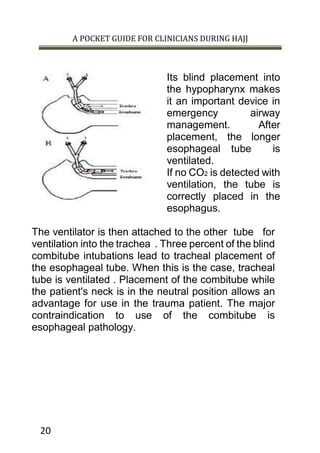
This document provides guidance on airway management for clinicians during Hajj. It discusses manual airway opening techniques like head tilt/chin lift and jaw thrust. Adjuncts like oropharyngeal and nasopharyngeal airways are also described. Definitive airways include endotracheal tubes, which require rapid sequence induction and confirmation of proper placement. Nasotracheal intubation and surgical airways like cricothyroidotomy are also summarized as alternatives when other methods fail or in specific injury cases. Maintaining a clear airway is a top clinical priority to allow for breathing and oxygenation.



![A POCKET GUIDE FOR CLINICIANS DURING HAJJ
28
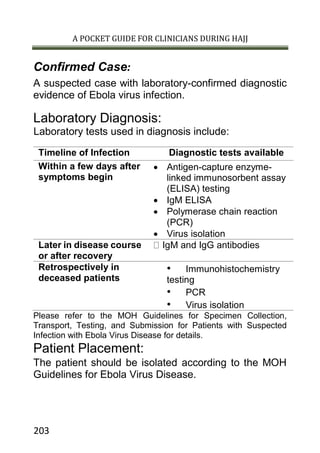
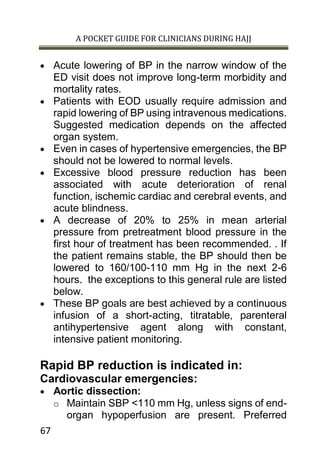
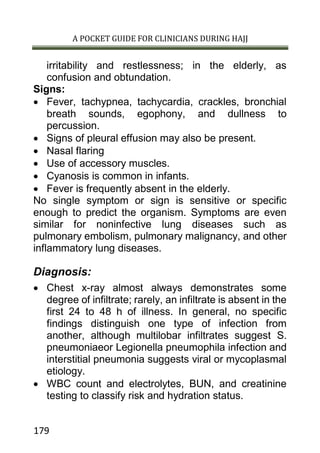
Acute respiratory failure
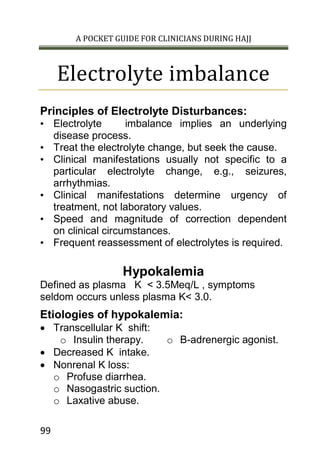
There are two types of respiratory failure:
Type I: the most common form of respiratory failure is
Hypoxemic respiratory failure which is characterized by a
PaO2 of less than 60 mm Hg with a normal or low PaCO2.
and it can be associated with all acute diseases of the lung,
which generally involve fluid filling or collapse of alveolar
units. Some examples of type I respiratory failure are
cardiogenic or noncardiogenic pulmonary edema,
pneumonia, and pulmonary hemorrhage.
type II : Hypercapnic respiratory failure is characterized
by a PaCO2 of more than 50 mm Hg. And commonly
associated with Hypoxemia, The pH depends on the level
of bicarbonate, which is dependent on the duration of
hypercapnia. Common etiologies include drug overdose,
neuromuscular disease, chest wall abnormalities, and
severe airway disorders (eg, asthma, chronic obstructive
pulmonary disease [COPD]).
Manifestations:
Altered mental status
Increased work of breathing
o Tachypnea
o Accessory muscle use, retractions, paradoxical
breathing pattern
Catecholamine release
o Tachycardia, diaphoresis, hypertension
Abnormal arterial blood gas values](https://image.slidesharecdn.com/hajjpocketguide-150613001804-lva1-app6892/85/Hajj-pocket-guide-29-320.jpg)

![A POCKET GUIDE FOR CLINICIANS DURING HAJJ
105
meq/L/hour, in 1st
few hours. Serum Na should not
exceed >12meq/24h.
• 1ml of 3% NaCl /kg/h - increase serum Na 1meq/l/h.
