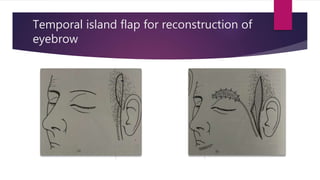
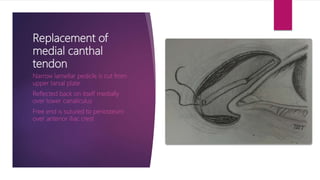
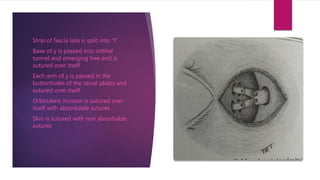
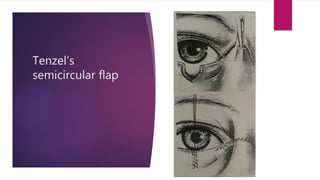
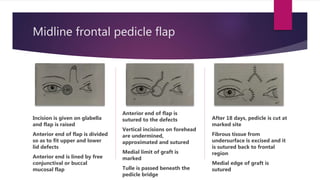
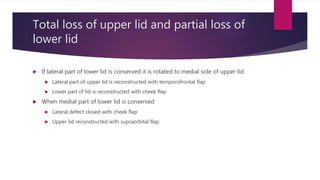
The document discusses the anatomy and surgical techniques for eyelid reconstruction. It describes the thin skin of the eyelids with no subcutaneous fat. It outlines techniques for closing lid defects like V-Y plasty, Mustarde's operation using cheek rotation flaps, and Tenzel's semicircular flap. Surgical considerations are to preserve the lid margin and orbicularis muscle. Closure of full thickness lid defects involves suturing in layers from the grey line to the skin. Local flaps, free grafts, and pedicled grafts can be used for reconstruction, with options like temporal island flaps for eyebrows.