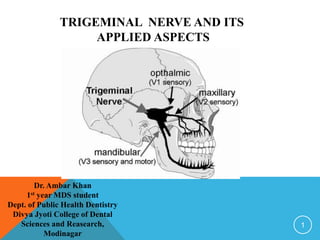
Trigeminal Nerve and its applied aspects
- 1. TRIGEMINAL NERVE AND ITS APPLIED ASPECTS 1 Dr. Ambar Khan 1st year MDS student Dept. of Public Health Dentistry Divya Jyoti College of Dental Sciences and Reasearch, Modinagar
- 2. CONTENTS: • Introduction • Trigeminal nerve • Trigeminal Nuclei • Functional Components • Course and Distribution • Trigeminal ganglion • Divisions of Trigeminal Nerve • Applied Anatomy • Summary • References 2
- 3. INTRODUCTION: CRANIAL NERVES: • Cranial nerves are the nerves that emerge directly from the brain . • Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck. • 12 pairs 1. Olfactory nerve 7. Facial nerve 2. Optic nerve 8. Vestibulocochlear nerve 3. Occulomotor nerve 9. Glossopharyngeal nerve 4. Trochlear nerve 10. Vagus nerve 5. Trigeminal nerve 11. Accessory nerve 6. Abducens nerve 12. Hypoglossal nerve • The cranial nerves are considered as a component of the peripheral nervous system. 3
- 4. 4 CRANIAL NERVES ( I – XII)
- 5. TRIGEMINAL NERVE: Anatomically, the Trigeminal nerve can be studied under the following: • Trigeminal nuclei • Trigeminal ganglion • Trigeminal nerve and its branches 5
- 6. TRIGEMINAL NERVE: • The largest cranial nerve. • It is a mixed nerve; i.e. contains both sensory and motor nerve fibres. • Sensory to – Skin of face Mucosa of cranial viscera Except base of tongue and pharynx • Motor to – Muscles of Mastication Tensor velli palatine, Tensor tympani Anterior belly of digastric Mylohyoid muscle 6
- 8. TRIGEMINAL NUCLEI: • A cranial nerve nucleus is a collection of neurons (grey matter) in the brain stem that is associated with one or more cranial nerves. • Axons carrying information to and from the cranial nerves from a synapse first at these nuclei. • Lesions occurring at these nuclei can lead to effects resembling those symptoms which are seen in severing of the nerve(s) they are associated with. 8
- 9. 1. Mesencephalic nuclie Cell body of Pseudounipolar neuron Relay proprioception from muscles of mastication, Extra ocular muscles, situated in midbrain, just lateral to the Aqueduct. SENSORY NUCLEI: 9
- 11. 2. Principal sensory nucleus (Nucleus principalis nervi trigemini) Lies in Pons lateral to Motor nucleus. Relays touch sensation. 11
- 12. 3. Spinal nucleus Extends from caudal end of principal sensory Nucleus in pons to 2nd or 3rd spinal segment. It relays Pain and Temperature sensation. 12
- 13. MOTOR NUCLEUS: • Innervates muscles of mastication and Tensor tympani and Tensor velli palatine. • Derived from the first Branchial arch. • Located in Pons medial to principle sensory nucleus. 13
- 14. 14
- 15. FUNCTIONAL COMPONENTS: • SENSORY ROOT • MOTOR ROOT 15
- 16. 16
- 17. 17
- 18. 18
- 19. COURSE AND DISTRIBUTION: • Both motor and sensory root are attached ventrally to the junction of pons and middle cerebellar peduncle with motor root lying ventro- medially to the sensory root. • Pass anteriorly in the middle cranial fossa to lie below the Tentorium cerebelli in Cavum trigeminale, here motor root lies inferior to sensory root. 19
- 20. • Sensory root is connected to postero-medial concave border of the Trigeminal ganglion. • Convex antero-lateral margin of the ganglion gives attachment to the 3rd division of the Trigeminal nerve. 20
- 21. • Motor root turns further anterior with sensory component of V3 to emerge out of Foramen ovale as Mandibular nerve. • Opthalmic and Maxillary divisions emerges through Superior orbital fissure and Foramen rotundum respectively. 21
- 22. 22
- 25. THE TRIGEMINAL GANGLION: • SEMILUNAR or GASSERIAN GANGLION. • Cresent in shape with convexity antero-laterally. • Contains cell bodies of pseudounipolar neurons. • LOCATION: lies in a bony fossa at the apex of the petrous temporal bone on the floor of middle cranial fossa, just lateral to the posterior part of lateral wall of the Cavernous sinus. 25
- 26. 26
- 27. • COVERINGS: covered by the dural pouch; i.e. MECKLE’S CAVE or CAVUM TRIGEMINALE, a cave lined by pia and arachnoid mater, thus the ganglion is bathed in CSF. • ARTERIAL SUPPLY: Ganglionic branch of Internal Carotid artery, Middle Meningeal artery and Accessory Meningeal artery 27
- 28. 28 TRIGEMINA L GANGLION LOCATION OF THE TRIGEMINAL GANGLION: At the apex of the petrous temporal bone on the floor of middle cranial fossa
- 29. RELATIONS: • SUPERIORLY: *Superior petrosal sinus *Free margin of Tentorium cerebelli • INFERIORLY: *Motor root *Greater petrosal nerve *Petrous apex *Foramen lacerum • MEDIALLY: *Posterior part of lateral wall of Cavernous sinus *Internal Carotid Artery with its sympathetic plexus • LATERALLY: *Uncus of Temporal lobe *Middle Meningeal artery and vein *Nervous spinosum 29
- 30. 30 RELATIONS OF THE TRIGEMINAL GANGLION:
- 31. DIVISIONS OF TRIGEMINAL NERVE: 1. Ophthalmic nerve 2. Maxillary nerve 3. Mandibular nerve 31
- 32. 32 DIVISIONS OF TRIGEMINAL NERVE
- 34. OPTHALMIC NERVE: • Smallest division • Sensory only • Supplies: Eyeballs, conjunctiva, lacrimal gland, mucosa of nose and paranasal sinuses, skin of forehead, eyelid and nose. 34
- 36. COURSE: Emerges from the Trigeminal ganglion Lateral wall of the Cavernous sinus Gives off 3 branches in the anterior part of the Cavernous sinus Lacrimal, Nasociliary and Frontal Superior Orbital fissure ORBIT 36
- 37. COURSE: 37
- 38. 38 BRANCHES OF OPHTHALMIC NERVE:
- 39. BRANCHES OF OPHTHALMIC NERVE: Gives off 3 branches: • Lacrimal nerve : shortest branch • Frontal nerve : Divides into 1. Supratrochlear nerve 2. Supraorbital nerve • Nasociliary nerve: gives off 5 branches 1. Short ciliary nerve 2. Long ciliary nerve 3. Posterior ethmoidal nerve 4. Infratrochlear nerve 5. Anterior ethmoidal nerve 39
- 40. LACRIMAL NERVE: • Smallest of the 3 branches. • Passes into orbit through lateral compartment of the Superior orbital fissure outside the tendinous ring. • Receives communicating branch from the Trochlear nerve branch of the Ophthalmic nerve. 40
- 41. • Receives branch from Zygomaticotemporal nerve branch of the Maxillary nerve. • Sensory to lateral conjunctiva, upper lid and lacrimal gland. • Post synaptic parasympathetic fibers from Pterygopalatine ganglion to lacrimal gland (parasympathetic secretomotor) 41
