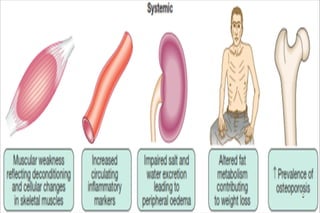
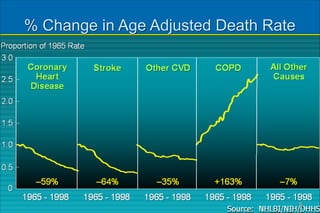
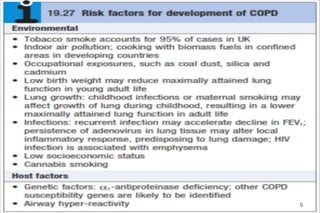
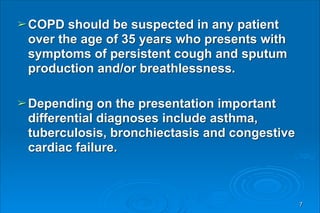
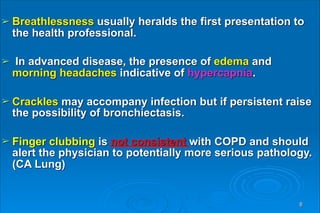
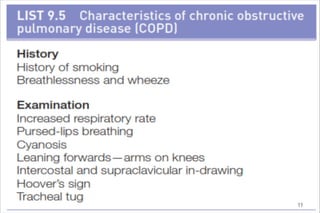
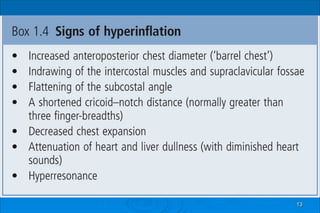
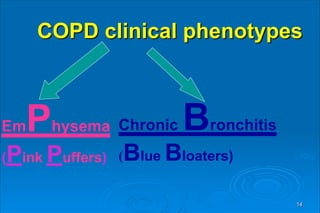
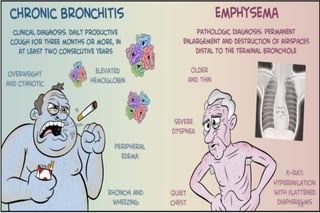
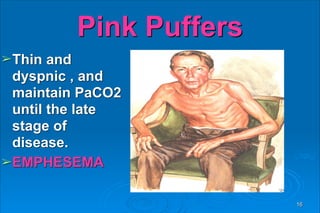
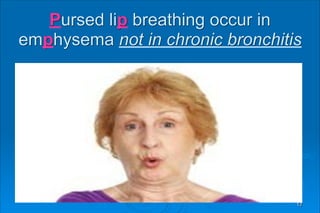
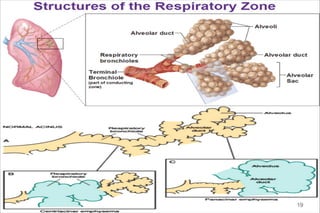
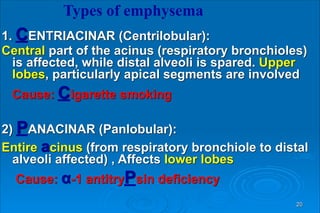
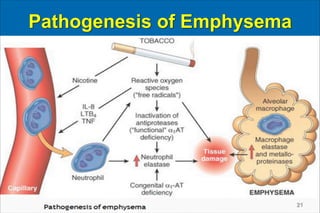
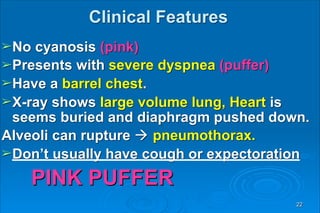
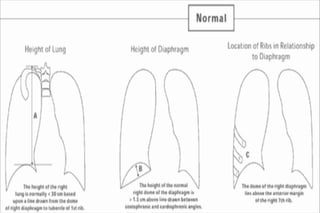
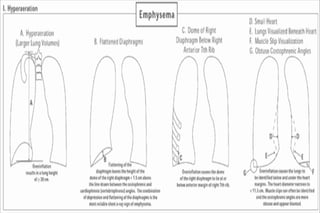
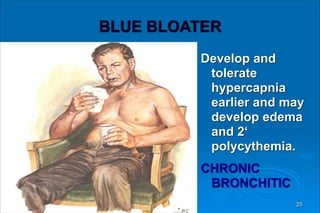
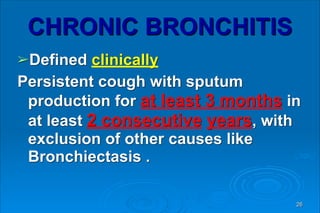
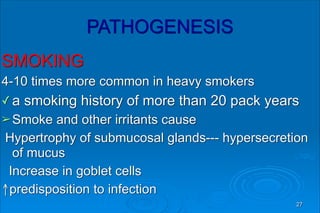
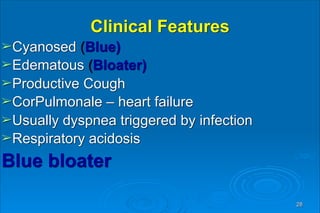
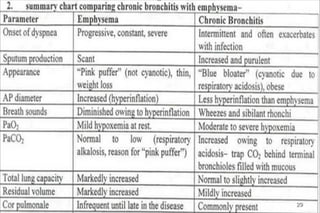
