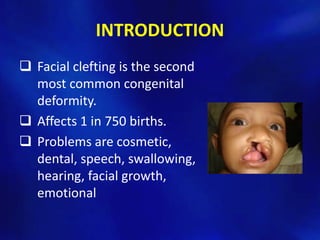
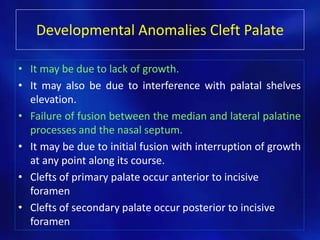
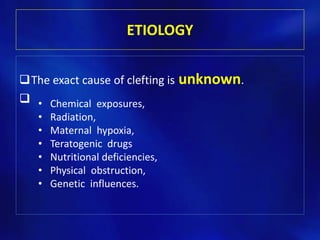
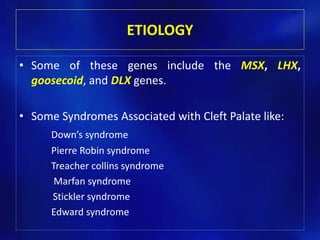
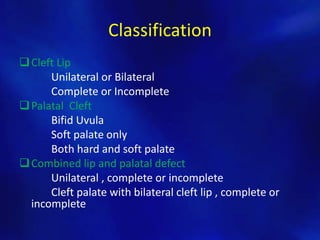
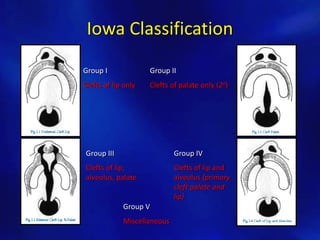
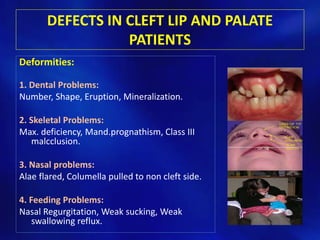
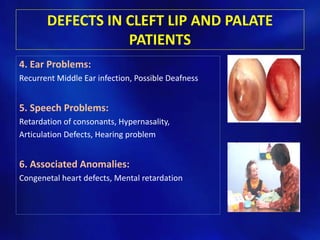
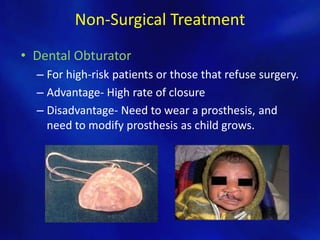
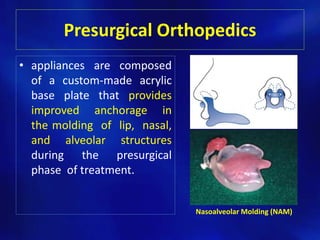
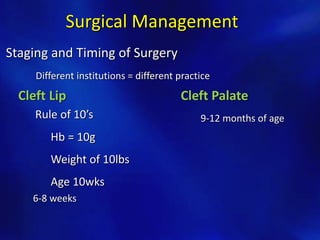
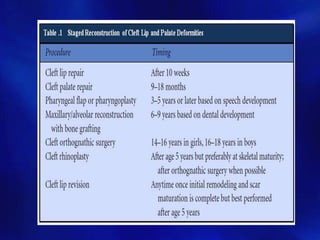
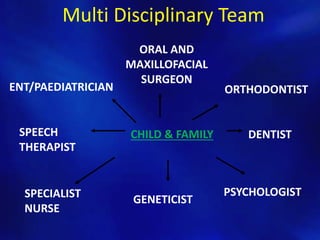
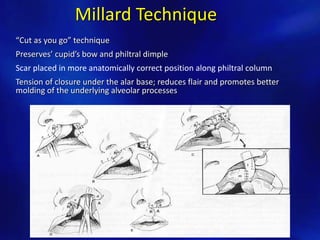
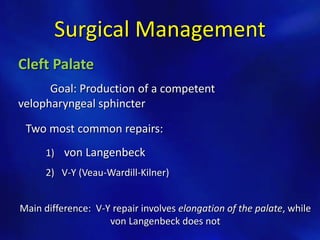
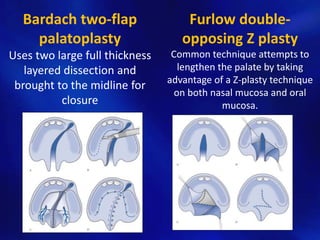
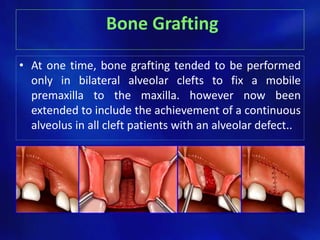
Cleft lip and palate is a birth defect where the tissue of the mouth and palate do not properly fuse together, leaving an opening in the lip and/or roof of the mouth. It affects 1 in 750 births and can cause problems with feeding, speech, dental issues, and facial growth. The document discusses the anatomy, development, causes, classification, and management of cleft lip and palate. Management involves a multi-disciplinary team and stages of surgery to repair the lip, palate, and other issues, as well as other treatments like dental appliances and bone grafts.