- 42. FRONTAL NERVE: • Largest of the 3 branches. • Enters orbit through lateral part of the Superior orbital fissure outside the tendinous ring. • Passes forward between the roof of the orbit and Levator Palpebral Superioris. • Divides midway into : 1. Supratrochlear nerve 2. Supraorbital nerve 42
- 43. S U P R AT R O C H L E A R N E R V E • Smaller nerve • Medial branch • Receives communicating branches from Infratrochlear nerve • Curves around superomedial margin of orbit S U P R A O R B I TA L N E R V E • Larger nerve • Lateral branch • Passes through Supraorbital notch • Divides in medial and lateral branches 43
- 44. S U P R AT R O C H L E A R N E R V E • Supplies : median conjunctiva, upper lid and lower part of the forehead • Lies between the frontalis and corrugator superciliary muscles. S U P R A O R B I TA L N E R V E • Supplies : conjunctiva, scalp upto the vertex, mucous membrane of the frontal sinus. • Lies beneath frontalis muscle. 44
- 45. 45 BRANCHES OF FRONTAL NERVE:
- 46. NASOCILIARY NERVE: • Purely Sensory. • Passes through middle part of the Superior orbital fissure within the tendinous ring. • Runs along medial wall of orbit between Superior oblique and Medial rectus. • Divides into : Anterior Ethmoidal and External Nasal. • Gives off 5 branches in the orbit. 46
- 47. 1. Short Ciliary Nerves : Fibres reach the eyeball and also contain fibres from the ciliary ganglion. 2. Long Ciliary Nerves : 2 or 3 in number. Supplies to the iris and cornea. 3. Posterior Ethmoidal Nerve : Passes through the Posterior ethmoidal foramen to supply the Ethmoid and Sphenoid PNS. 4. Infratrochlear Nerve : Appears on the face above the median angle of the eye. Supplies to the skin of the lacrimal sac and caruncle. 47
- 48. 5. Anterior Ethmoidal Nerve: Larger terminal branch. COURSE: Anterior ethmoidal foramen and canal Into Anterior cranial fossa on superior surface of the cribriform plate Through a slit lateral to the crista galli into the nasal cavity Medial internal nasal branch Lateral internal nasal branch Supplies anterior nasal septum Supplies anterior part of the lateral nasal cavity emerges nasal nerve to the skin of ala, vestibule and tip of nose 48
- 49. 49 BRANCHES OF NASOCILIARY NERVE
- 50. 50 BRANCHES OF OPHTHALMIC NERVE:
- 52. • After leaving the Foramen rotundum, it moves anteriorly in the uppermost part of the pterygopalatine fossa. • As it passes through the pterygopalatine fossa, it also gives branches to shenopalatine ganglion, posterior superior alveolar nerve and zygomatic branches. 52
- 53. • It then moves laterally and moves in a groove on the posterior surface of the maxilla. • Then enters the orbit through the infra orbital fissure and moves through the infra orbital groove where it is called as the Infraorbital nerve and emerges on face from the infraorbital foramen. 53
- 54. 54
- 55. BRANCHES Within cranium In pterygopalatine fossa In infraorbital canal On face MAXILLARY NERVE Middle meningeal nerve Inferior palpebral Lateral nasal Superior labial MSA (middle superior alveolar nerve) ASA (anterior superior alveolar nerve) Zygomati c PSA (posterior superior alveolar) Pterygopalatine Zygomatico temporal zygomatico facial Orbital Nasal Palatine Pharyngeal 55
- 56. • Middle Meningeal nerve: Travels along the middle meningeal artery and provides sensory innervation to the cranial duramater. 56 BRANCHES: In middle cranial fossa (within cranium):
- 57. In Pterygopalatine fossa: 1. Ganglionic branches: Arises as 2 trunks. Trunks join to form single root within the pterygopalatine ganglion. Gives Orbital branches, Palatine branches, Pharyngeal branches and Nasal branches. Gives postganglionic secretomotor fibres to the lacrimal gland via the zygomaticotemporal and lacrimal. 57
- 58. PTERYGOPALATINE NERVE: These are communications between pterygopalatine ganglion & maxillary nerve PTERYGOPALATI NE NERVE
- 59. 1. Orbital branch: Supplies periosteum of orbit 2. Nasal branch: Supplies to mucosa of superior and inferior conchae, posterior ethmoidal sinus and posterior portion of nasal septum. It also includes Nasopalatine branch. It passes across the roof of the nasal cavity downwards and forwards lying between mucosa and periosteum of nasal septum. Reaches to the floor of nasal cavity and give branch to the anterior part of the nasal septum and floor of the nasal cavity. Enters Incisive canal and enters oral cavity through the Incisive foramen It provides sensation to the palatal mucosa of the premaxilla region. 59
- 60. 60 Nasal branch:
- 61. 3 Palatine branch: Arises as Greater Palatine (anterior) and Lesser Palatine (middle and posterior) Greater Palatine nerve descends through pterygopalatine canal from the ganglion and emerges from Greater palatine foramen of the hard palate. Middle palatine and Posterior palatine emerges from the Lesser palatine foramen and supply the soft palate and the tonsillar region respectively. 61
- 63. 5. Pharyngeal branch: It leaves the posterior part of the pterygopalatine ganglion and passes through the pharyngeal canal. It is distributed to the mucous membrane of the nasal part of pharynx, posterior to the Eustachian tube. 63 Pharyngeal branch
- 64. POSTERIOR SUPERIOR ALVEOLAR NERVE: • It arises from the main trunk of the maxillary nerve in the pterygopalatine fossa just before the nerve enters the inferior orbital canal. • Usually arises as 2 trunks. • Passes downwards and crosses the pterygopalatine fossa reaching the infratemporal surface of maxilla. • 1st trunk continues downwards on the posterior surface of maxilla and provides sensory innervation to the buccal gingiva in the maxillary molar region and the adjacent facial mucosal surface. 64
- 65. • 2nd trunk enters maxilla through the PSA canal to travel to the posterolateral wall of maxillary sinus, providing sensory innervation to the sinus mucosa. Continuing downwards, this also provides sensory innervation to the alveoli, PDL and pulp of the molar teeth. 65
- 66. POSTERIOR SUPERIOR ALVEOLAR NERVE POSTERIOR SUPERIOR ALVEOLAR NERVE:
- 67. ZYGOMATIC NERVE: Enters orbit through inferior orbital fissure , It gives 2 branches within inferior orbital fissure ZYGOMATIC NERVE
- 68. ZYGOMATICOTEMPORAL NERVE - Runs along lateral orbital wall - Appears in infratemporal region - Supplies skin of temporal region after piercing temporal fascia 2 cm above the zygoma. - Gives communicating branch to lacrimal nerve. - Supplies parasympethetic Secretomotor fibres to lacrimal gland.
