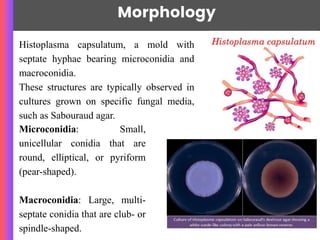
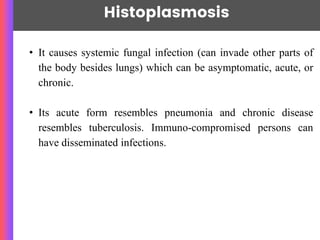
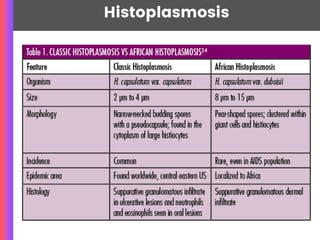
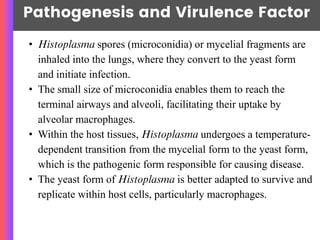
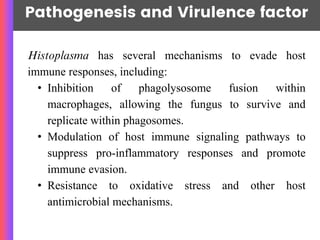
Histoplasma is a dimorphic fungus, primarily Histoplasma capsulatum, which causes histoplasmosis, a disease that can range from asymptomatic to severe. The infection is primarily acquired through inhalation of spores in environments contaminated with bird or bat droppings and can affect various organs, particularly in immunocompromised individuals. Diagnosis involves microscopy, culture, and serological tests, with antifungal therapy being the main treatment approach.