This document provides information about histoplasmosis, including its characteristics, pathogenesis, types, clinical presentation, and laboratory diagnosis. It can be summarized as follows:
1. Histoplasmosis is caused by the dimorphic fungus Histoplasma capsulatum, which exists in both a mycelial and yeast form. It is found worldwide in soil contaminated with bird or bat droppings.
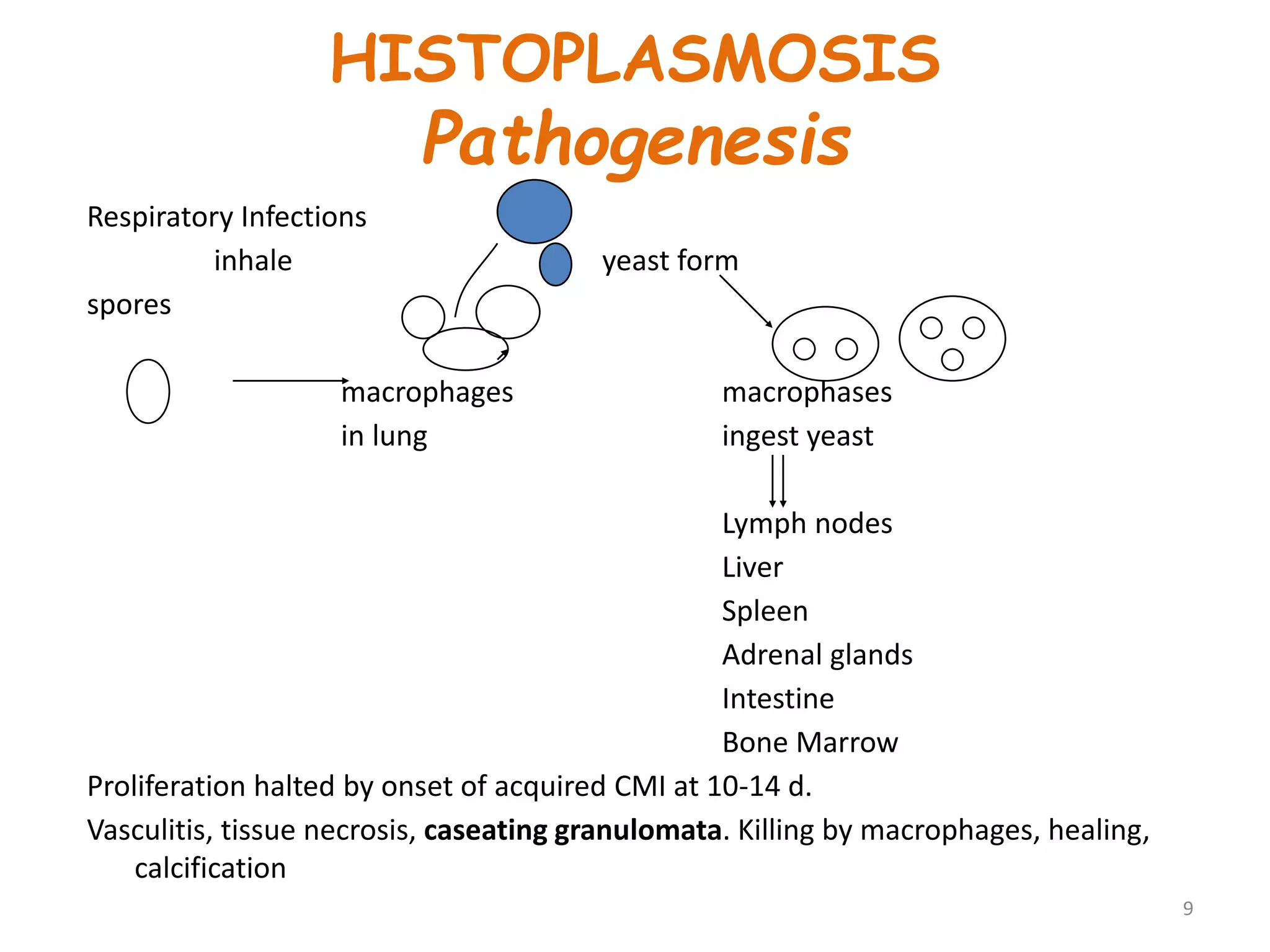
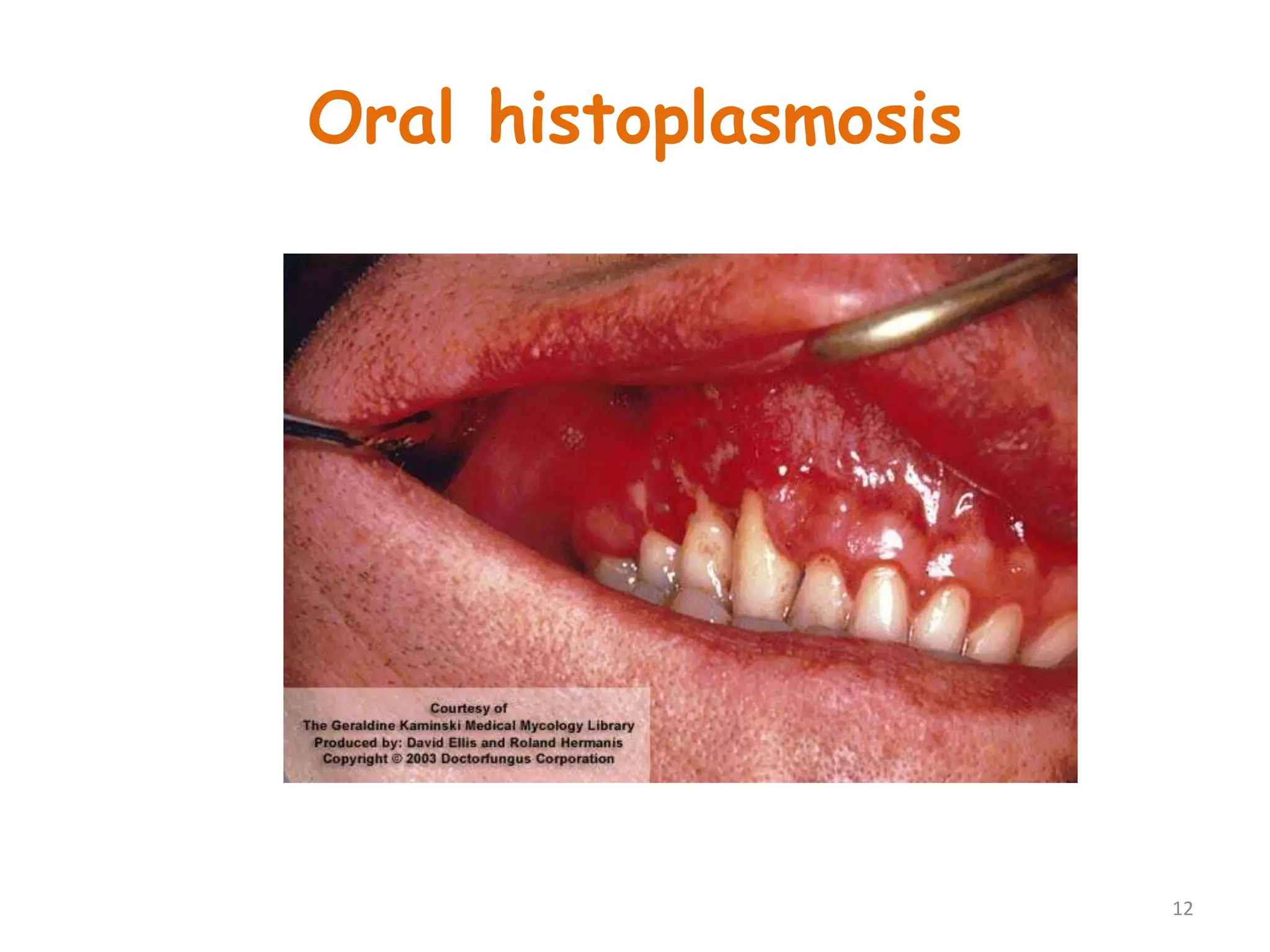
2. Infection typically occurs via inhalation of yeast cells into the lungs. It can cause pulmonary or disseminated disease, spreading to organs in immunocompromised individuals.
3. Laboratory diagnosis involves direct examination of samples for yeast cells, culture of the fungus, and serological tests like complement fixation