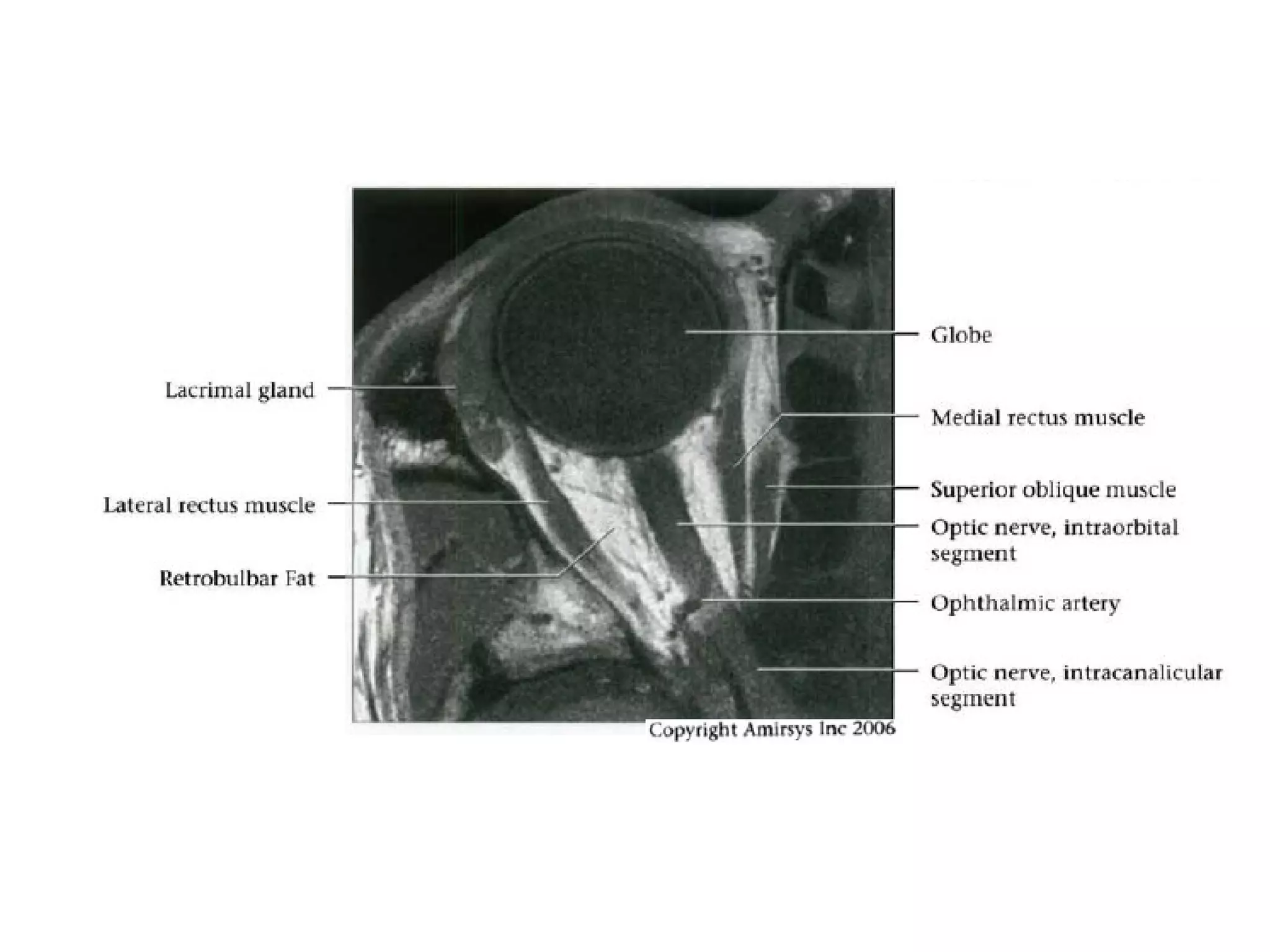
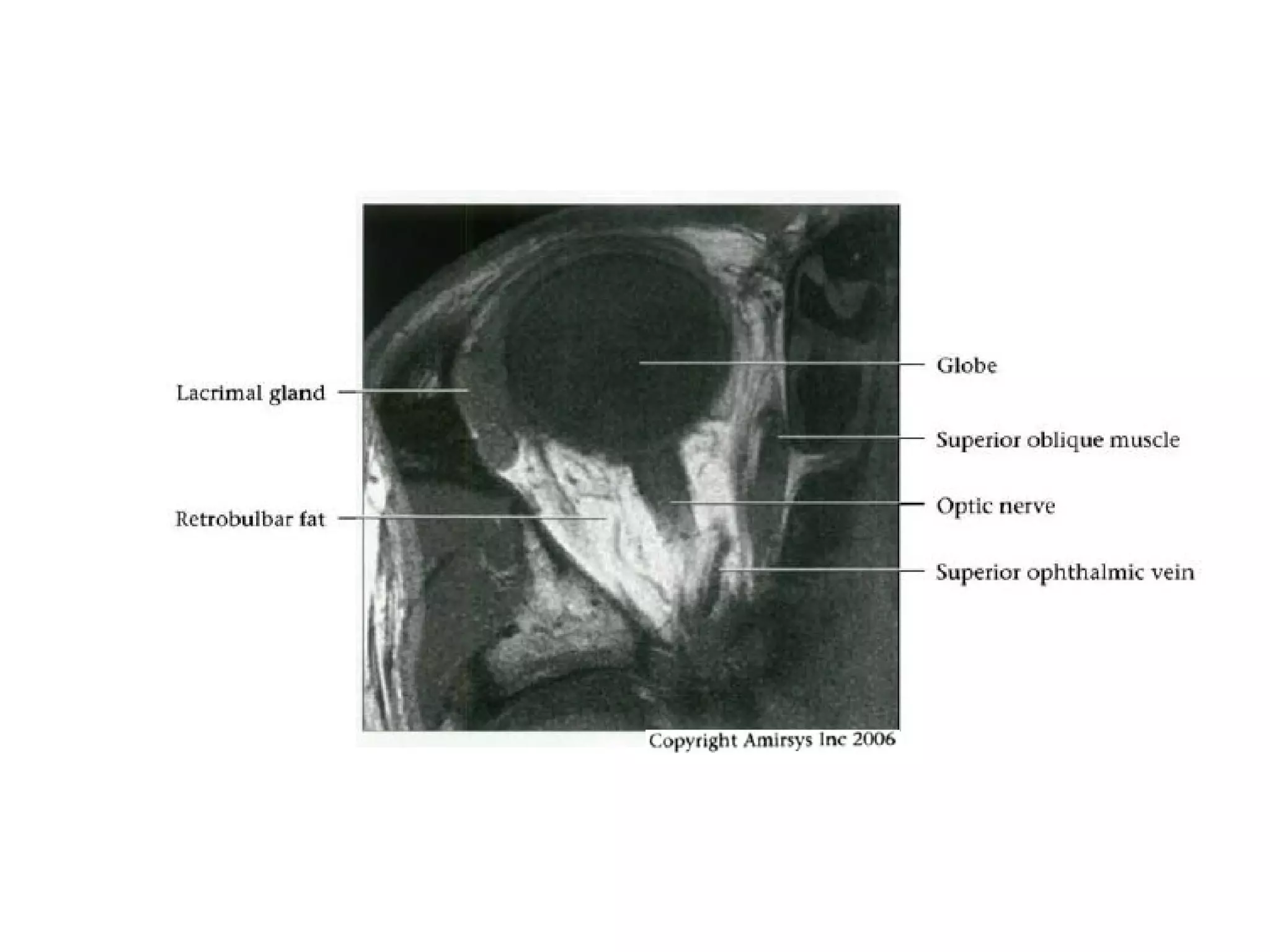
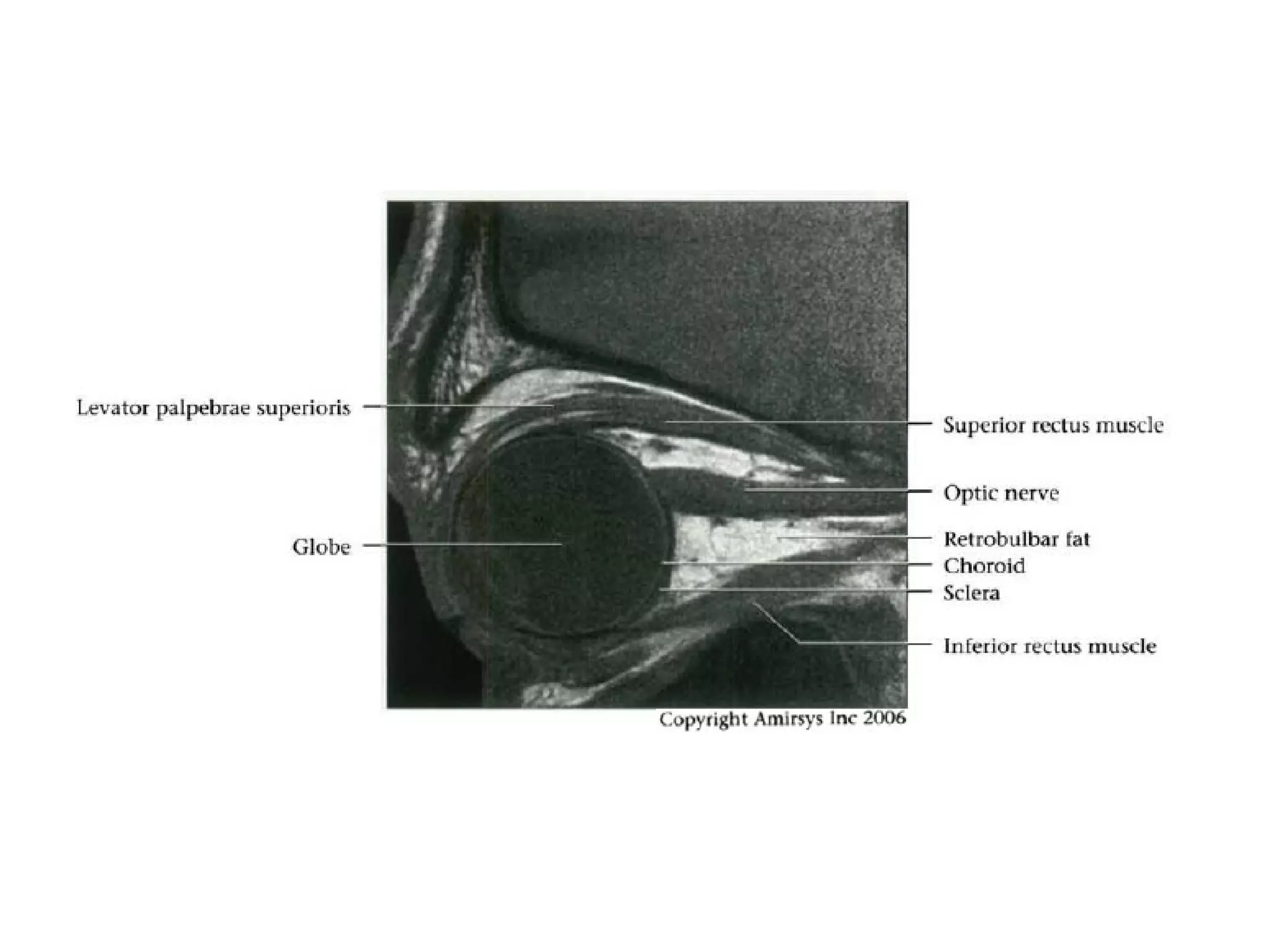