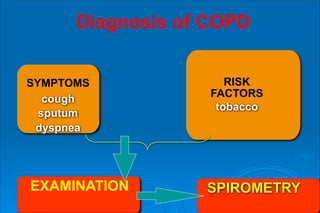
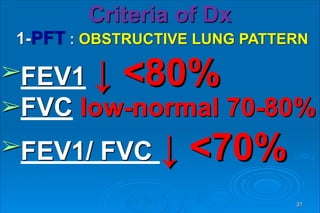
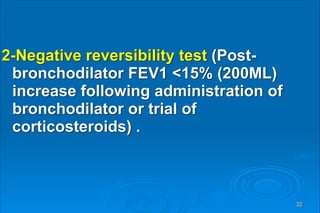
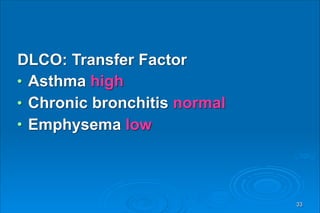
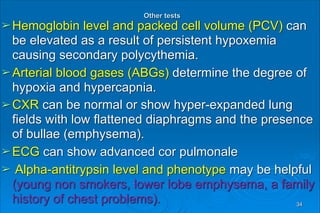
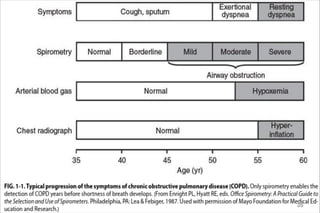
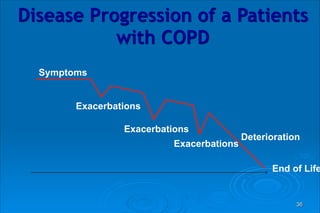
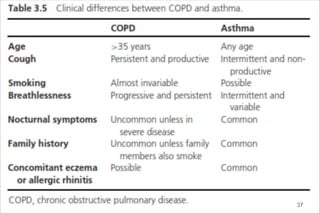
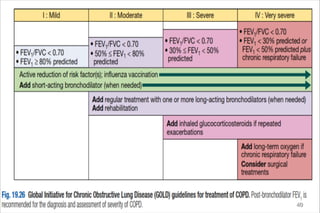
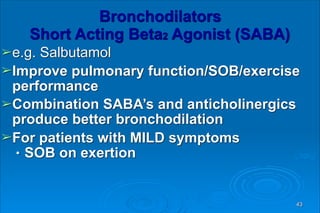
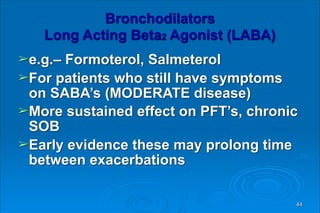
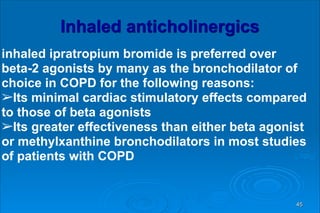
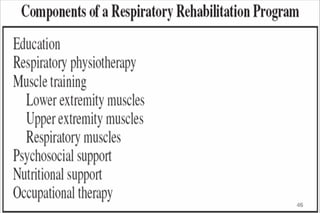
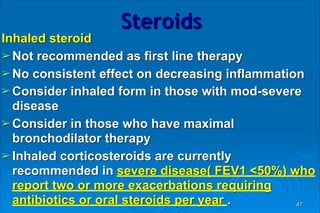
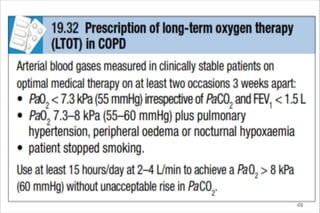
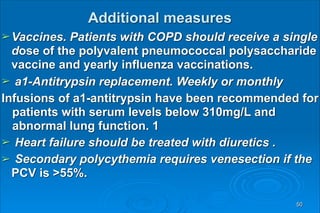
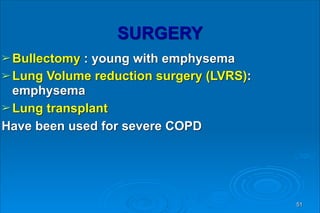
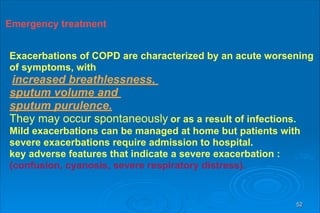
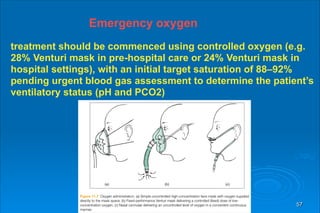
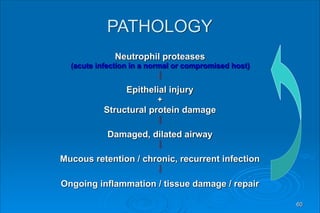
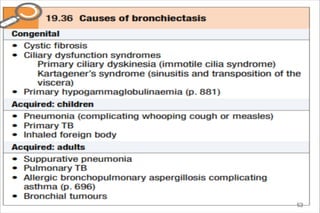
