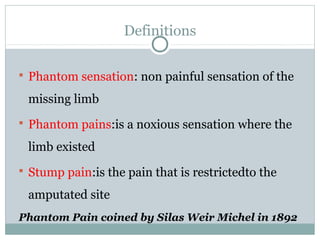
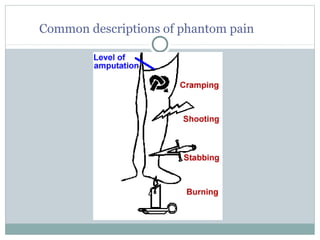
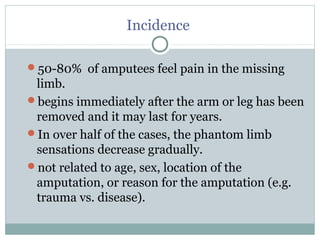
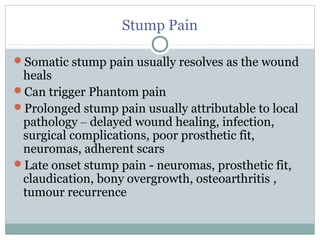
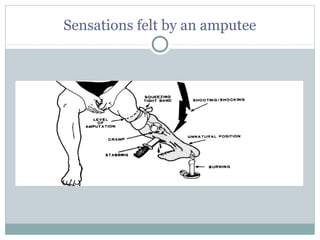
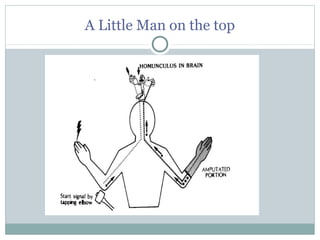
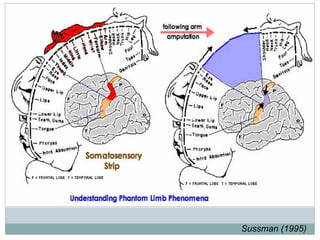
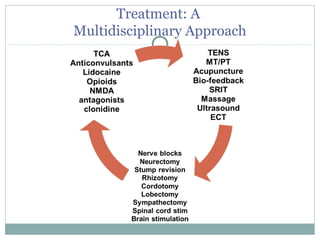
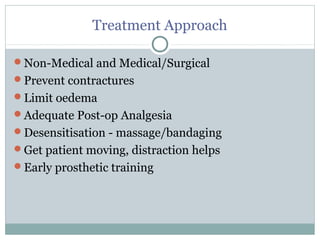
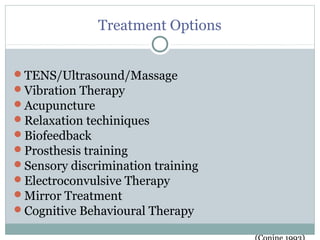
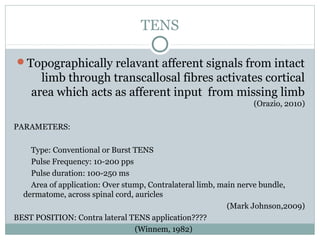
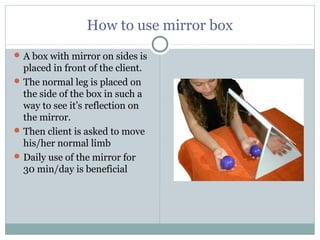
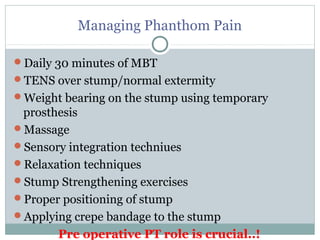
Phantom limb pain is experienced by 50-80% of amputees as pain in the missing limb. It is caused by neuromas forming at the amputation site that generate abnormal activity. Central and peripheral sensitization in the spinal cord and brain reorganize sensory processing after limb loss. A multidisciplinary approach is needed including desensitization, mirror therapy, TENS, massage and prosthesis training to manage phantom limb pain. Regular use of mirror box therapy tricking the brain into seeing movement of the missing limb has shown effectiveness in reducing phantom limb pain.