- 69. ZYGOMATICOFACIAL NERVE Appears on face through foramen in the zygomatic bone Supplies the skin over prominence of cheek.
- 70. ZYGOMATIC NERVE: Z Y G O M A T I C O F A C I A L N E R V E • Appears on the face through foramen in the zygomatic bone. • Supplies skin on the prominence of cheek. Z Y G O M A T I C O T E M P O R A L N E R V E • Appears in infratemporal region through foramen in the zygomatic bone. • Supplies skin of temporal region after piercing the temporal fascia 2 cm above the zygoma • Gives communicating branch to the Lacrimal nerve, supplying parasympathetic secretomotor fibres to the lacrimal gland. 70
- 71. 1. Middle Superior Alveolar nerve: • Runs along the lateral wall of maxilla. • Participates in the Superior Dental plexus. • Innervates the premolars 71 IN THE INFRAORBITAL CANAL:
- 72. 2. Anterior Superior Alveolar nerve: Runs in the anterior wall of maxilla = CANALII SINOSUS. It gives off Dental as well as nasal branches. DENTAL BRANCHES NASAL BRANCHES Joins Superior dental plexus Lateral wall of the inferior meatus To supply canines Opening of the maxillary sinus 72
- 73. DENTAL PLUXES
- 74. Anterior superior alveolar nerve ANTERIOR SUPERIOR ALVEOLAR NERVE:
- 75. FACIAL BRANCHES: 1. Inferior Palpebral nerve – pierces Orbicularis oculi and supplies skin of the lower eyelid. 2. Lateral Nasal nerve – supplies skin of the lateral wall, nose and mobile parts of the septum. 3. Superior labial nerve – forms the Infraorbital plexus. Supplies skin and mucous membrane of the upper lip, cheek and the labial glands. 75
- 76. ON FACE 1. INFERIOR PALPEBRAL 2. LATERAL NASAL 3. SUPERIOR LABIAL
- 78. MANDIBULAR NERVE: • Largest branch of the Trigeminal nerve. • Mixed nerve (both sensory and motor) • Nerve of the 1st Branchial arch. 78
- 79. COURSE: 79
- 80. 80
- 81. BRANCHES: • Trunk (undivided) • Nervous spinosus • Nerve to medial pterygoid • Anterior division: • Massetric nerve • Deep temporal nerve • Nerve to lateral pterygoid • Buccal nerve 81
- 82. • Posterior division: • Auriculotemporal nerve • Inferior alveolar nerve • Lingual nerve 82
- 83. BRANCHES FROM THE TRUNK • Before dividing into anterior and posterior division it gives 2 branches during its path of 2-3 mm. • Nervous spinosus or Meningeal branch of Mandibular nerve: • It re-enters the cranial cavity through foramen spinosus along with the middle meningeal artery. • Supply duramater of middle cranial fossa and mastoid air sinus. • Nerve to medial pterygoid: • Supplies medial pterygoid. • Through Otic ganglion without interruption to: 1) Tensor tympani 2) Tensor palitini 83
- 84. BRANCHES FROM THE ANTERIOR DIVISION: The anterior division is significantly smaller than the posterior division. After dividing from the main trunk. It runs anteriorly and below the lateral pterygoid muscle to over its upper border. After this, the nerve is called Buccal nerve. It reaches its external surface by either passing through 2 heads or winding. 1. NERVE TO LATERAL PTERYGOID: It enters the deep surface of the muscle. It may arise as independent branch or may arise in common with the buccal nerve. 84
- 85. 1. MASSETERIC NERVE: Emerges at the upper border of the lateral pterygoid just infront of the TMJ. Passes laterally through mandibular notch along with the masseteric vessels, and enters the deep surface of masseter, also supplies the TMJ. 2. BUCCAL NERVE: is the only sensory branch of anterior division. Travels between 2 heads of the lateral pterygoid and emerges in cheek at the anterior border of the masseter. Supplies skin and mucous membrane of cheek. 3. DEEP TEMPORAL NERVE: These are anterior and posterior deep temporal nerves. Passes between skull, and enters deep surface of the temporalis. Anterior is often a branch of buccal nerve and the posterior branch is placed at the back of the temporal fossa, and sometimes arise in common with the masseteric nerve. 85
- 86. 86
- 88. BRANCHES OF POSTERIOR DIVISION: 1. Auriculotemporal nerve 2. Inferior alveolar nerve 3. Lingual nerve 88
- 89. AURICULOTEMPORAL NERVE: Arises from 2 roots which run backwards and encircle the Middle meningeal artery and form single trunk The trunk passes posterior to the lateral pterygoid between neck of the mandible and the sphenomandibular ligament superior to the 1st part of the maxillary artery Lies behind the TMJ close to the parotid gland. Ascends behind the superficial temporal vessels and then in the temporal region divides into superior temporal branches. 89
- 90. 90 SUPERFICIAL RELATIONS OF THE SPHENOMANDIBULAR LIGAMENT SEEN AFTER THE REMOVAL OF LATERAL PTERYGOID
- 91. BRANCHES OF AURICULOTEMPORAL NERVE: • AURICULAR BRANCHES: Supplies Tragus, upper part of auricle, roof of External auditory meatus, anterosuperior part of tympanic membrane. • SUPERIOR TEMPORAL BRANCHES: Supplies skin of temple. It also gives sensory and secretomotor supply to Parotid gland. • ANTERIOR BRANCHES: Supplies the TMJ. 91
- 92. INFERIOR ALVEOLAR NERVE: • It is a mixed nerve. • Runs vertically downwards medial to lateral pterygoid and lateroposterior to the lingual nerve. Then moves between the Sphenomandibular ligament and medial surface of mandibular ramus. • Enters mandible through mandibular foramen to run in a bony canal below the teeth. 92
- 93. BRANCHES: 1. MYLOHYOID NERVE: Arises just before the nerve enters the mandibular foramen. It pierces the Sphenomandibular ligament along with the mylohyoid muscle and runs in the mylohyoid groove. Supplies to the mylohyoid muscle and anterior belly of digastric. It is also sensory to the skin of inferior and anterior surfaces of the mental protruberance. It may provide sensory innervation to the mandibular incisors. There is also evidence that the mylohyoid nerve supply to the mesial root of the mandibular first molar. 2. BRANCHES TO THE LOWER TEETH AND GINGIVA. 3. MENTAL NERVE: It exits the canal and divides into 3 branches innervating the skin of chin, skin and the mucous membrane of the lower lip. 4. INCISIVE NERVE: It remains within the canal and form a plexus that innervates the pulpal tissue of 1st premolar and incisors through its dental branches. 93
