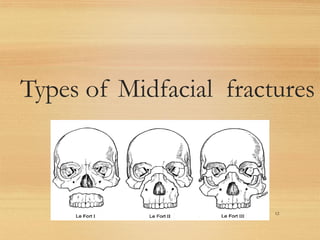
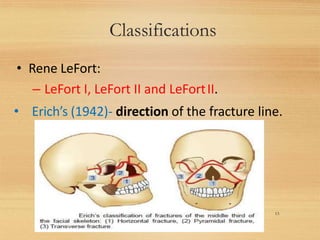
This document provides information on midfacial fractures, including the LeFort classifications. It describes:
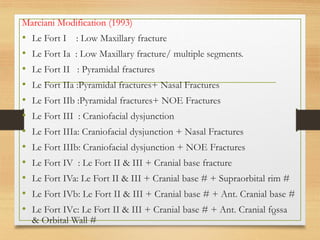
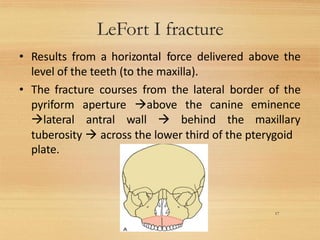
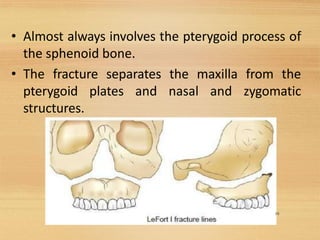
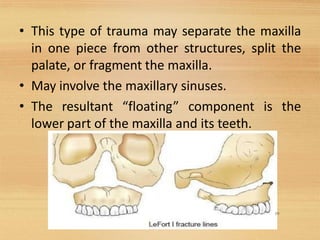
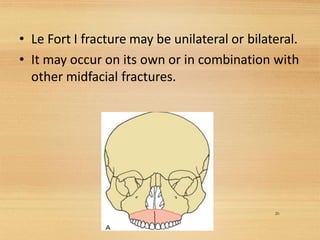
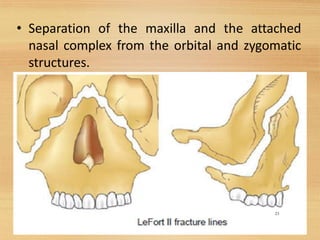
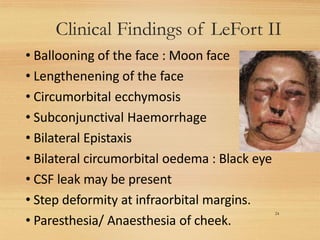
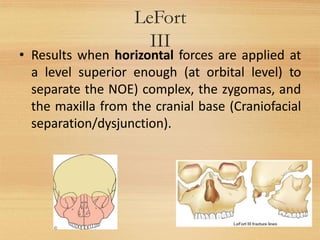
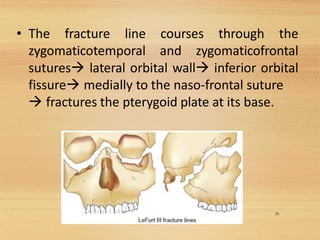
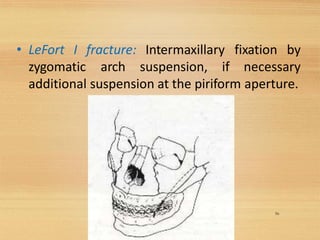
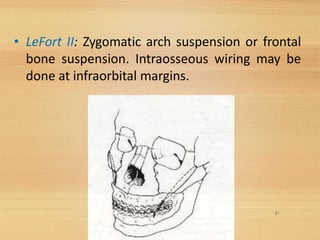
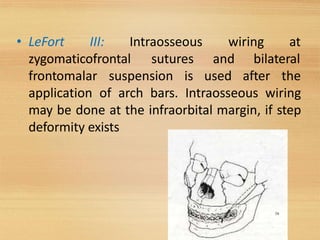
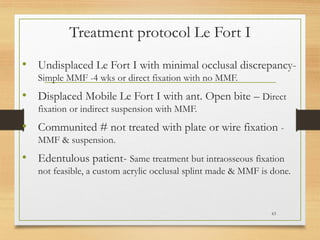
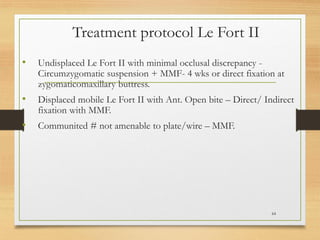
1) The LeFort I, II, and III fracture patterns involving the maxilla and midface bones. LeFort I involves the maxilla, LeFort II separates the midface, and LeFort III separates the entire midface from the skull.