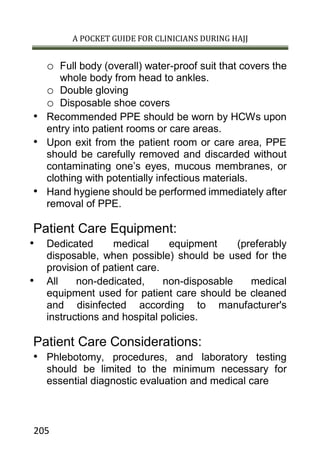
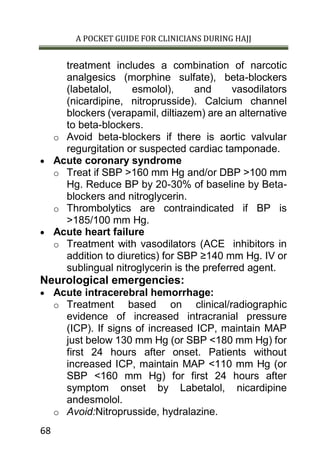
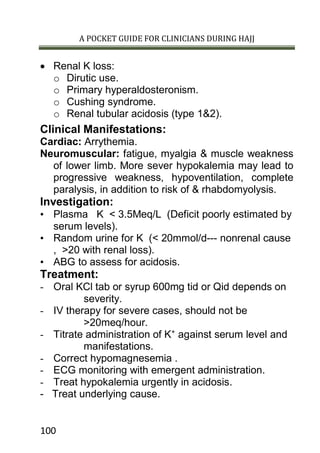
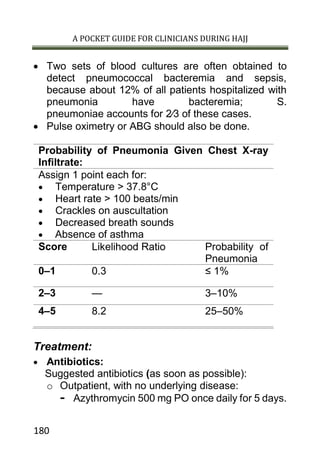
Hypernatremia
Defined as serum Na > 145meq/L.
Etiologies of hypernatremia:
Hyponatremia secondary to water loss (commonest
cause).
o Nonrenal water loss e.g. GIT loss , burn.
o renal water loss e.g. osmotic dieresis like in
hyperglycemia , Manitol & Diabetes inspidus (
CDI,NDI).
Impaired thirst:
o Intubated patient in ICU.
o Patient with impaired mental status.
o Physically handicapped.
Hyponatremia due to Na gain:
o In Patient with DKA &osmotic dieresis treated
with N saline.
o Treatment with IV NaHCO3 during resuscitation.
Manifestations:
• Mainly neurological include altered mental status,
weakness, Coma& seizure.
• H2O deficit (L) =[0.6 wt (kg) ] [measured Na - 1]140
Treatment:
• Stop ongoing water loss.
• Correct water deficit.](https://image.slidesharecdn.com/hajjpocketguide-150613001804-lva1-app6892/85/Hajj-pocket-guide-106-320.jpg)
![A POCKET GUIDE FOR CLINICIANS DURING HAJJ
108
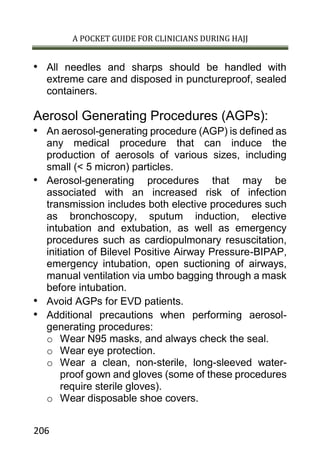
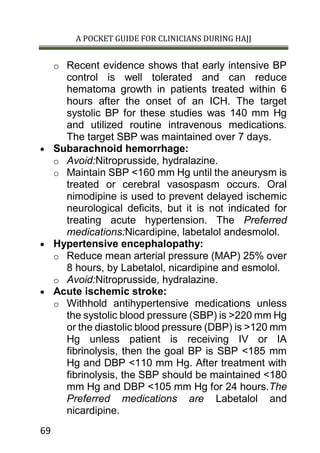
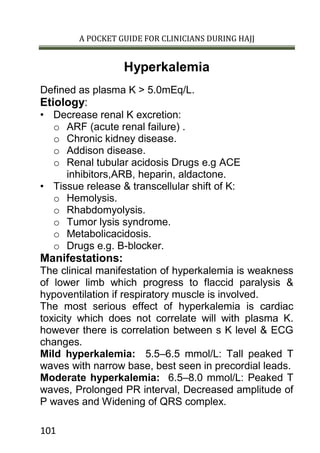
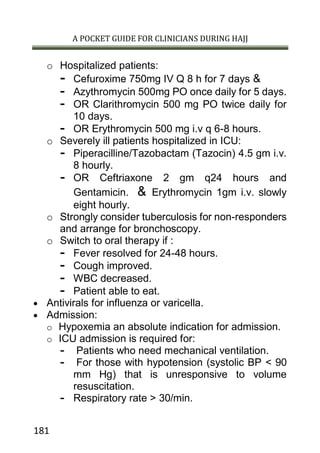
Normal anion gap : 9 ± 3 mEq /L
Reveal additional information on albumin level.
