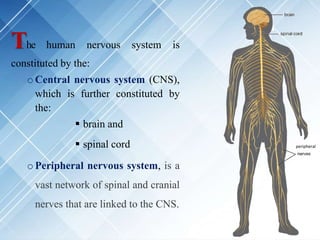
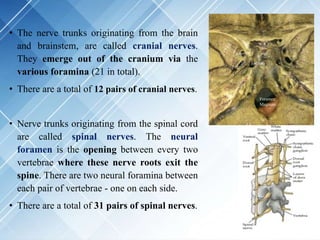
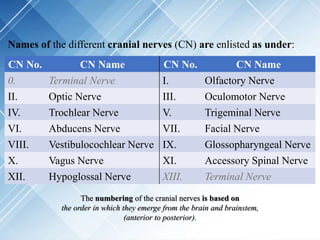
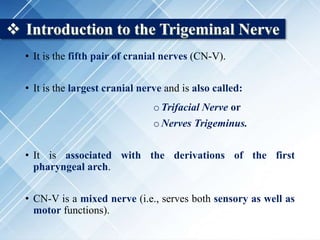
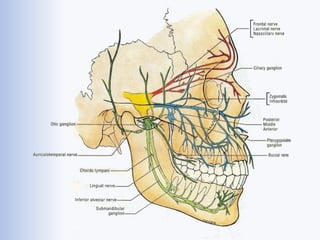
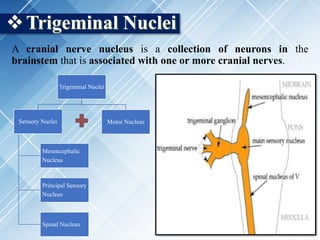
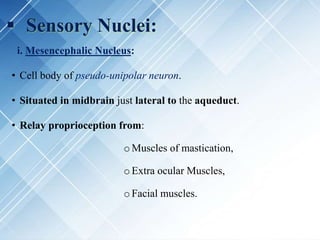
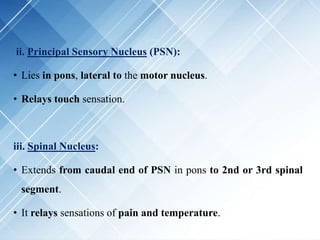
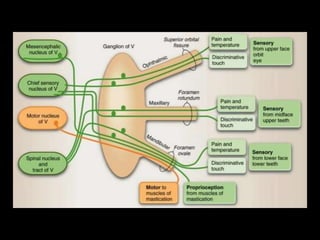
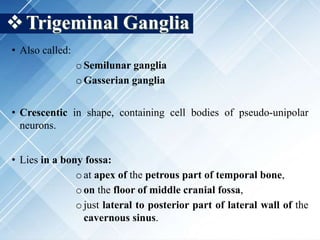
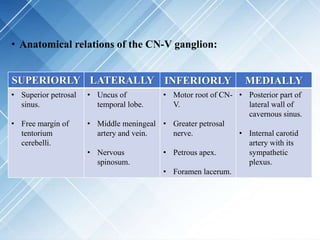
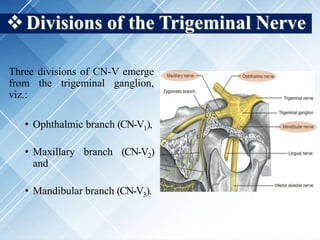
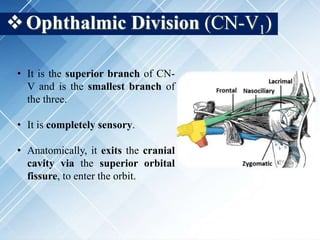
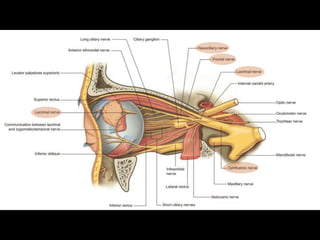
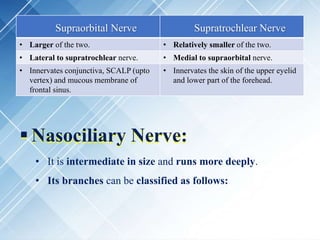
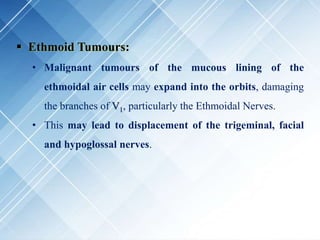
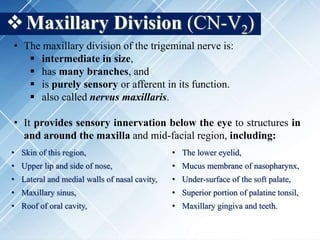
