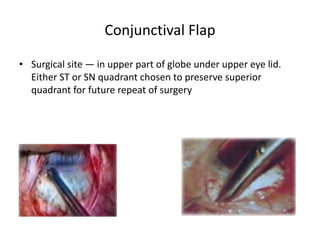
Trabeculectomy is a surgical procedure to lower intraocular pressure by creating a fistula between the anterior chamber and subconjunctival space. This allows aqueous humor to drain out of the eye and form a filtering bleb under the conjunctiva. It involves making a partial thickness scleral flap, creating a sclerostomy, and sometimes using antimetabolites to modulate healing. The procedure aims to lower IOP while avoiding complications like hypotony, infection, or bleb failure. Close postoperative monitoring is required to manage IOP and bleb formation.