- 95. 95 MANDIBULAR NERVE WITH OTIC GANGLION & ITS CONNECTIONS:
- 96. LINGUAL NERVE: Lies anterior to the Inferior alveolar nerve between the lateral pterygoid and tensor palatini Receives the Chorda tympani branch (SVA) of the Facial nerve Emerges from the Inferior border of the Lateral pterygoid to lie between the ramus and medial pterygoid in the pterygomandibular space Moves downwards and forwards deep to the pterygomandibular raphe between the origins of the superior constrictor and mylohyoid muscles . 96
- 97. Reach to the side of base of the tongue 1cm below and behind 3rd molar just below the mucous membrane of the lateral lingual sulcus Proceeds anteriorly across the muscles of tongue Looping medially and downwards to the Submandibular duct Deep surface of Submandibular gland Breaks into its TERMINAL BRANCHES 97
- 98. 98 COURSE OF THE INFRATEMPORAL NERVE
- 99. BRANCHES OF LINGUAL NERVE AND ITS DISTRIBUTION: 1. Chorda tympani 2. Communications with submandibular ganglion 3. Hypoglossal nerve 99
- 100. 100 RELATIONS OF THE LINGUAL NERVE
- 101. INNERVATION: • Sensory to anterior 2/3rd roof the tongue along with special sensation. • Sensory to floor of the mouth and gingiva on lingual side of the mandible. 101
- 102. GANGLIA ASSOCIATED WITH THE TRIGEMINAL NERVE 102
- 103. 103
- 104. 1. CILIARY GANGLION: • Sensory for orbit 104 CILIARY GANGLION
- 105. 2. PTERYGOPALATINE GANGLION: (Synonym: Ganglion Pterygopalatinum, Meckel's ganglion, Nasal ganglion, Sphenopalatine ganglion) connected to maxillary nerve in infratemporal fossa. Sensory to orbital septum, orbicularis and nasal cavity , maxillary sinus , palate , nasopharynx. 105
- 107. 3. OTIC GANGLION: between trunk of mandibular nerve and tensor palatini supplies post ganglionic Parasympethetic secretomotor fibres to parotid gland. 107 OTIC GANGLION
- 108. 108 RELATIONS OF THE OTIC GANGLION
- 109. related to lingual nerve, rests on the hyoglossus muscle Supplies post ganglionic Parasympethetic secretomotor fibres to submandibular and sublingual gland. 4. SUBMANDIBULAR GANGLION: 109 SUBMANDIBULAR GANGLION
- 110. 5. TRIGEMINAL GANGLION: 110 RELATIONS OF THE TRIGEMINAL GANGLION:
- 111. CUTANEOUS DISTRIBUTION OF TRIGEMINAL NERVE: • Each half of the face is supplied by 13 cutaneous nerves. • 1 motor nerve and 12 sensory nerves • Of the 12 sensory : 11 are from the Trigeminal nerve 1 is c2 Greater Auricular nerve • Branches of Trigeminal nerve: • 5 from the Ophthalmic nerve: 1. Lacrimal nerve 2. Supraorbital nerve 3. Supratrochlear nerve 4. Infratrochlear nerve 5. External nasal nerve 111
- 112. • 3 from the Maxillary nerve: 1. Infraorbital nerve 2. Zygomaticofacial nerve 3. Zygomaticotemporal nerve • 3 from the Mandibular nerve: 1. Buccal nerve 2. Auriculotemporal nerve 3. Mental nerve DIVISIONAL SUPPLY: From lateral canthus to the vertex – Ophthalmic nerve From angle of mouth to the vertex – Mandibular nerve Between the 2 areas – Maxillary nerve 112
- 113. 113 CUTANEOUS DISTRIBUTION OF TRIGEMINAL NERVE
- 115. 115
- 116. 116
- 117. 117
- 118. 118
- 119. • Motor function: • Test the patient’s ability to chew and work against resistance and observe contraction of the massater and temporal muscles by visual examination and digital palpation. 119
- 120. PURPOSE OF TEST: 1. Is there any loss of sensation ???? 2. Where the lesion is present ???? - Peripheral branches - Gasserian ganglion 120
- 121. VARIOUS TECHNIQUES OF NERVE BLOCKS 121
- 122. Nerves anaesthetized : • Anterior superior alveolar nerve • Middle superior alveolar nerve • Infraorbital nerve a) Inferior palpebral b) Lateral nasal c) Superior labial LANDMARKS: Supraorbital ridge, infraorbital ridge, infraorbital notch, infraorbital depression, pupils of the eye, Upper 2 premolar or anterior teeth. 122 INFRAORBITAL NERVE BLOCK: AREAS ANAESTHETIZED BY INRAORBITAL NERVE BLOCK
- 123. • Assume 10 o’clock position for the right and left infraorbital nerve block. • Patient position – supine or semisupine • Prepare the tissue at the height of the mucobuccal fold (usually above the lateral incisor) • Retract the lip and insert the needle to the upper rim of the infraorbital foramen. • Insert the needle slowly. • Aspirate slowly. • Deposit and withdraw the needle. 123 TECHNIQUE: INFRAORBITAL NERVE BLOCK
- 124. COMPLICATIONS: • Uncontrolled or prolonged bleeding • Infection at the site of block • Artery or vein injury • Unintentional injection of the anaesthetic into artery or vein • Haematoma formation – Though rare, identified by discoloration of the skin below the lower eyelid. • Nerve damage • Edema 124
- 125. Nerves anaesthetized : • Nasopalatine nerve during its path as it emerges from the anterior palatine foramen, located on the anterior palate in the midline. LANDMARKS: maxillary central incisor teeth, Incisive papilla in the midline of the hard palate, location posterior to the middle of maxillary central incisors. 125 NASOPALATINE NERVE BLOCK: AREAS ANAESTHETIZED BY NASOPALATINE NERVE BLOCK
- 126. • A 25 or 27 gauge short is recommended. • AREA OF INSERTION: Palatal mucosa just lateral to the incisive papilla. • Approach the incisive papilla at a 45 degree angle with the orientation of the bevel towards the palatal tissue. • Clean and dry the tissue with gauze. • Apply topical anesthetic lateral to the incisive papilla for 2 min. After 2 min move the cotton applicator directly on the papilla. • Apply sufficient pressure so that there is blanching. Place the bevel of the needle against the blanched soft tissue at the injection site. 126 TECHNIQUE: NASOPALATINE NERVE BLOCK
- 127. • Direct the syringe into the mouth from the opposite side of the mouth at the injection site at a right angle to the target area with orientation of the needle bevel toward the palatal soft tissue. • Place the bevel of needle gently against the blanched tissue and apply enough pressure to slightly bow the needle. • Deposit a small amount of LA. • Slowly advance the needle approximately 8mm until palatine bone is contacted. • Withdraw 1mm and aspirate. • If negative, inject LA over 30 sec. • Withdraw the needle and recap. • Wait 2-3 min before starting the treatment. 127