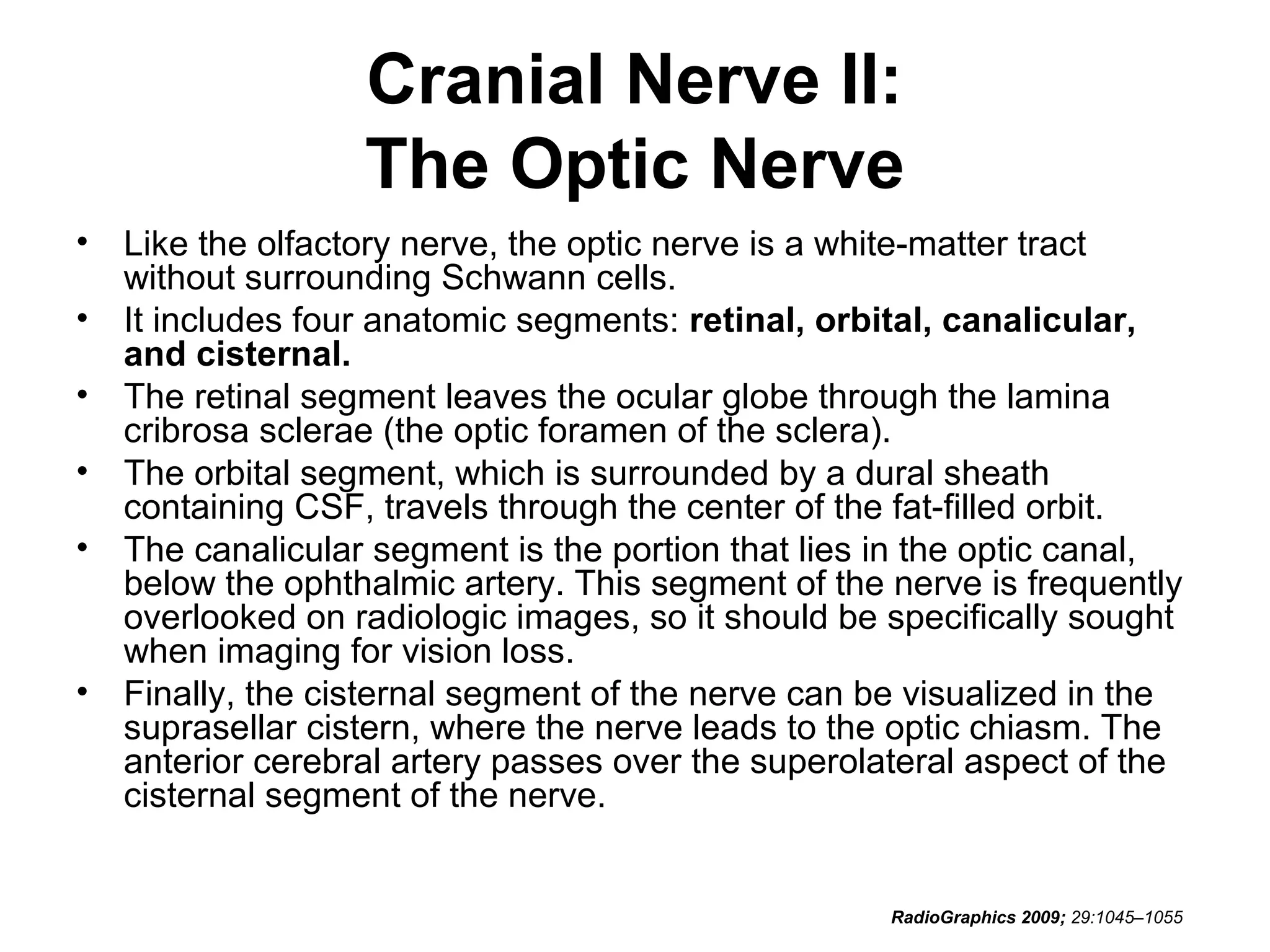
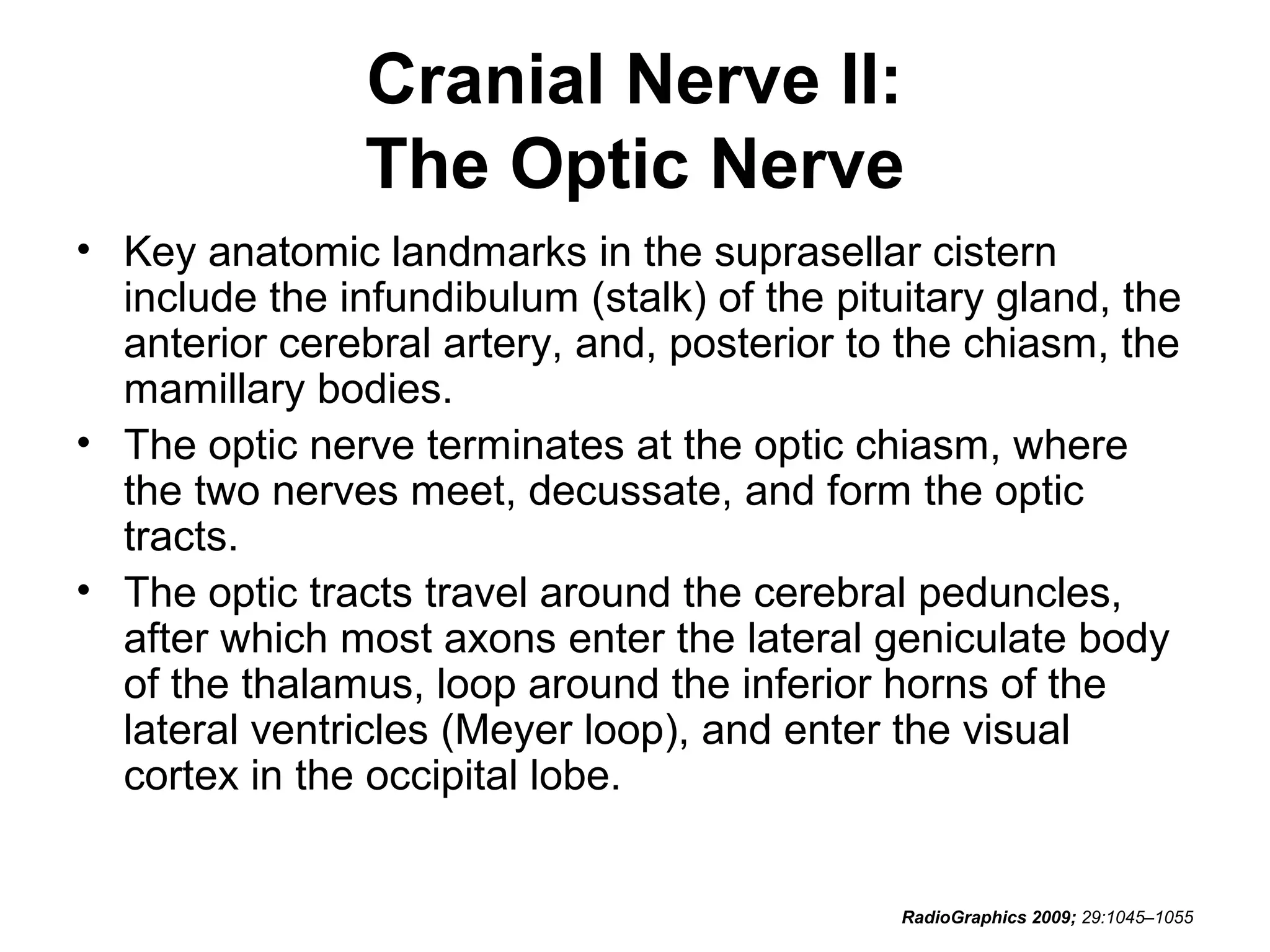
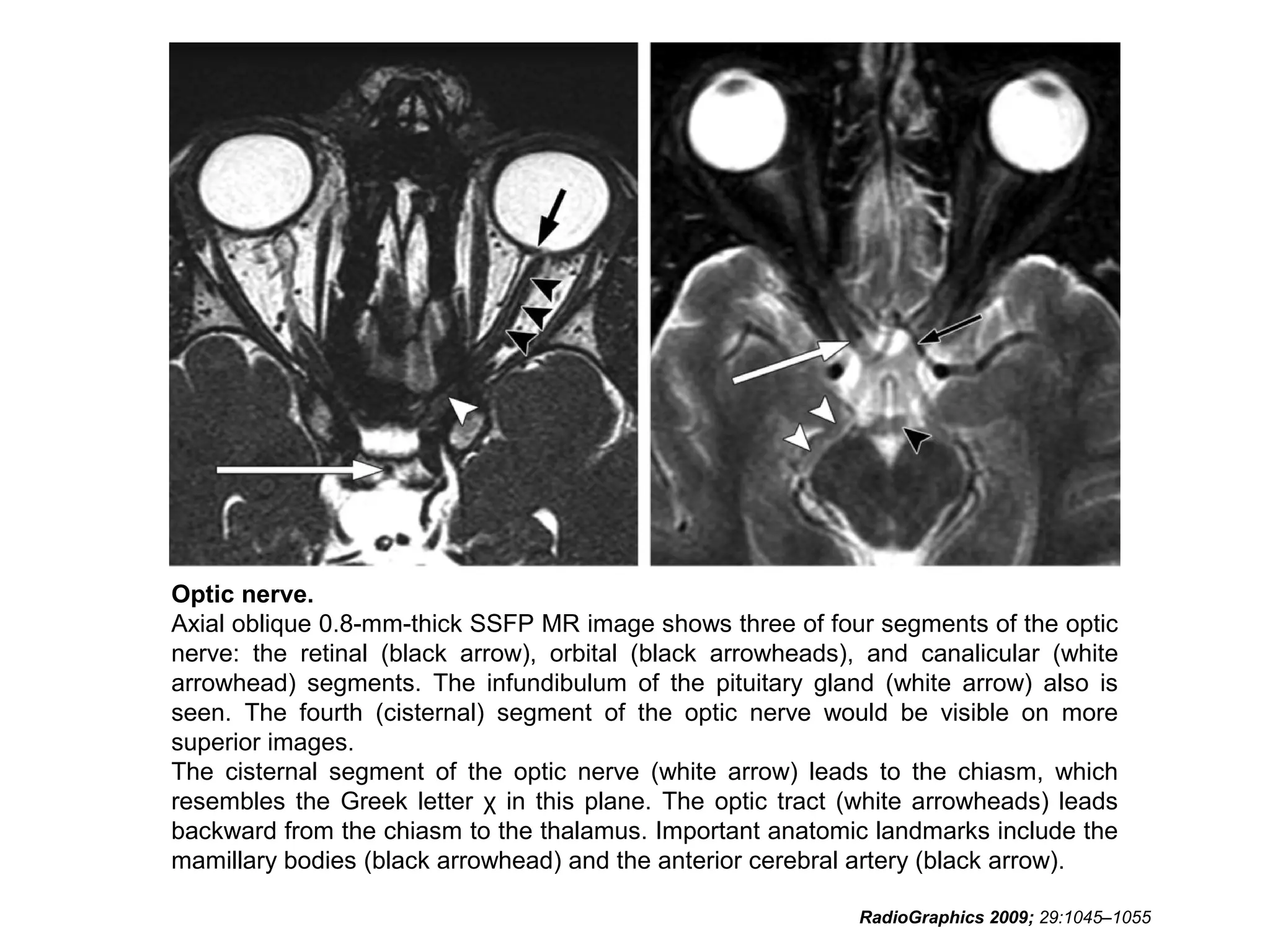
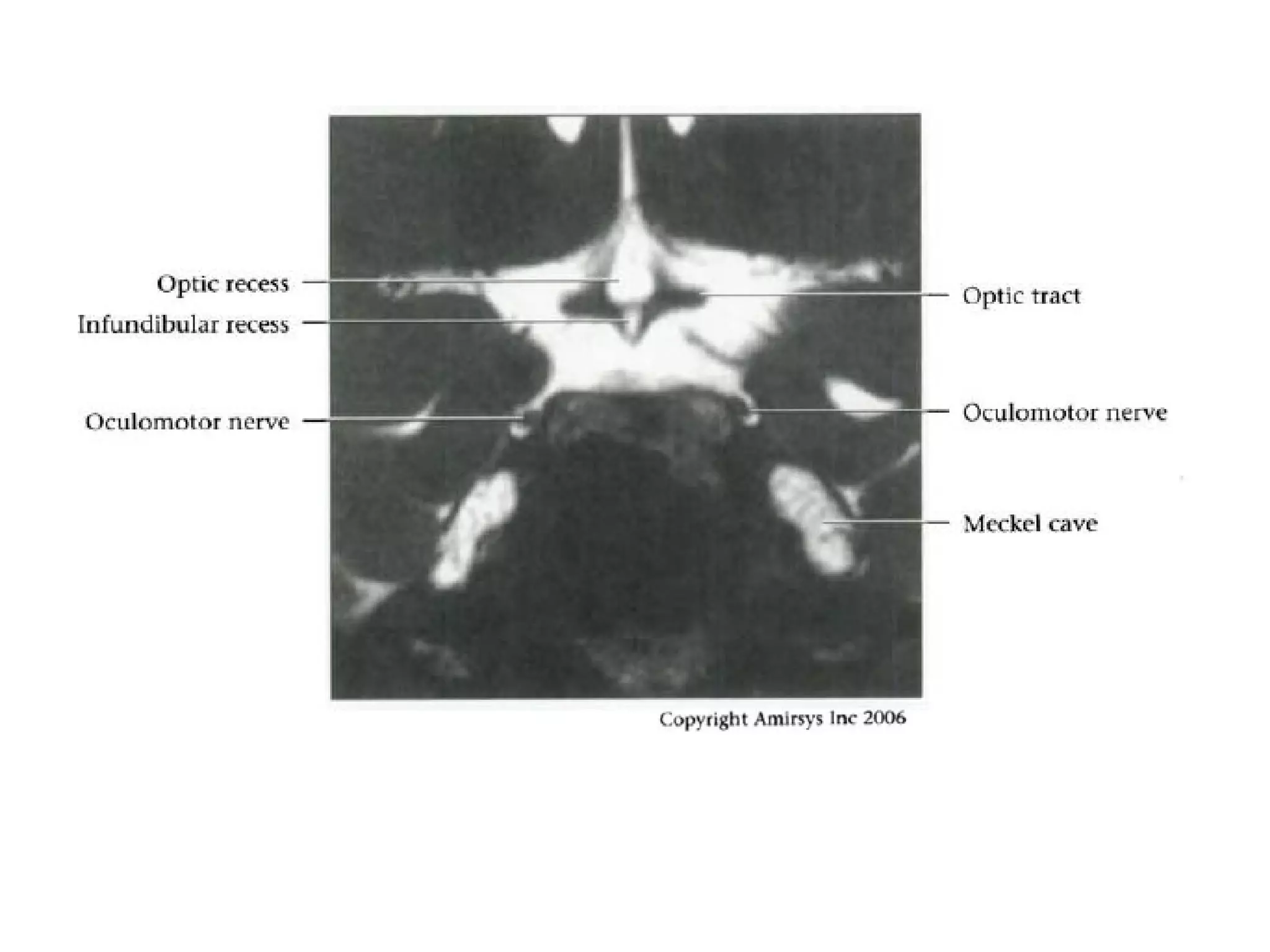
