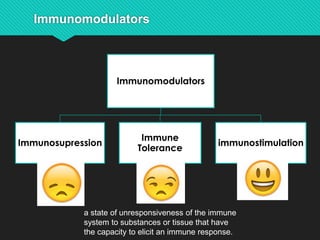
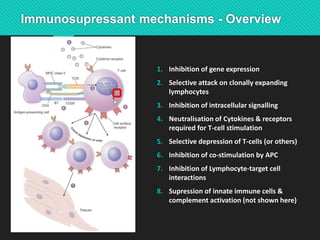
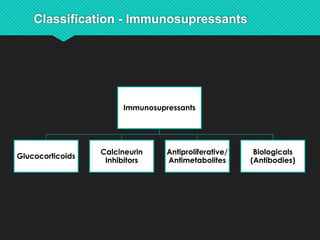
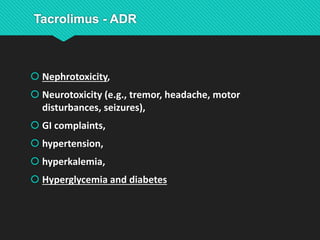
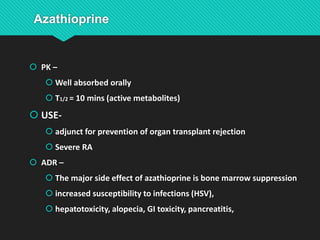
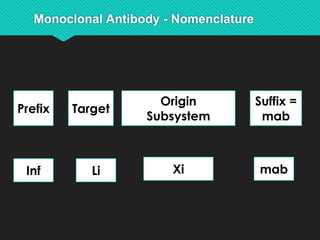
Immunomodulators can stimulate or suppress the immune system. There are several classes of immunomodulators including glucocorticoids, calcineurin inhibitors, antiproliferatives, and biologicals. Glucocorticoids have broad anti-inflammatory effects and work by binding to receptors that regulate gene transcription. Calcineurin inhibitors like tacrolimus and cyclosporine inhibit T cell activation. Antiproliferatives such as azathioprine, mycophenolate mofetil, and methotrexate inhibit lymphocyte proliferation. Biologicals include monoclonal antibodies that target specific molecules. Immunomodulators are used to prevent transplant rejection and treat autoimmune disorders but can have side