- 128. COMPLICATIONS: • Palatal ischemia and necrosis of soft tissue • Haematoma formation is possible. • Some patients may be uncomfortable if their soft palate becomes anaesthesized. • Infection at the site of block • Nerve damage 128
- 129. Nerves anaesthetized : • Anterior superior alveolar nerve or the Greater palatine nerve as it leaves the Greater palatine foramen. LANDMARKS: Second and third molars, Gingival margin of the 2nd and 3rd maxillary molars on palatal side, midline of the palate, a point 1cm away from the palatal gingival margin toward the midline of palate 129 GREATER PALATINE (ASA) NERVE BLOCK: AREAS ANAESTHETIZED BY GREATER PALATINE NERVE BLOCK
- 130. • A 25 or 27 gauge short is recommended. • Locate the Greater palatine foramen. • Approach the incisive papilla at a 45 degree angle with the orientation of the bevel towards the palatal tissue. • Prepare the tissue at the injection site, 1-2 mm anterior to the Greater palatine foramen. • Clean and dry the tissue with gauze. • Apply topical anesthetic with a cotton applicator for 2 min. • Move the cotton applicator posteriorly so that it is directly over the GP foramen and supply sufficient pressure to blanch the tissue for 30 sec. 130 TECHNIQUE: GREATER PALATINE NERVE BLOCK
- 131. • Apply enough pressure to slowly bow the needle. Deposit a small amount of anaesthetic. • Straighten the needle and penetrate the tissue with the needle. • Continue to apply pressure with the cotton applicator while injecting, • Slowly advance the needle towards the incisive foramen while injecting until the bone is contacted (about 5mm) • Withdraw the needle 1mm and aspirate. If negative, slowly deposit the LA. • Slowly remove the needle and recap. • Wait for 2-3 min before starting the treatment. 131
- 132. COMPLICATIONS: • Ischemia and necrosis of soft tissue, when highly concentrated vasoconstricting solution is used for homeostasis over a prolonged period of time. • Some patients may be uncomfortable if their soft palte becomes anaesthesized. • Infection at the site of block • Nerve damage • Needle breakage 132
- 133. Nerves anaesthetized: Posterior superior alveolar nerve Areas anaesthetized: • Maxillary molar (except mesiobuccal root of first molar) • Buccal alveolar bone and soft tissues • Lining of the maxillary sinus corresponding to the molar teeth LANDMARKS: Mucobuccal fold, Zygomatic process of maxilla, Infra temporal surface of maxilla, Anterior border and coronoid process of the ramus of the mandible, maxillary tuberosity. 133 POSTERIOR SUPERIOR ALVEOLAR NERVE BLOCK: AREAS ANAESTHETIZED BY POSTERIOR SUPERIOR ALVEOLAR NERVE BLOCK
- 134. • Assume 10 o’clock position for the right and left PSA nerve block. • 25 gauge short needle is recommended. • Patient position: Supine or semi supine. • Prepare the tissue at the height of the mucobuccal fold above the maxillary 2nd molar. • Target area is the PSA nerve which is posteior, superior and medial to the posterior border of the maxilla. 134 TECHNIQUE: POSTERIOR SUPERIOR ALVEOLAR NERVE BLOCK
- 135. • Ask the patient to keep their mouth halfway open as it provides better accessibility. • Retract the patient’s cheek. Pull the tissues at the injection site taut. • Insert the needle slowly in an upward, backward and inward direction. • Aspirate • Deposit and withdraw the needle. 135
- 136. COMPLICATIONS: • Haematoma formation: commonly produced by inserting the needle too far posteriorly into the Pterygoid plexus of veins. In addition, the maxillary artery may be perforated. Use of a short needle minimizes the risk of pterygoid plexus puncture • Mandibular anaesthesia: The mandibular division (V3) of the Trigeminal nerve is located lateral to the PSA nerve. Deposition of LA lateral to the desired location may produce varying degrees of mandibular anesthesia. • Trauma to lateral and medial pterygoid muscles, leading to trismus. 136
- 137. Nerves anaesthetized : • Inferior alveolar nerve • Mental nerve • Lingual nerve • Incisive nerve LANDMARKS: Mucobuccal fold and its concavity, Zygomatic process of the maxilla, infratemporal surface of the maxilla, anterior border and coronoid process of the ramus of the mandible, maxillary tuberosity 137 INFERIOR ALVEOLAR NERVE BLOCK: AREAS ANAESTHETIZED BY INFERIOR ALVEOLAR NERVE BLOCK
- 138. • Assume 8 o’clock position for the right and left IANB nerve block. • Patient position – supine or semisupine • A 25 gauge long needle is recommended for adult patient. • AREA OF INSERTION: Medial ramus, mid-coronoid notch. • Level with the occlusal plane (1cm above) • ¾ posterior from the coronoid notch to pteryomandibular raphe • Advance to bone (20-25mm) 138 TECHNIQUE: INFERIOR ALVEOLAR NERVE BLOCK
- 139. COMPLICATIONS: • Transient hemifacial paralysis: The muscles being supplied by that side of the facial nerve are affected and cannot contract. • Occurs due to accidental nerve injury to the Facial nerve while giving IANB nerve block. • This results in the loss of muscle action of the affected side of the face. • The eyelids cannot be closed by the patient. • Loss of maintaining of the lip position on the affected side and drooping of the lips on the affected side. 139
- 141. • Muscle trismus: It is due to muscle spasm caused when the injection is given into the medial pterygoid muscle causing tearing of the muscle fibres. It is called as Medial pterygoid trismus or Myospasm. • Haematoma: It is caused when there is an accidental injection to the blood vessels. • Mucosal irritation • Infection at the injection site • Needle breakage. 141
- 142. Nerve to be anaesthetized : Long Buccal nerve LANDMARKS: Retromolar triangle, between the internal and external oblique ridge of the mandible. 142 LONG BUCCAL NERVE BLOCK: AREAS ANAESTHETIZED BY LONG BUCCAL NERVE BLOCK
- 143. • 25 to 27 gauge long needle is recommended. • AREA OF INSERTION: Apex of the retromolar triangle between the external and internal oblique ridges. • DIRECTION OF INJECTION : Parallel to the occlusal plane from the same side. • 0.2 ml of anaesthetic solution is deposited at the apex of the retromolar triangle between the external and internal oblique ridge. 143 TECHNIQUE: LONG BUCCAL NERVE BLOCK