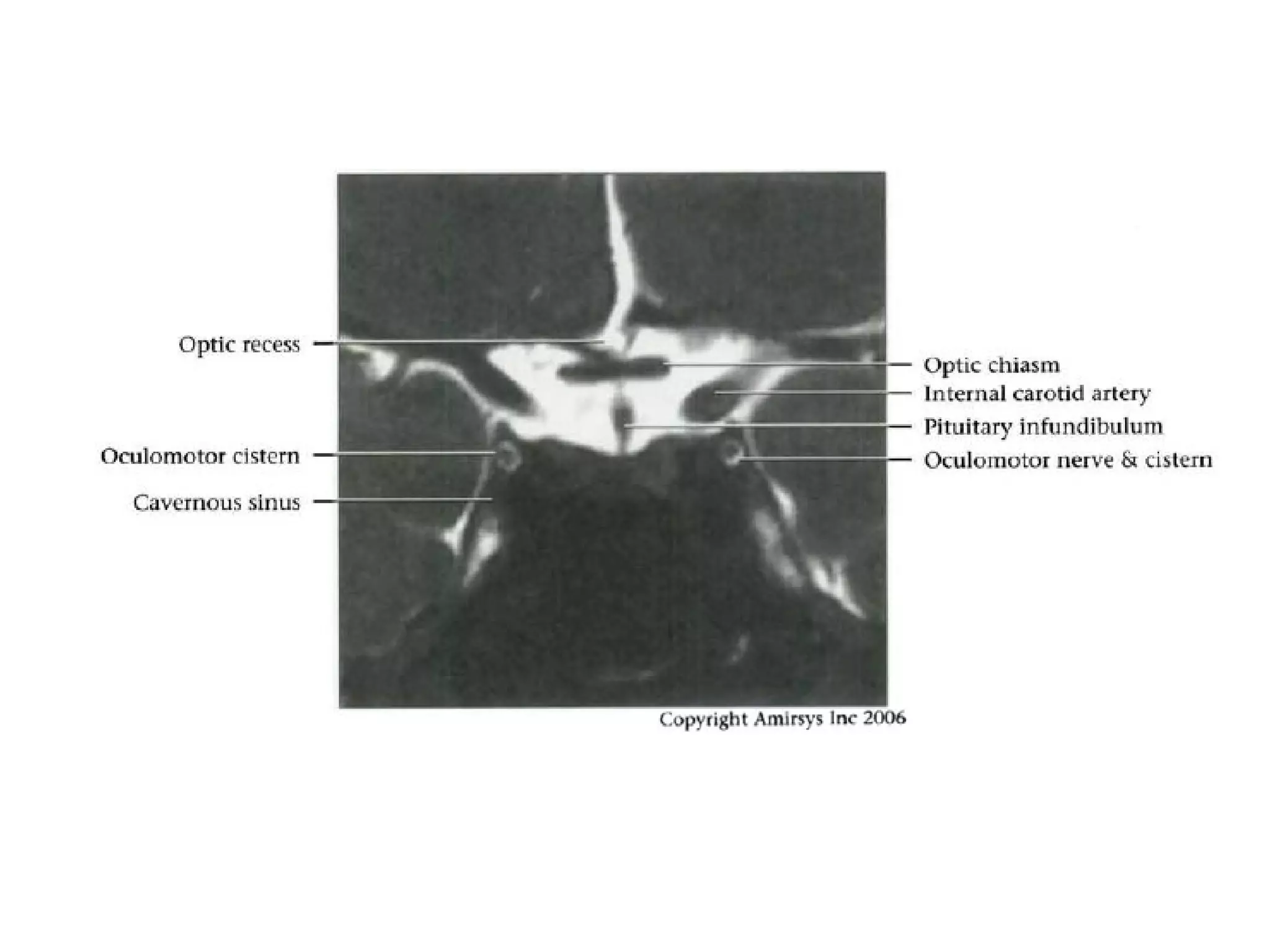
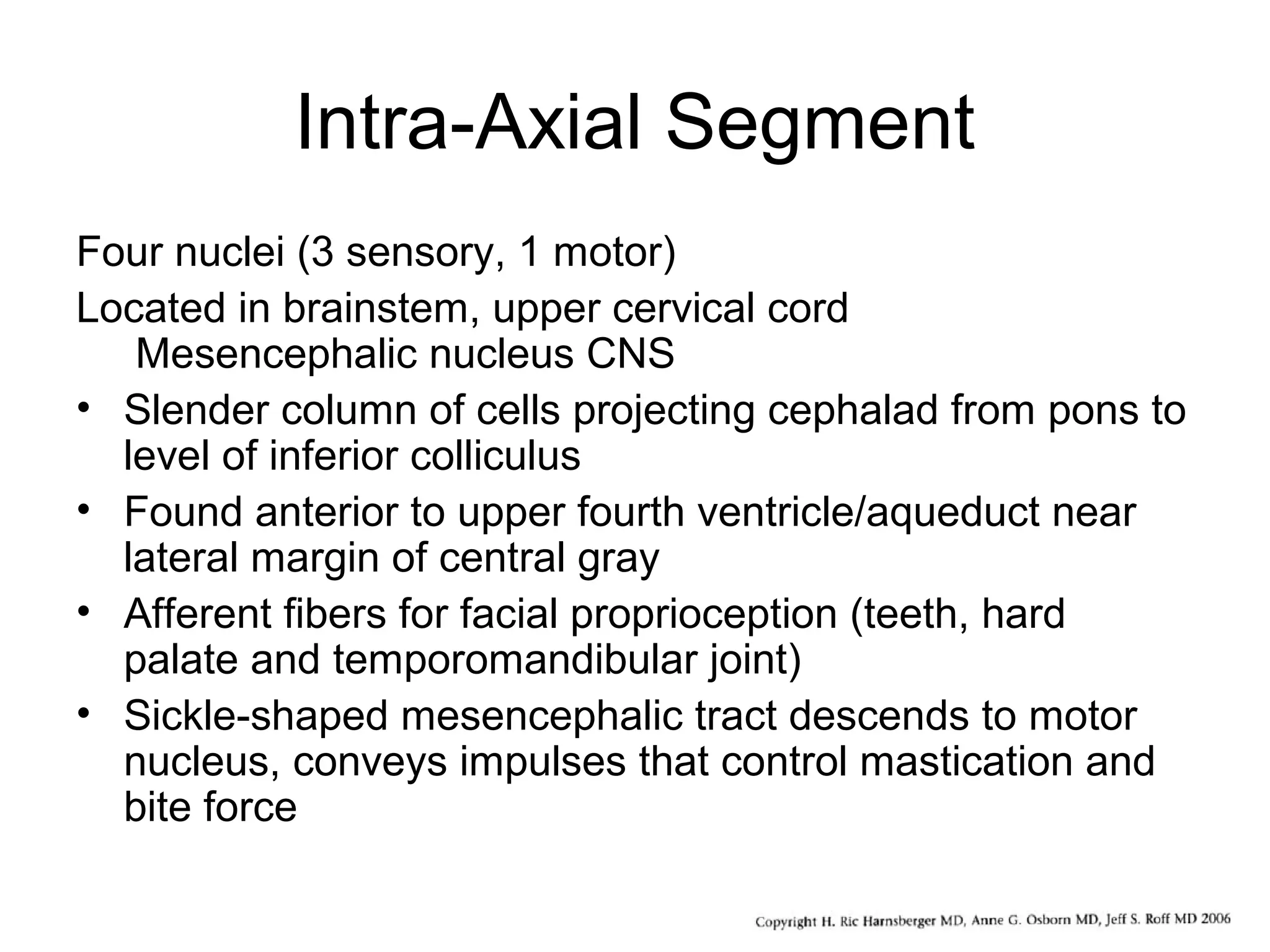
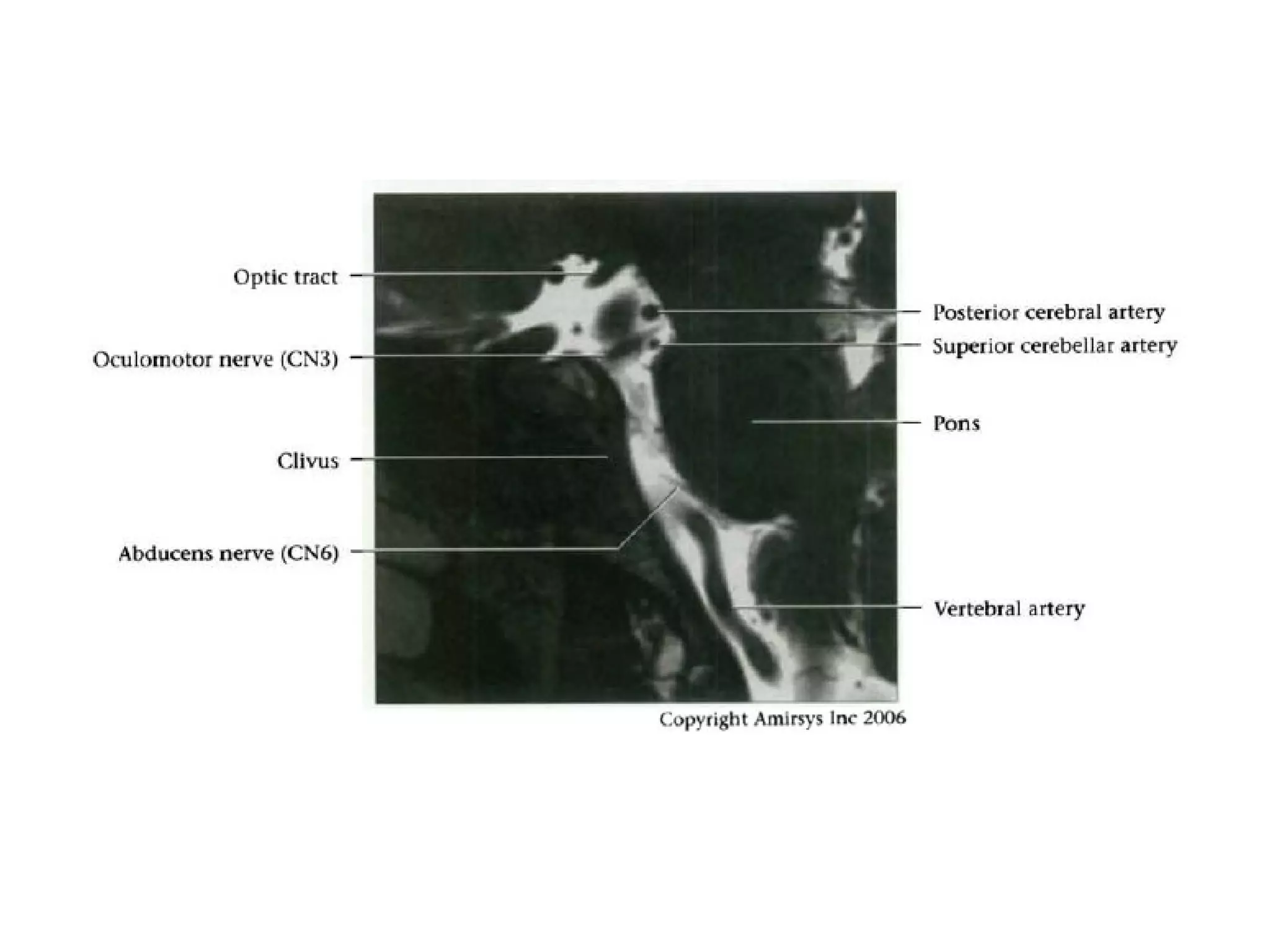
The optic nerve (CN2) is the nerve of sight. It has four segments - intraocular, intraorbital, intracanalicular, and intracranial. In the optic chiasm, nerve fibers from the medial half of each retina cross to the opposite side. From the chiasm, the optic tracts extend posteriorly to terminate in the lateral geniculate bodies of the thalamus, forming connections to the primary visual cortex via the optic radiations.