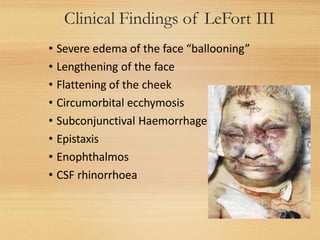
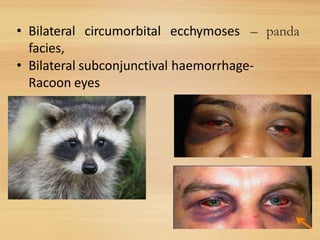
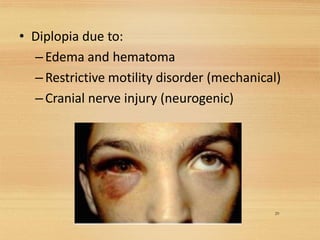
2) Clinical signs of each type include swelling, mobility of teeth, and malocclusion for LeFort I; moon face and raccoon eyes for LeFort II; and severe edema and flattening of the cheeks for LeFort III.
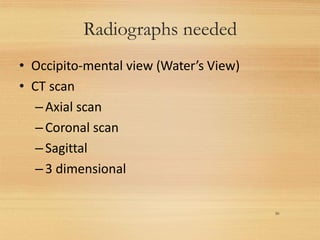
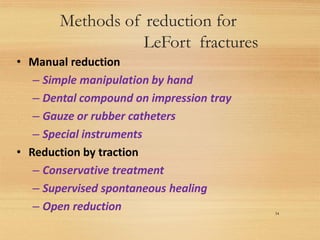
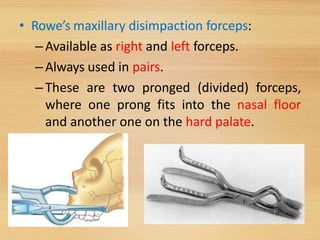
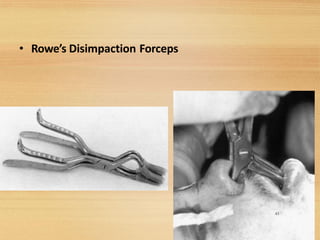
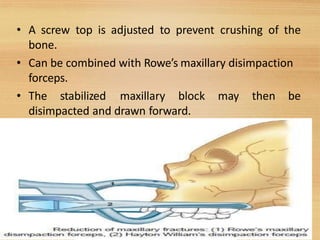
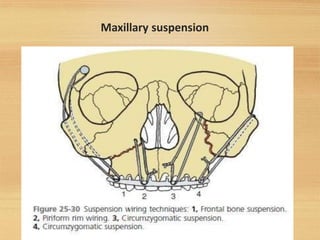
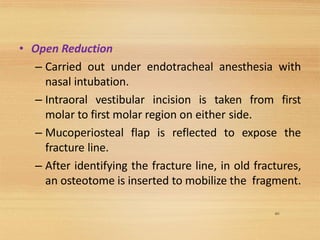
3) Treatment involves reducing and fixing the fractures, usually through closed or open reduction using manual manipulation or specialized instruments to re