- 144. COMPLICATIONS: • Needle induced nerve damage, resulting in paraesthesia • Haematoma formation leading to trismus • Needle breakage (rare) 144
- 145. 145 APPLIED ANATOMY
- 146. 1. TRIGEMINAL NEURALGIA – TIC DOULOUREX DEFINITION: Sudden, usually unilateral, severe, brief, stabbing, lancinating, recurring pain the distribution of one or more branches of the Trigeminal (vth) nerve. 146
- 147. TRIGEMINAL NEURALGIA – TIC DOULOUREUX • Relatively common • Paroxysm of sudden intense, shocking, stabbing onset of facial pain. • Involves one or more areas of distribution of the Trigeminal nerve. • Maxillary and Mandibular divisions are commonly involved. 147
- 148. CLINICAL FEATURES: Symptoms may include one or more of these features: • Episodes of severe, shooting or jabbing pain that may feel like an electric shock. • Spontaneous attacks of pain or attacks triggered by daily activities like touching the face, chewing, speaking or brushing teeth. • Bouts of pain lasting from a few seconds to several minutes. • Episodes of several attacks lasting a few days, weeks, months or longer – some people have periods when they experience no pain. • Constant burning feeling or aches that may occur before it evolves into the spasm-like pain. 148
- 149. • Pain in the areas supplied by the Trigeminal nerve, including the cheek, jaw, teeth, gums, lips, or less often the eye and forehead. • Pain affecting one side of the face at a time, though may rarely affect both sides of the face. • Pain focused in one spot or spread in a wider pattern. • Attacks that become more frequent and intense overtime. 149
- 150. Local lesions- Ophthalmic division : Acute glaucoma Frontal sinusitis Maxillary division : Caries Carcinoma of maxilla Empyema of maxillary sinus Mandibular division : Caries Carcinoma or ulcer of the tongue TRIGGER ZONES 150
- 151. 151
- 152. MEDICATION: Medications used to treat trigeminal neuralgia are those used for many other nerve pain syndromes—drugs originally designed to treat seizures. These anti seizure agents suppress or entirely block the pain signals that the trigeminal nerve sends to your brain. Carbamazepine is to be used as the first-line treatment. Second line drug treatment is the alternative if carbamazepine is contraindicated or not tolerated 152
- 153. Second-line drug treatments: Gabapentin Phenytoin Lamotrigine Oxy carbamazepine Topiramate Baclofen(Antispasmodic) Tricyclic antidepressants like Amitriptyline and Imipramine 153
- 154. Carbamazepine: Carbamazepine is to be used as the first-line treatment. Start with a low dose and titrate slowly upwards until pain settles or adverse effects limit further dose increases: For carbamazepine, start with 100 mg daily and titrate by 100–200 mg every 1–2 weeks. A dose of 200 mg three or four times a day is commonly needed, although a maximum of 1600 mg per day can be used. While using carbamazepine always check for potential drug interactions Carbamazepine induces liver microsomal enzymes and interacts with many drugs (e.g. oral contraceptives). 154
- 155. The adverse effects like diplopia, headache, nausea, and vomiting are common after a dose increase but usually settle in a few days. Adverse effects are rare but serious. They include decreased platelets or white blood cells, Stevens–Johnson syndrome, exfoliative dermatitis, and hepatitis Check full blood count, liver function tests, and serum creatinine if an idiosyncratic reaction is suspected. 155
- 156. Gabapentin (Neurontin) Gabapentin is an alternative for first-line treatment if carbamazepine is contraindicated or not tolerated 300 to 600 mg tid (300 mg once on day 1, 300 mg bid on day 2, 300 mg tid on day 3, then increasing dose as needed to 600 mg tid) Common adverse effects of gabapentin include drowsiness, dizziness, ataxia, and fatigue. The clearance of gabapentin is markedly reduced in renal impairment. The total daily dose should not exceed 1200 mg in someone with mild renal impairment (common in elderly people). 156
- 157. Lamotrigine (Lamictal) This drug provided sustained relief in 2 small prospective studies. With concomitant antiepileptic drugs, initiate at 25-50 mg qid for 2 week, then increase by 25-50 mg/day. Max dosage is 400 mg/day. Phenytoin (Dilantin) Drug has similar mechanism of action as carbamazepine but is probably less effective. The drug has several common adverse effects, which often are troublesome in older patients The drug may provide relief as an add-on drug when carbamazepine monotherapy wanes, as commonly happens after 1 or several years. 157
- 158. Topiramate It is a second-line agent ,the efficacy of which is still to be established Risk of developing a kidney stone is increased 2-4 times that of untreated population. Patients taking topiramate should seek immediate medical attention if they experience blurred vision or periorbital pain. Continued usage after symptoms develop can lead to glaucoma. 158
- 159. INJECTION THERAPY When the medicinal therapy does not provide the relief injection of absolute alcohol and anesthetic solution are used. Injection Of Anesthetic Solution: The nerve may be injected with the 2% Xylocaine Hydrochloride solution to break the pain cycle. This may be followed by oedema at the site of injection and trismus The relief may last for few weeks to months and injection can be repeated when the pain occurs 159
- 160. Injection Of Absolute Alcohol: Injection of absolute alcohol around the nerve trunk or the ganglion gives good results It provides the relief for the period of 6 to 12 months . The injection are given into the maxillary and mandibular division of trigeminal nerve at the level of the base of skull. The peripheral alcohol injection are given at the level of infraorbital foramen, mental foramen and inferior alveolar foramen 160
- 161. SURGERY For patients in whom medical therapy has failed, surgery is a viable and effective option. Among patients who develop TN when younger than 60 years, surgery is the definitive treatment. Surgery exposes the patient to operative risks and the risk of permanent, residual facial numbness and dysesthesias. The primary complications of surgery include permanent anesthesia over the face or the troubling dysesthetic syndrome of anesthesia dolorosa. 161