![References
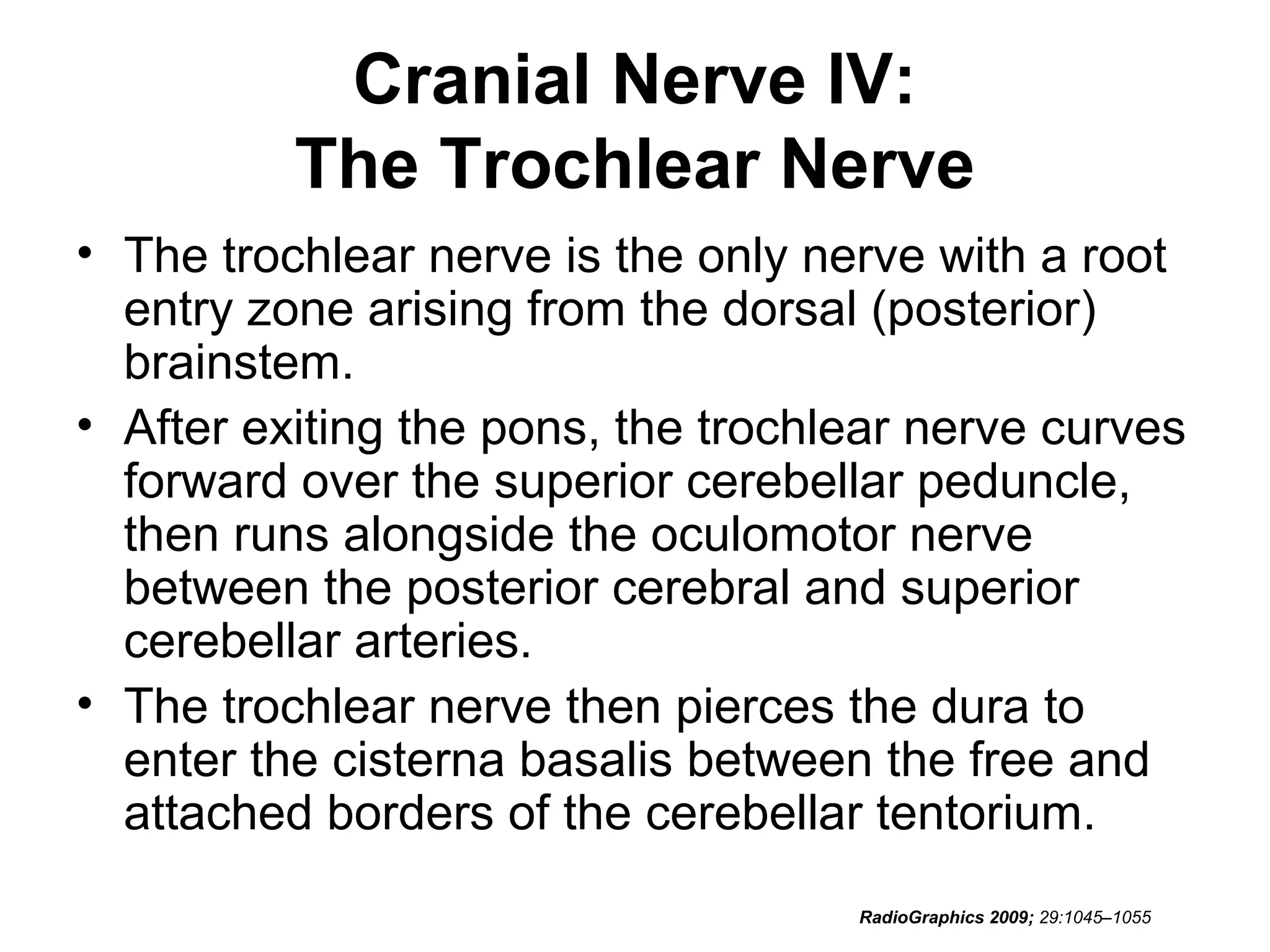
• Diagnostic and Surgical Imaging Anatomy.
Brain, Head & Neck, Spine / H. Ric
Harnsberger. [et al.] ; managing editor, Andre
Macdonald. n 1st ed. I:174-I:259.