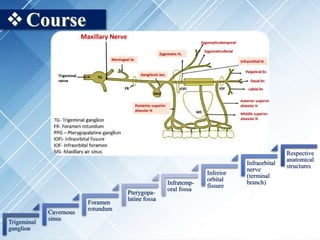
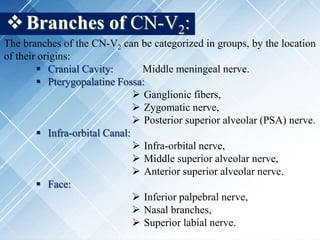
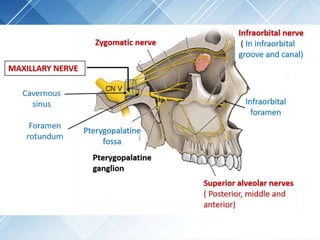
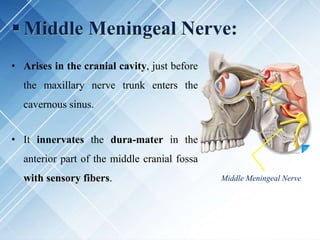
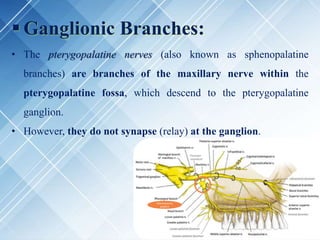
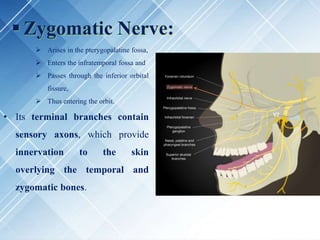
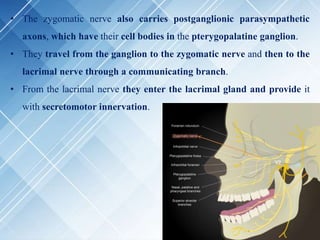
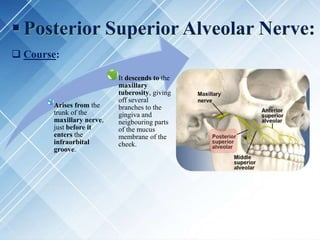
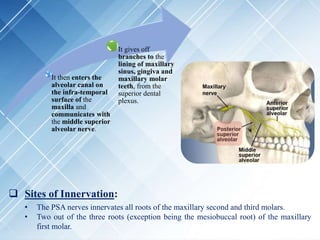
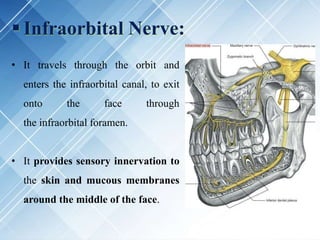
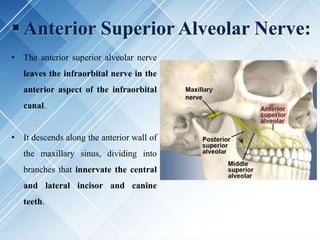
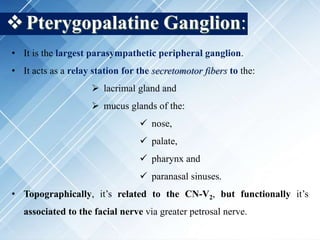
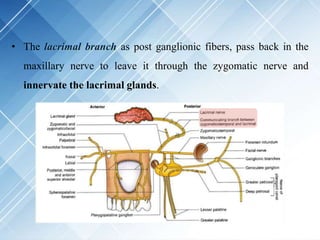
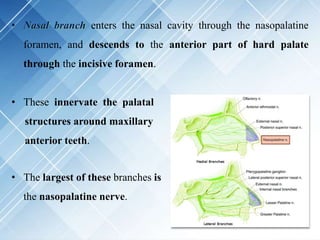
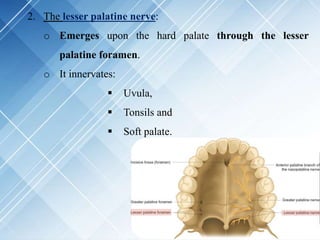
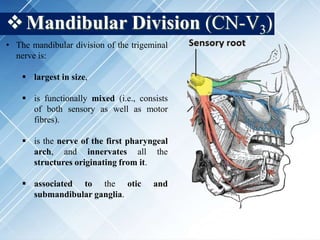
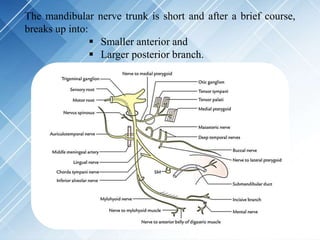