Note that an AG acidosis can exist even when the AG
is normal; this is particularly true in critically ill
patients with low albumin.
Expected AG decreases by 2.5-3 mmol/L for
every 1 g/dL decrease in albumin
Calculate the delta gap if a metabolic acidosis is
present.
Δgap = (deviation of AG from normal)– (deviation
of [HCO3] from normal)
Accurate analysis should lead to early interventions.
Metabolic Acidosis
Mechanisms:
Increased acid intake orIncreased acid production,
so, exceeding renal acid excretion (e.g. ketoacidosis
or lactic acidosis).
Renal acid excretion fails to match endogenous acid
production (e.g Renal Tubular Acidosis).
Decreased bicarbonate by GIT loss (e.g. diarrhea or
fistula).
Types of metabolic acidosis:
Normal anion gap metabolic acidosis:
o Causes:
- RTA (Renal Tubular Acidosis).
- Loss of HCO3- from GIT as in :
- Diarrhea - Uretral diversion
- ileostomy.](https://image.slidesharecdn.com/hajjpocketguide-150613001804-lva1-app6892/85/Hajj-pocket-guide-109-320.jpg)



![A POCKET GUIDE FOR CLINICIANS DURING HAJJ
202
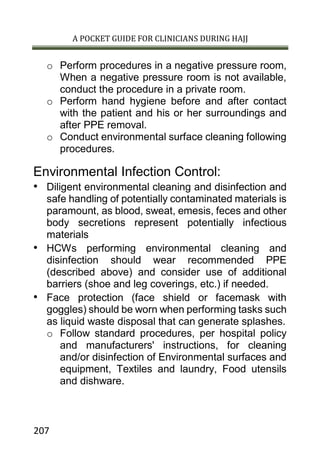
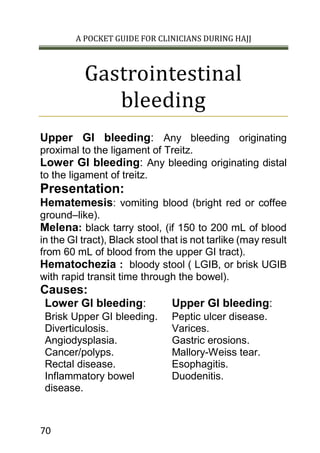
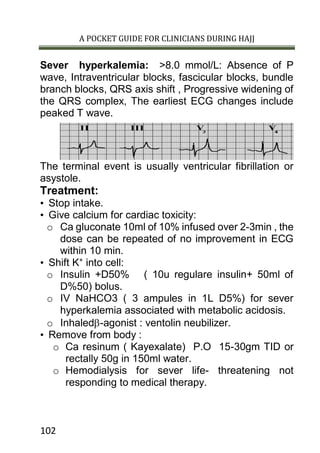
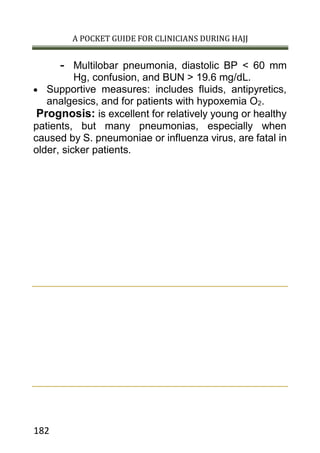
Ebola Virus Disease
(EVD)
Case Definition for Ebola Virus Disease:
Suspected Case:
Illness in a person who has both consistent symptoms
and risk factors as follows:
Clinical criteria, which includes fever of greater than
38.6O
C, and additional symptoms such as severe
headache, muscle pain, vomiting, diarrhea, abdominal
pain, or unexplained hemorrhage (gingival, nasal,
cutaneous [petechiae, bruises, ecchymosis],
gastrointestinal, rectal [gross or occult blood], urinary
[gross or microscopic hematuria], vaginal, or puncture
sites bleeding); AND Epidemiologic risk factors within
the past 3 weeks before the onset of symptoms, such as
contact with blood or other body fluids of a patient
known to have or suspected to have EVD; residence
in—or travel to—an area where EVD transmission is
active; or direct handling of dead or alive fruit bats,
monkeys, chimpanzees, gorillas, forest antelope and
porcupines from disease-endemic areas. Malaria
diagnostics should also be a part of initial testing
because it is a common cause of febrile illness in
persons with a travel history to the affected countries.](https://image.slidesharecdn.com/hajjpocketguide-150613001804-lva1-app6892/85/Hajj-pocket-guide-203-320.jpg)