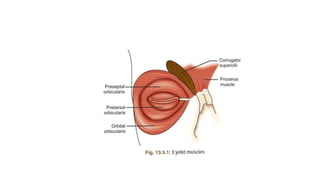
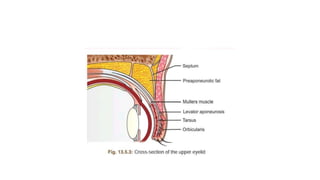
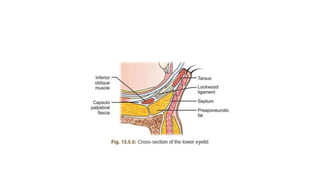
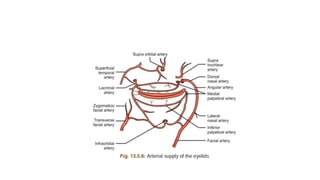
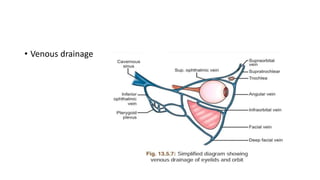
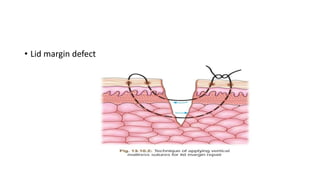
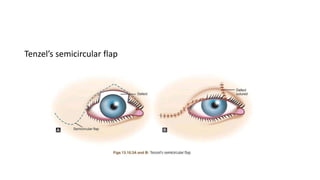
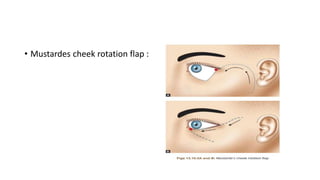
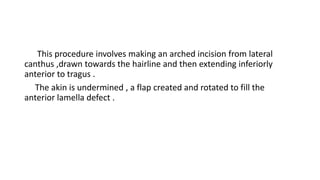
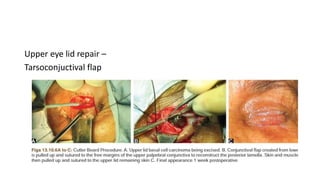
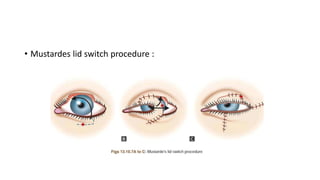
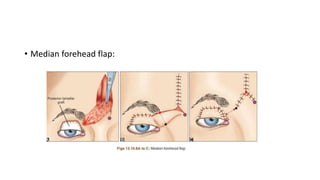
This document summarizes eyelid reconstruction techniques for various types of eyelid defects. It begins by describing the anatomy of the eyelid and its blood supply. It then classifies eyelid defects and outlines approaches for different defect sizes, including primary closure, skin grafts, local flaps like Tenzel's semicircular flap and V-Y flap for defects up to 50%, and workhorse flaps like Hughes tarsoconjunctival flap and Mustarde's cheek rotation flap for larger defects up to 75%. For total eyelid loss, conjunctival flaps are covered with forehead flaps, with division later for eyelid formation. The goal is to restore the layered anatomy and function of the eyelid.