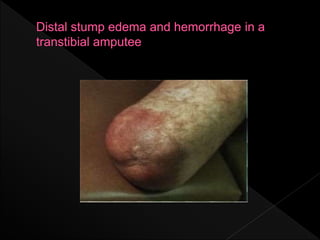
This document discusses pain management, skin disorders, and psychological consequences related to amputation. It covers different types of pain experienced after amputation like immediate postoperative pain and phantom limb pain. Skin issues from poor hygiene, infections, and reactions to the prosthetic are examined. Management of pain, skin conditions, and the important role of psychology in adapting to life with an amputation are summarized.