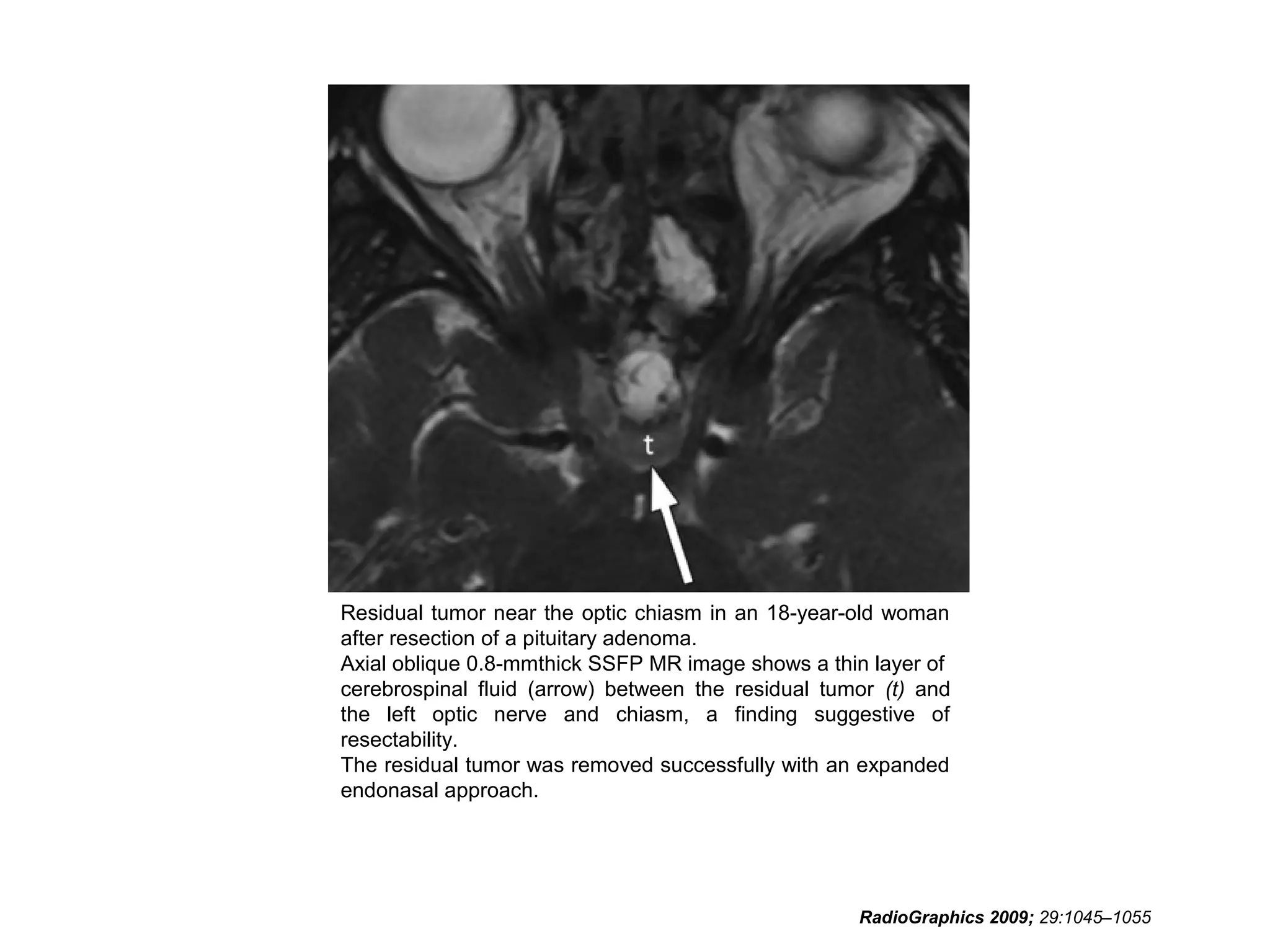
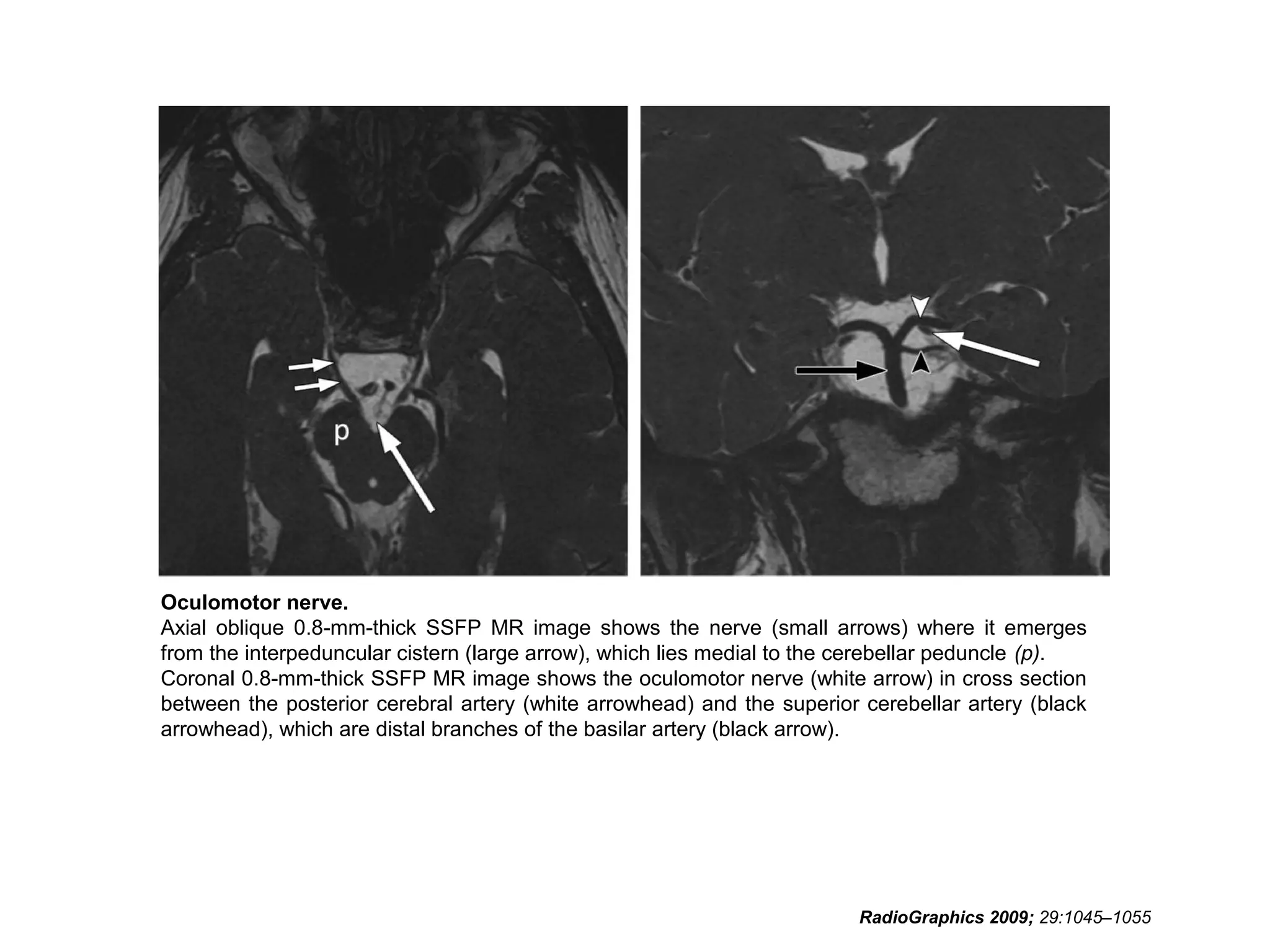
• RadioGraphics 2009; 29:1045–1055 • Sujay
Sheth, BA • Barton F. Branstetter IV, MD •
Edward J. Escott, MD. Appearance of Normal
Cranial Nerves on Steady-State Free
Precession MR Images.](https://image.slidesharecdn.com/cranialnervesparti-131009150807-phpapp01/75/Cranial-nerves-part-1-186-2048.jpg)