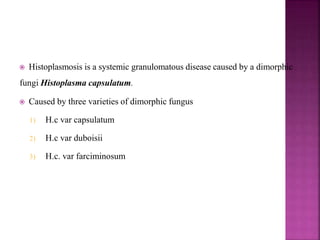
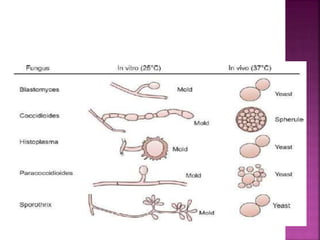
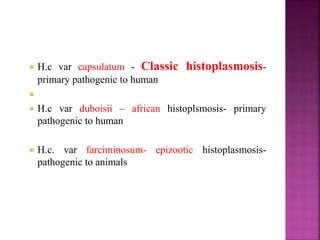
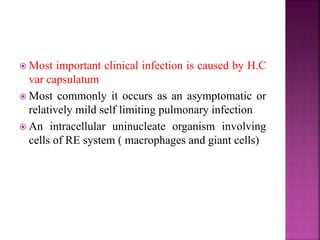
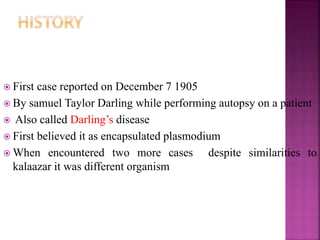
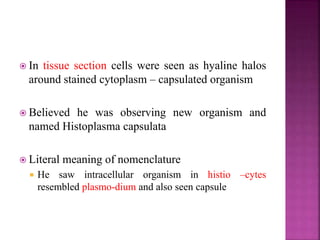
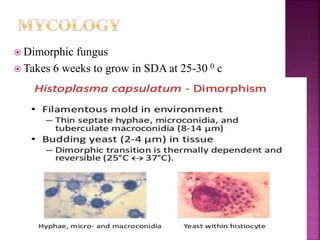
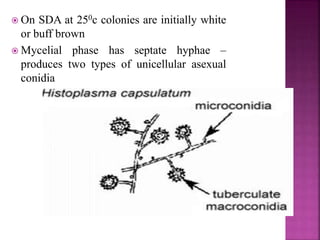
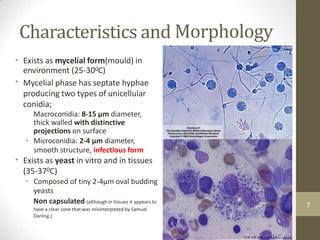
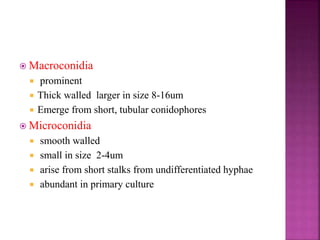
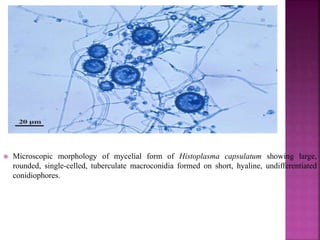
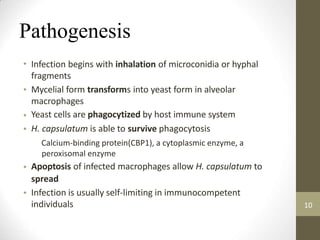
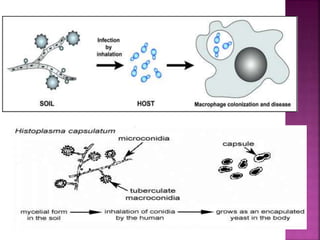
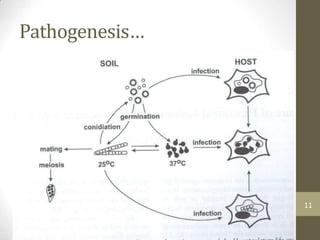
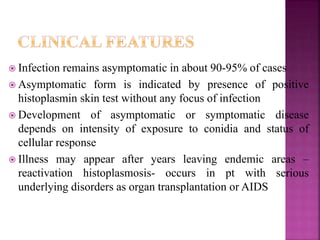
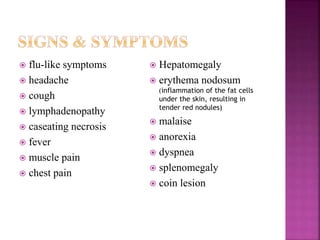
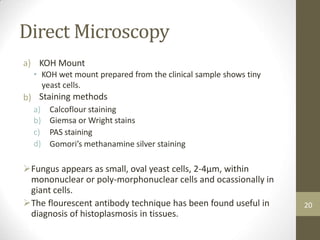
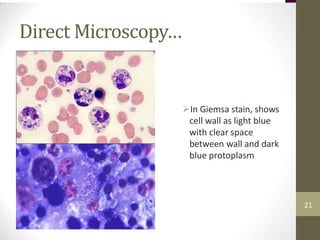
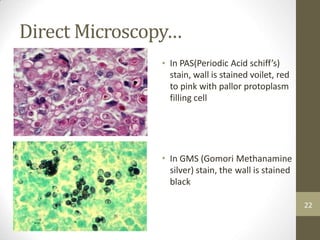
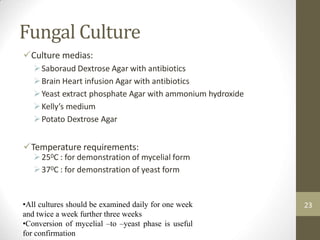
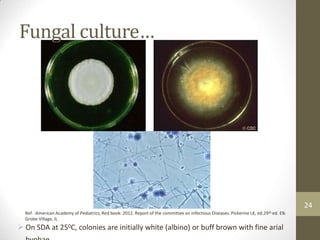
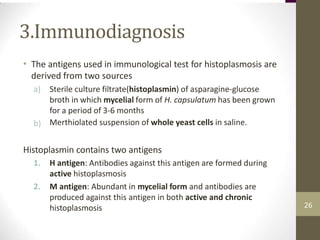
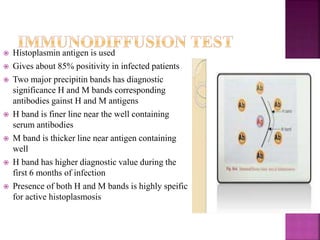
Histoplasmosis is caused by the dimorphic fungus Histoplasma capsulatum. It exists in the mycelial phase in the environment and the yeast phase in tissues. Infection occurs via inhalation of microconidia from contaminated soil. Most infections are asymptomatic, but some may cause flu-like symptoms. Diagnosis involves microscopy of clinical samples or cultures to identify the yeast cells. Serological tests and skin tests also assist in diagnosis. Amphotericin B and itraconazole are used to treat severe or disseminated cases.