- 162. Three operative strategies now prevail: a) Percutaneous Procedures b) Gamma Knife Surgery (GSK) c) Micro vascular decompression (MVD) 162
- 163. SURGERY Pain-free intervals after percutaneous procedures last 1.5-2 years, 3-4 years after another percutaneous procedure, and 15 years commonly after MVD (Sweet, 1988). Percutaneous surgeries are usually indicated for older patients with medically unresponsive TN. Younger patients and those expected to do well under general anesthesia should first consider micro vascular decompression– presently the most cost-effective surgery 163
- 164. PERCUTANEOUS SURGERIES Percutaneous procedures usually can be performed on an outpatient basis under local or brief general anesthesia at acceptable or minimal risk of morbidity. For these reasons, they commonly are performed in debilitated persons or those older than 65 years. There are 3 types of procedures: a) Percutaneous Radiofrequency Trigeminal Gangliolysis (PRTG) b) Percutaneous Retrogasserian Glycerol Rhizotomy (PRGR) c) Percutaneous Balloon Microcompression (PBM). 164
- 165. In (PRTG) radiofrequency heating tip sears the ganglion until the area of facial pain becomes numb PRTG has gained wide acceptance , because the patient is awake during the procedure, recovers quickly, and goes home the day of the procedure or the next day. 165 PERCUTANEOUS RADIOFREQUENCY TRIGEMINAL GANGLIOLYSIS (PRTG)
- 166. PERCUTANEOUS RETROGASSERIAN GLYCEROL RHIZOTOMY (PRGR) In PRGR, a spinal needle penetrates the face, this time to the trigeminal cistern, at which point a cisternogram is obtained with water-soluble contrast material. After removing this material, the surgeon instills anhydrous glycerol, asking the patient to remain seated for an additional 2 hours to fully ablate the nerve. 166
- 167. GAMMA KNIFE SURGERY This technique is minimally invasive, is associated with a low risk (10%) of facial paresthesias or sensory loss, and offers a high rate (86%) of significant, initial pain relief. Focuses cobalt radiation upon TN root producing a delayed injury to nervous tissue 167
- 168. The pain recurrence rate is low for patients who initially attain complete relief. It is generally effective, even in patients in whom prior surgery or medication trials failed. Patients must wait 1 month for the pain to resolve. The technique is less technically demanding and less operator- dependent. 168
- 169. MICROVASCULAR DECOMPRESSION (MVD) Microvascular decompression commonly is performed in younger, healthier patients, especially those with pain isolated to the ophthalmic division or in all 3 divisions of the trigeminal nerve and in those with secondary TN. High initial success rates (>90%) have led to the widespread use of this procedure. Pain control rate after single MVD at 10 years is 64% It is generally agreed that MVD provides the longest duration of pain relief while preserving facial sensation. 169
- 170. Skin incision is given behind the ear and a 3-cm craniectomy is performed . After retracting the dura to expose the trigeminal nerve, arterial loop compressing the nerve as it enters the pons is identified . Then this vascular structure is padded with Teflon felt. Recovery is more prolonged than with percutaneous procedures. 170
- 171. PERIPHERAL TRIGEMINAL NERVE BLOCKS, SECTIONING AND AVULSIONS: Involves injuring the peripheral portions of TN external to skull to provide permanent pain relief. Indicated in older patients, more than 60 years of age. Used as the last resort, when all other treatments have failed. 17 1
- 172. Radiosurgery: Several reports have documented the efficacy of Gamma Knife stereotactic radiosurgery for TN Because radiosurgery is the least invasive procedure for TN, it is a good treatment option for patients with co-morbidities, High-risk medical illness or pain refractory to prior surgical procedures. 172
- 173. 2. TRIGEMINAL NEUROPATHY • Often referred to as Trigeminal neuropathic pain. • It is the sensory loss of facial muscles or weakness of the jaw muscles. CAUSES: SLE, Sjogren’s syndrome, Herpes zoster, Leprosy Meningioma, Schwanomma, Wallenberg syndrome, Vertebral artery occlusion, Infarction of lateral medulla
- 174. SYMPTOMS - ipsilateral facial sensory loss, ipsilateral Horner’s syndrome, ipsilateral IX,X,XI palsy ipsilateral cerebellar ataxia , contralateral sensory loss TREATMENT- Antiepileptic drugs like Carbamezepine. Phenytoin, Gabapentin Tricyclic antidepressants like Amitriptyline and Imipramine Medications rarely provide complete relief but can reduce the severity of the symptoms Councelling of the patient as it is a disease with long term effects. 17 4
- 175. 3. HERPES ZOSTER OPHTHALMICUS: About 15% of the cases of Herpes zoster (HHV3/Varicella zoster) involve the trigeminal nerve. Most frequently affecting nasociliary branch of the Ophthalmic division. Gasserian ganglion Ophthalmic nerve Supraorbital Nerve. Infraorbital N. Supratrochlear Nerve. Infratrochlear Nerve. Nasal Nerve.
- 176. CLINICAL FEATURES: Pain precedes skin lesion Clinical feature is hemifacial unioccular cutaneous lesions - Maculopapular rash Vesicle Pustules Crust Permanent scar
- 177. • III, IV, VI th cranial nerve palsy • Progressive proptosis • Post herpetic neuralgias • Keratitis, conjunctivitis, scleritis, iritis, anterior uveitis, retinitis. • Without antiviral therapy, 50-70% cases develop ocular complications. Treatment: • Analgesics • Anti depressants • Anti viral therapy for VZV infection • Trigeminal rhizotomy • Stellate ganglion block
- 178. 178 4. CAVERNOUS SINUS SYNDROME:
- 179. Potential causes of cavernous sinus syndrome include – 1. Metastatic tumors, 2. Direct extension of nasopharyngeal tumors 3. Meningioma, 4. Pituitary tumors 5. Aneurysms of the intracavernous Carotid artery 6. Cavernous-Carotid arteriovenous fistula, 7. Bacterial infection causing cavernous sinus thrombosis, 8. Aseptic thrombosis 9. Fungal infections like rhinocerebellar mucormycosis, actinomycosis, aspergillosis.
