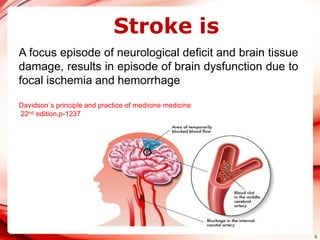
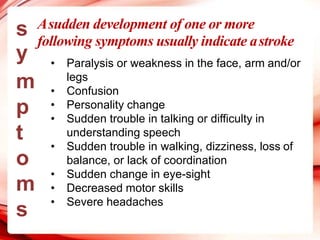
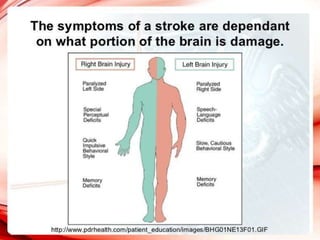
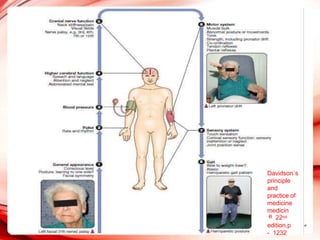
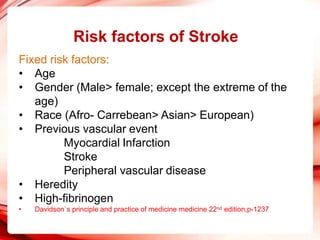
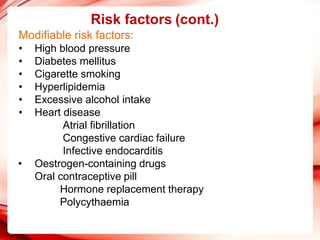
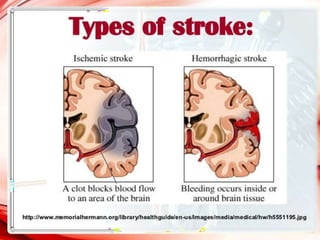
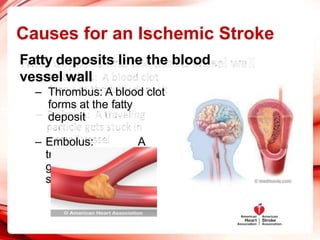
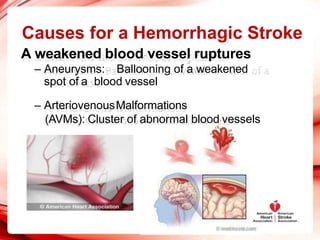
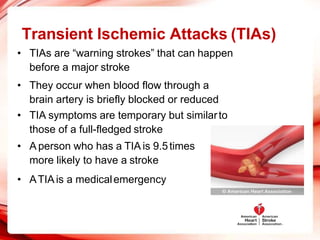
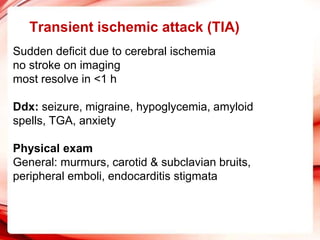
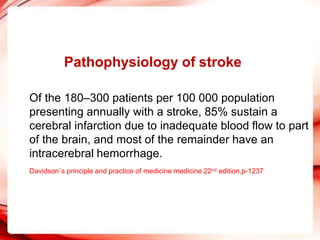
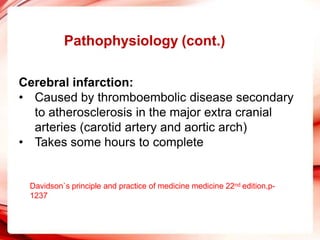
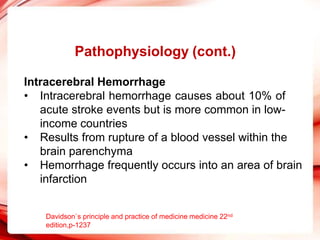
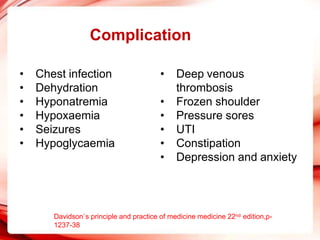
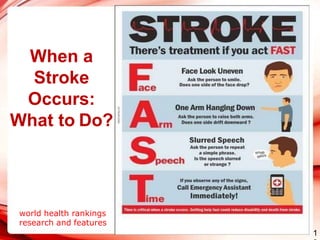
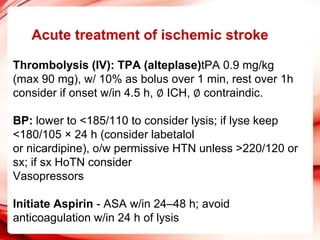
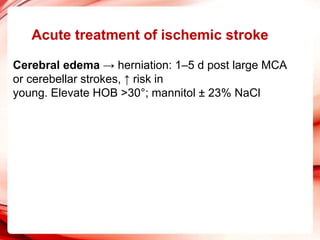
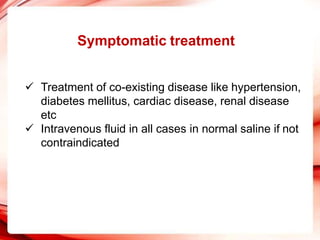
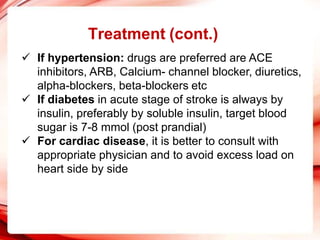
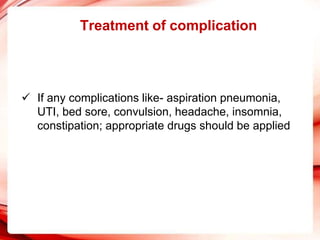
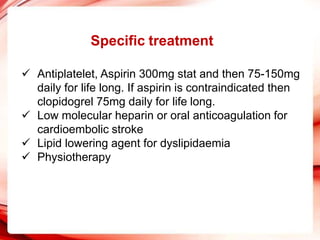
