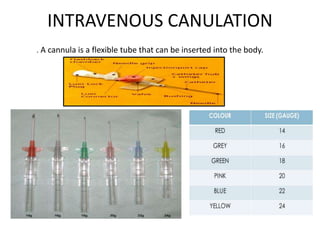
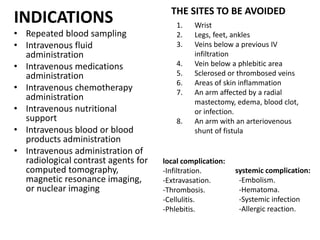
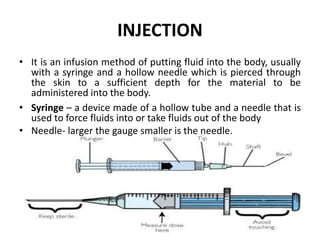
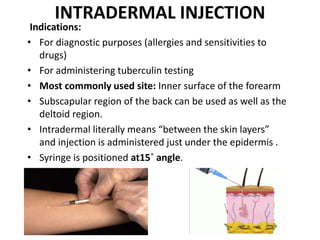
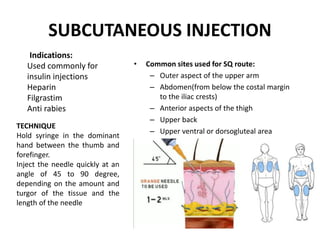
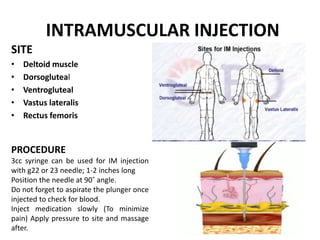
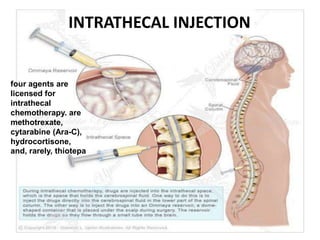
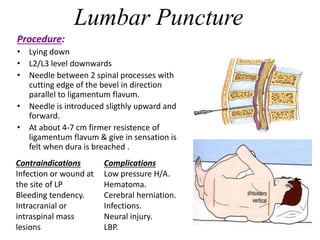
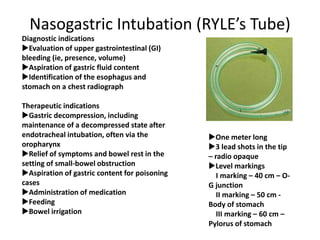
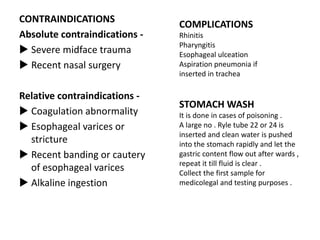
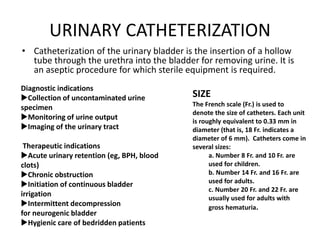
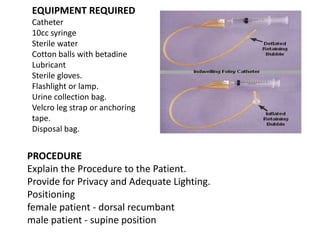
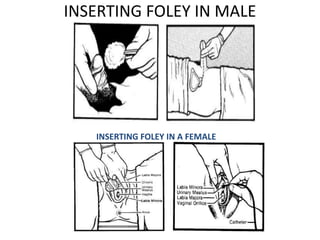
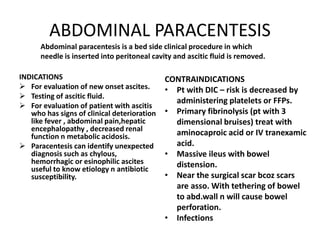
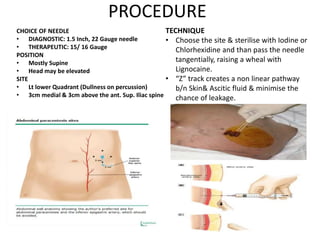
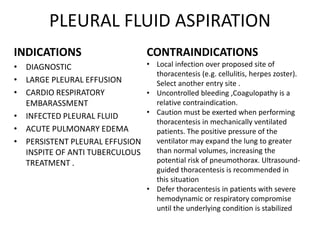
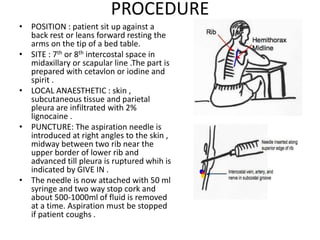
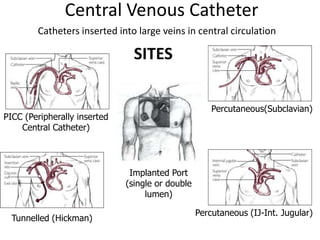
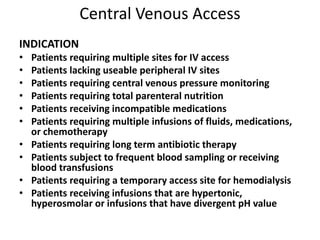
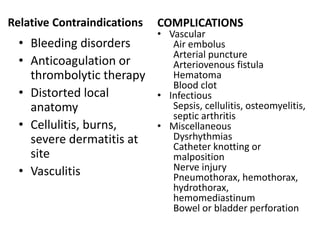