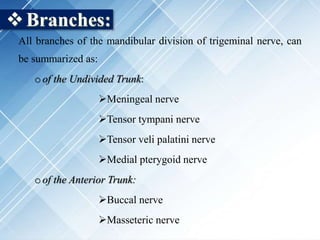
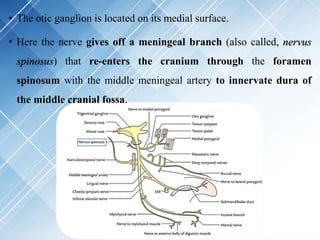
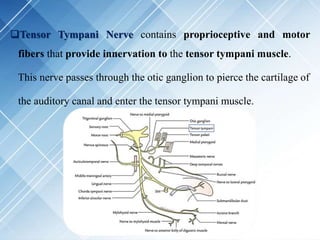
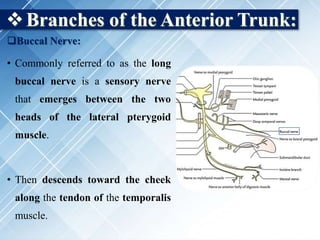
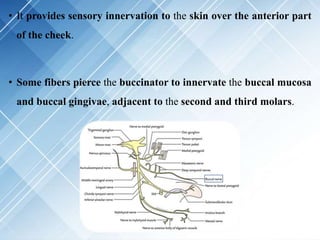
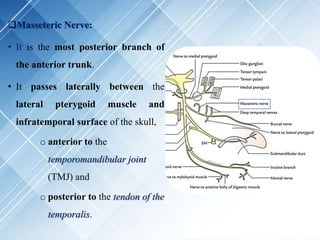
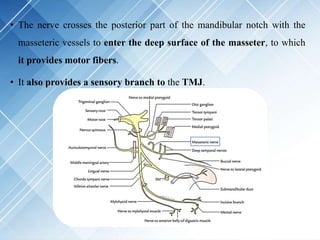
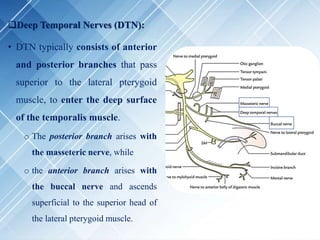
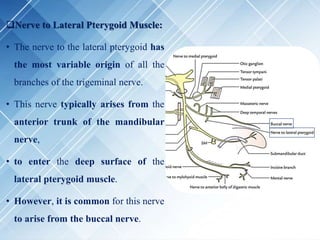
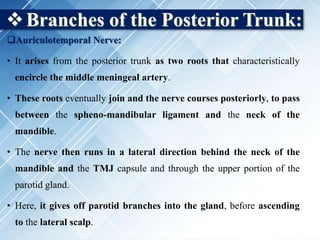
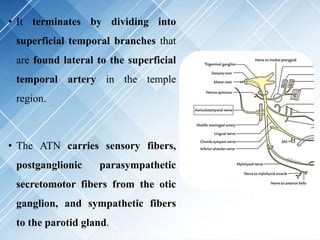
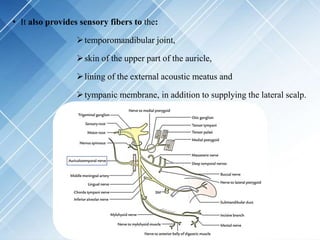
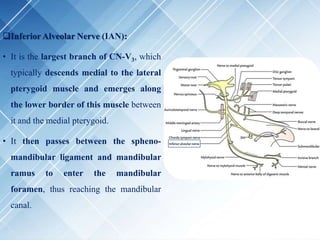
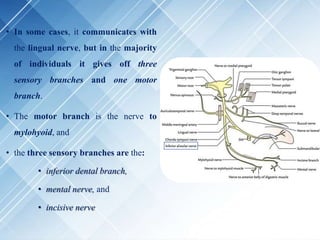
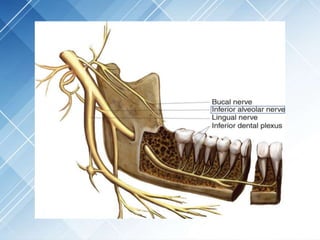
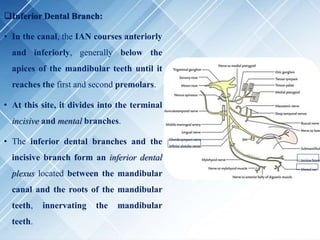
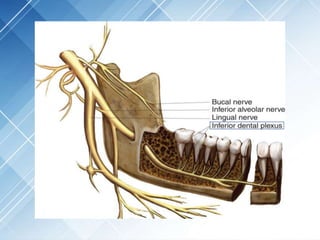
