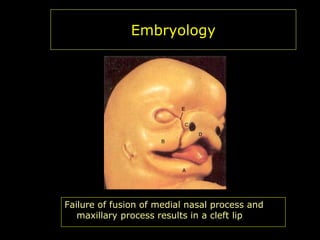
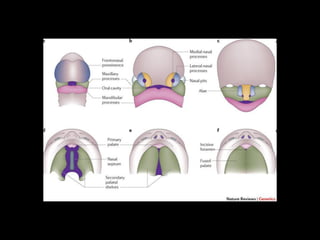
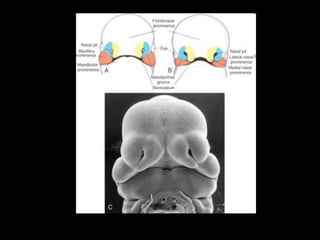
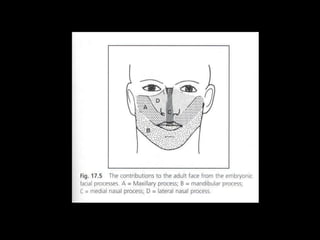
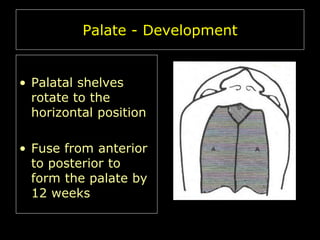
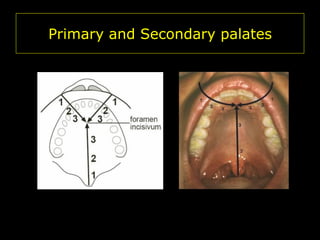
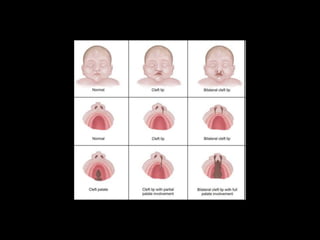
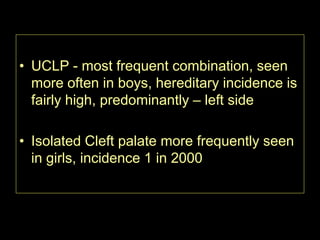
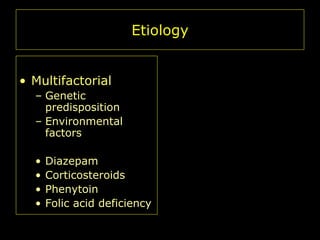
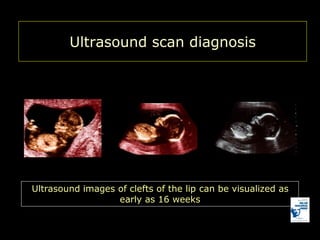
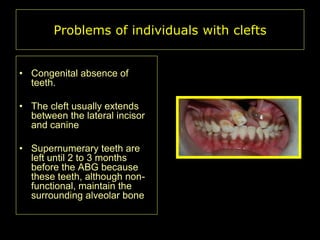
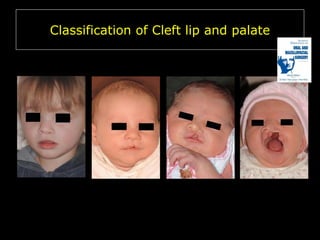
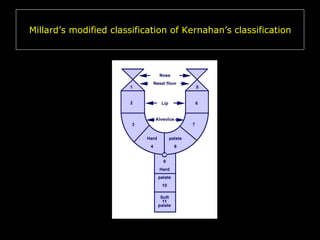
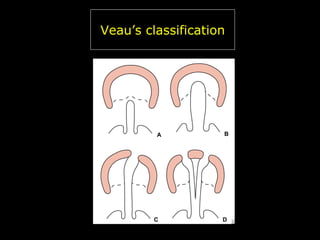
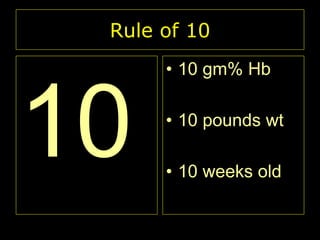
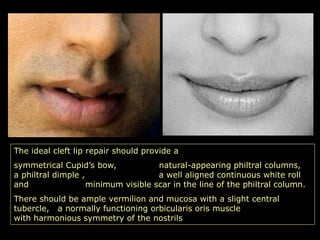
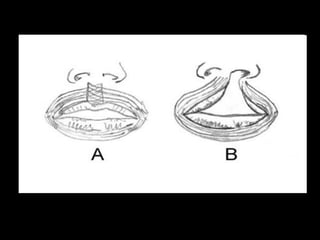
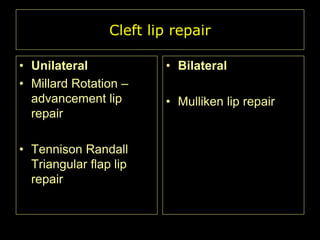
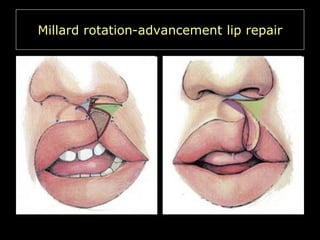
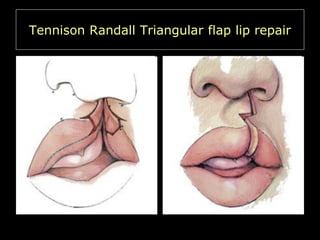
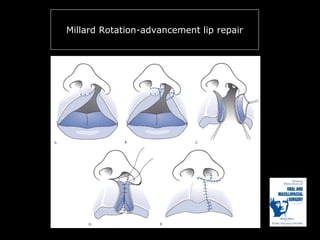