- 180. • Multiple cranial neuropathies: 1. Cavernous sinus tumors – metastatic lesions, pituitary tumors,cavernous sinus meningiomas. 2. Cavernous sinus aneurysm 3. Carotid – Cavernous fistulas 4. Cavernous sinus thrombosis 5. Miscellaneous inflammatory syndrome – Tolosa-Hunt syndrome, Horner’s syndrome. • Cavernous sinus syndrome is a medical emergency, requiring prompt medical attention, diagnosis, and treatment
- 181. TREATMENT: 1. Cavernous sinus tumors – • Metastatic lesions – Radiotherapy may offer transient improvement. • Pituitary tumors – May improve with oral dopamine agonists Resection of the tumor • Cavernous sinus meningiomas – Radiotherapy Gamma Knife Surgery 2. Cavernous sinus aneurysm – Endovascular balloon occlusion. 3. Carotid-Cavernous fistulas – Endovascular obliteration of fistula with colis. Some cases can be observationally managed 181
- 182. 4. Cavernous sinus thrombosis – High-dosage antibiotic therapy Drainage of any primary site of infection (e.g. abscess, sinusitis) Anticoagulation in aseptic patients. 5. Miscellaneous inflammatory syndrome – Tolosa-Hunt syndrome responds well to a course of high dosage steroid thetrapy for 3 to 6 months, which is slowly tapered off. 182
- 183. 5. NEUROTROPHIC KERATITIS Occurs due to partial or complete corneal anaesthesia due to loss of sensory innervation by the Trigeminal nerve. There is impaired response to corneal microtrauma as a result of impaired regeneration and healing of corneal epithelium CAUSES: • Bacterial infections – HSV, VZV, Leprosy. • Traumatic vascular nerve injury • Ablation of gasserian ganglion • Chemical burns • Topical anesthetic abuse, • Beta blockers • NSAIDS • Contact lens wear
- 184. SYSTEMIC: • Diabetes mellitus • Stroke • Brainstem hemorrhage • Aneurysm • Congenital TREATMENT: Mild epithelial defects can be treated with Erythromycin ointment 4-8 times/day. If corneal ulceration has occurred, smears and cultures are taken to rule out any infections. If culture is sterile, and no response to ointment is seen, consider a bandage contact lens, tarsorrhaphy, amniotic membrane graft or a conjunctival flap. 184
- 185. 6. GRADENIGO’S SYNDROME: Petrous bone osteitis due to suppurative otitis media Characterized by - • Ipsilateral Trigeminal Nerve palsy (Va, Vb) • Retro orbital pain • Ipsilateral sixth nerve palsy • Other symptoms include – photophobia, excessive lacrimation, fever and reduced corneal sensitivity. PETROUS BONE OSTEITIS
- 186. TREATMENT: The medical treatment is done with antibiotics: Ceftiaxone plus metronidazole (which covers anaerobic bacteria). In more severe cases, a parancentesis (aspiration of fluids) or mastoidectomy may be needed. 186
- 187. 7. RAEDER’S PARA TRIGEMINAL SYNDROME Oculosympathetic paresis with pain in distribution of trigeminal Nerve. Patient with episodic chronic pain Pain and headache Trigeminal hyperasthesia seen in areas supplied by post ganglionic fibers.
- 188. SIGNS AND SYMPTOMS: Pulling pain over the zygomatic region which may radiate behind and below the ear. Pain presents at morning and recurs at night time. Wooshing & buzzing sound in the ear. Numbness over the affected side of face. Blurred vision. Unable to bite. Nostrils appear blocked.
- 189. TREATMENT: • Unless intracranial pathology exists, treatment remains symptomatic. • For the management of associated pain, antispasmodic drug such as Baclofen or anticonvulsants such as Carbamazepine, Gabapentin, Pregabalin and Topiramte may be effective. • Anti-inflammatory agents such as corticosteroids can also be effective, and at times narcotic analgesics such as ergotamines may also be used. • The efficacy of Tricyclic antidepressants (TCAs) has also been demonstrated in some patients. • Vitamin B supplements can be given as adjuvant therapy. • Surgery is not indicated in most patients unless a secondary cause is found which justifies surgical intervention. 189
- 190. 8. STURGE WEBER SYNDROME/ ENCEPHALO TRIGEMINAL ANGIOMATOSIS •Rare congenital neurological & skin disorder •Often associated with port-wine stains of the face, glaucoma, seizures and mental retardation. •It is diagnosed clinically, based on the typical cutaneous, central nervous symptom (CNS), and ocular abnormalities. •Neurological symptoms include: 1. Developmental delay or intellectual disability 2. Learning problems 3. Attention deficit hyperactivity disorder (ADHD).
- 191. • Port-wine stains • Macrocephaly • Soft-tissue hypertrophy • Hemiparesis • Visual loss • Ocular manifestations • hemianopsia 191 SIGNS AND SYMPTOMS: PORT-WINE STAINS
- 192. TREATMENT: Medical care includes anticonvulsants for seizure control, symptomatic and prophylactic therapy for headache, glaucoma treatment to reduce intra-optic pressure, and laser therapy for port-wine stains, ANTIEPILEPTIC DRUGS: with an efficacy in focal seizures are preferred. The chance of achieving seizure control with medical treatment varies from patient to patient. GLAUCOMA MEDICATION: The goal of treatment is to control IOP to prevent Optic nerve injury. • Beta-antagonist eye drops – decrease the production of aqueous fluid. • Carbonic anhydrase inhibitors – also decrease the production of aqueous fluid. • Adrenergic eye drops and miotic eye drops – promote drainage of aqueous fluid 192
- 193. DYE LASER PHOTOCOAGULATION: Treatment of cutaneous type with Dye Laser photocoagulation has been helpful in reducing the cosmetic blemishes from the cutaneous vascular dilatation. SURGERY: is desirable in patients who have refractory seizures, glaucioma, or specific problems related to various disorders associated with Sturge Weber syndrome like Scoliosis. 193
- 194. CONCLUSION: Trigeminal nerve is a mixed nerve and it mainly supplies the regions of the face, head and neck. The various techniques of local anaesthesia are all directed towards the Trigeminal nerve. Thus, as a Public Health Dentist one should know thoroughly about the course and distribution of the Trigeminal nerve, to diagnose the pathologies associated with the nerve and their appropriate treatment. 194
- 195. REFERENCES: • Gray’s Anatomy – Henry Gray F. R. S. • Clinical Anatomy – Richard S. Snell • Human Anatomy: Head and Neck, Brain – B. D. Chaurasia • Handbook of Local Anaesthesia – Stanley F Malamed • Local Anaesthesia and Pain control in Dental Practice – Monheims, C Richard Bennett. 195
- 196. 196 THANK YOU
Editor's Notes
- Potential causes of cavernous sinus syndrome include metastatic tumors, direct extension of nasopharyngeal tumors, meningioma, pituitary tumors or pituitary apoplexy, aneurysms of the intracavernous carotid artery, cavernous-carotid arteriovenous fistula, bacterial infection causing cavernous sinus thrombosis, aseptic thrombosis, idiopathic granulomatous disease (Tolosa-Hunt syndrome), and fungal infections. Cavernous sinus syndrome is a medical emergency, requiring prompt medical attention, diagnosis, and treatment
- Symptoms Sturge–Weber syndrome is manifested at birth by seizures accompanied by a large port-wine stain birthmark on the forehead and upper eyelid of one side of the face. The birthmark can vary in color from light pink to deep purple and is caused by an overabundance of capillaries around the ophthalmic branch of the trigeminal nerve, just under the surface of the face. There is also malformation of blood vessels in the pia mater overlying the brain on the same side of the head as the birthmark. This causes calcification of tissue and loss of nerve cells in the cerebral cortex. Neurological symptoms include seizures that begin in infancy and may worsen with age. Convulsions usually happen on the side of the body opposite the birthmark and vary in severity. There may be muscle weakness on the same side.[clarification needed] Some children will have developmental delays and mental retardation; about 50% will have glaucoma (optic neuropathy often associated with increased intraocular pressure), which can be present at birth or develop later. Increased pressure within the eye can cause the eyeball to enlarge and bulge out of its socket (buphthalmos). Sturge–Weber syndrome rarely affects other body organs.