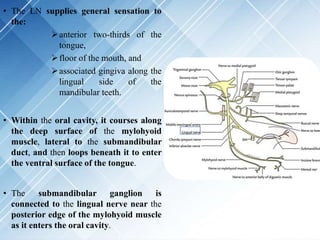
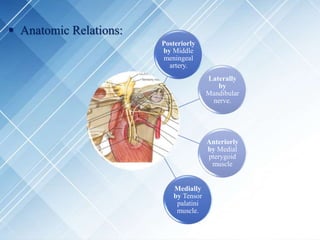
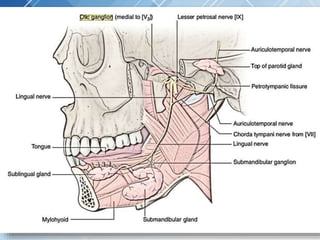
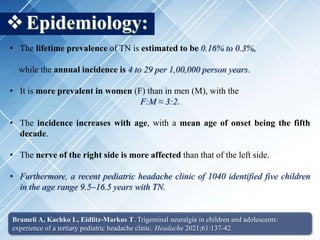
The document provides a comprehensive overview of the trigeminal nerve, including its anatomy, functions, divisions (ophthalmic, maxillary, and mandibular), and clinical significance, particularly in relation to trigeminal neuralgia. It also details the sensory and motor functions associated with each division and highlights relevant clinical aspects and management of conditions related to the nerve. Key anatomical relationships and the role of the trigeminal ganglion in sensory innervation are emphasized.