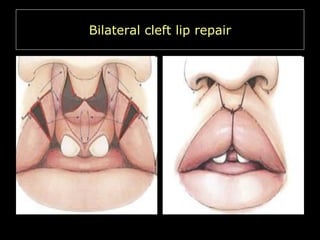
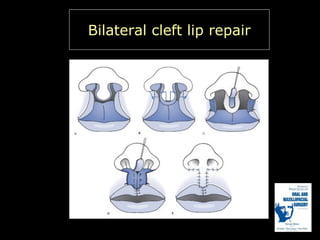
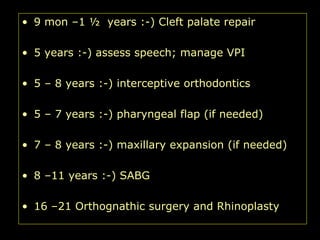
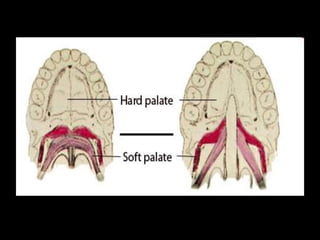
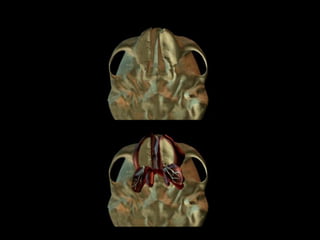
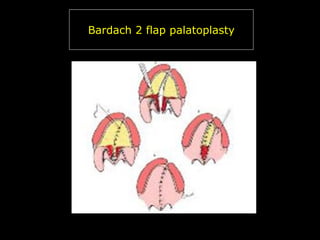
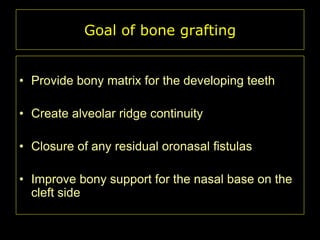
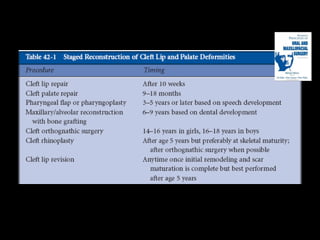
This presentation discusses cleft lip and palate, including the embryology, causes, problems experienced by patients, classification systems used, and principles and techniques for management and repair. It focuses on the development of the lip and palate in utero, factors that can cause cleft deformities like genetics and environmental exposures. Management involves a multidisciplinary team and follows a timeline of prenatal diagnosis, birth evaluation, lip repair at 3-6 months, palate repair at 9-18 months, bone grafting at ages 8-11 years and other procedures.