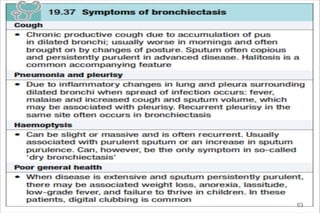
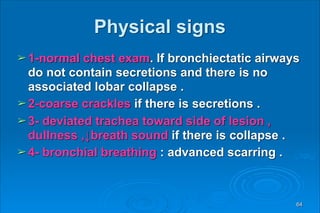
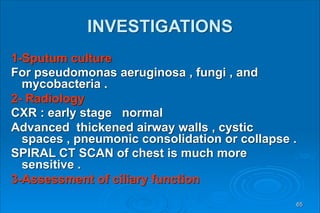
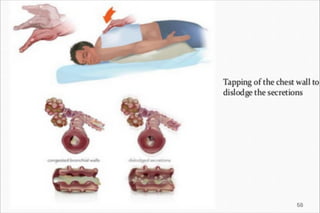
This document provides information about chronic obstructive pulmonary disease (COPD) including its definition, causes, diagnosis, management, and related conditions like emphysema and bronchiectasis. COPD is a progressive lung disease characterized by limited airflow in the lungs. The primary cause is cigarette smoking which leads to an abnormal inflammatory response in the lungs. Symptoms include breathlessness, chronic cough, and sputum production. Spirometry is required for diagnosis and shows airflow limitation. Management involves smoking cessation, bronchodilators, steroids, vaccines, and oxygen supplementation during exacerbations. Related conditions like emphysema and bronchiectasis are also discussed.