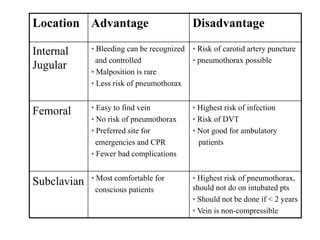
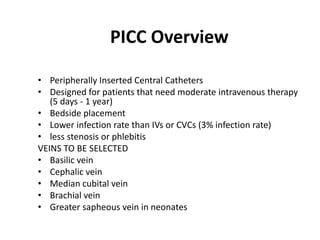
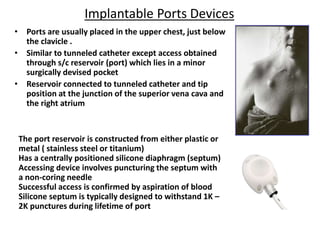
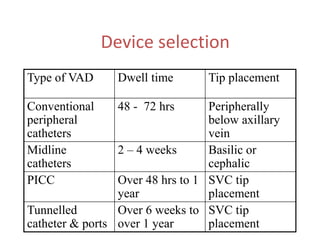
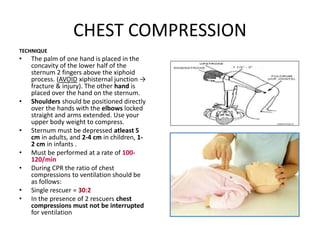
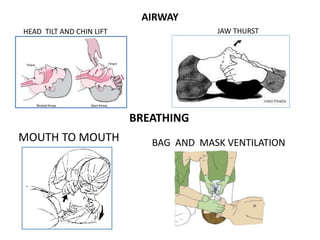
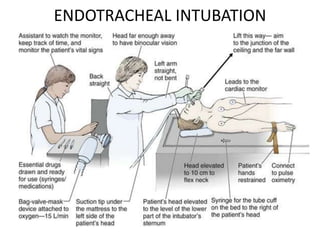
Dr. Durgesh Kumar presented various therapeutic procedures including IV cannulation, injection techniques, Ryle tube insertion, Foley catheterization, abdominal paracentesis, intraperitoneal chemotherapy, pleural fluid aspiration, lumbar puncture, and central venous access. The presentation covered indications, contraindications, equipment, procedures, and potential complications for each technique. Dr. Kumar also discussed cardiopulmonary resuscitation and its basic steps of compressions, airway, and breathing.