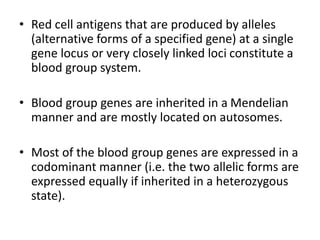
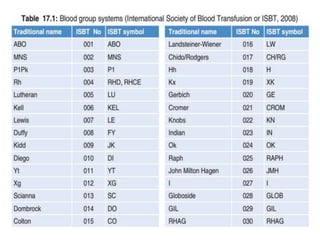
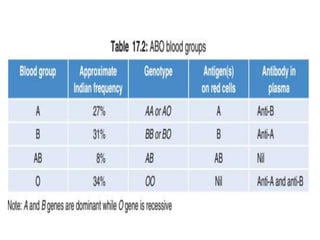
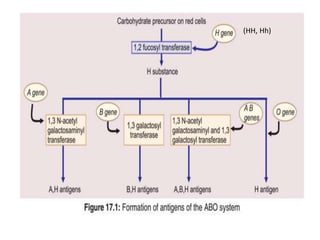
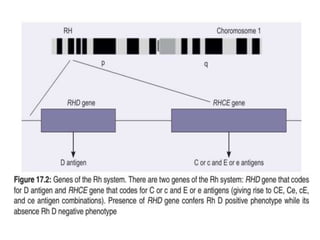
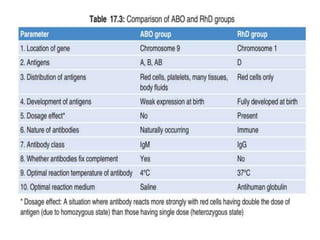
This document summarizes important blood group systems, focusing on ABO and Rh systems. It describes how blood group antigens are inherited and expressed, and the clinical significance of various blood group antibodies. The ABO system has four main blood types (A, B, AB, O) based on carbohydrate antigens. The Rh system's most important antigen is D, which readily induces anti-D antibodies in Rh-negative individuals, requiring careful blood typing to avoid transfusion reactions or hemolytic disease of the newborn.