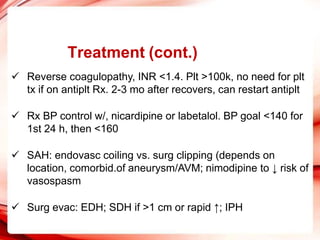
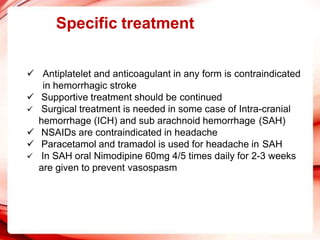
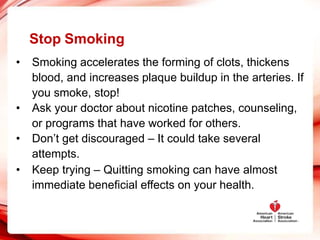
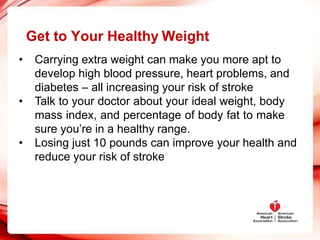
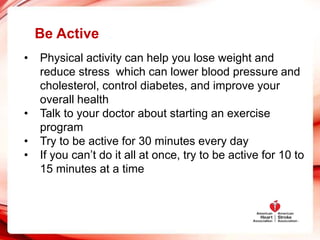
Stroke occurs when blood flow to the brain is interrupted, depriving brain tissue of oxygen and nutrients. The main types of stroke are ischemic (caused by blockage) and hemorrhagic (caused by bleeding). Risk factors include high blood pressure, diabetes, smoking, high cholesterol, obesity, heart disease, age, gender, family history, and prior vascular events. Treatment depends on the type of stroke but may involve clot-busting drugs, surgery, rehabilitation, and managing risk factors to prevent future strokes. Lifestyle changes like quitting smoking, losing weight, exercising, and following a healthy diet can significantly reduce the risk of having a stroke.