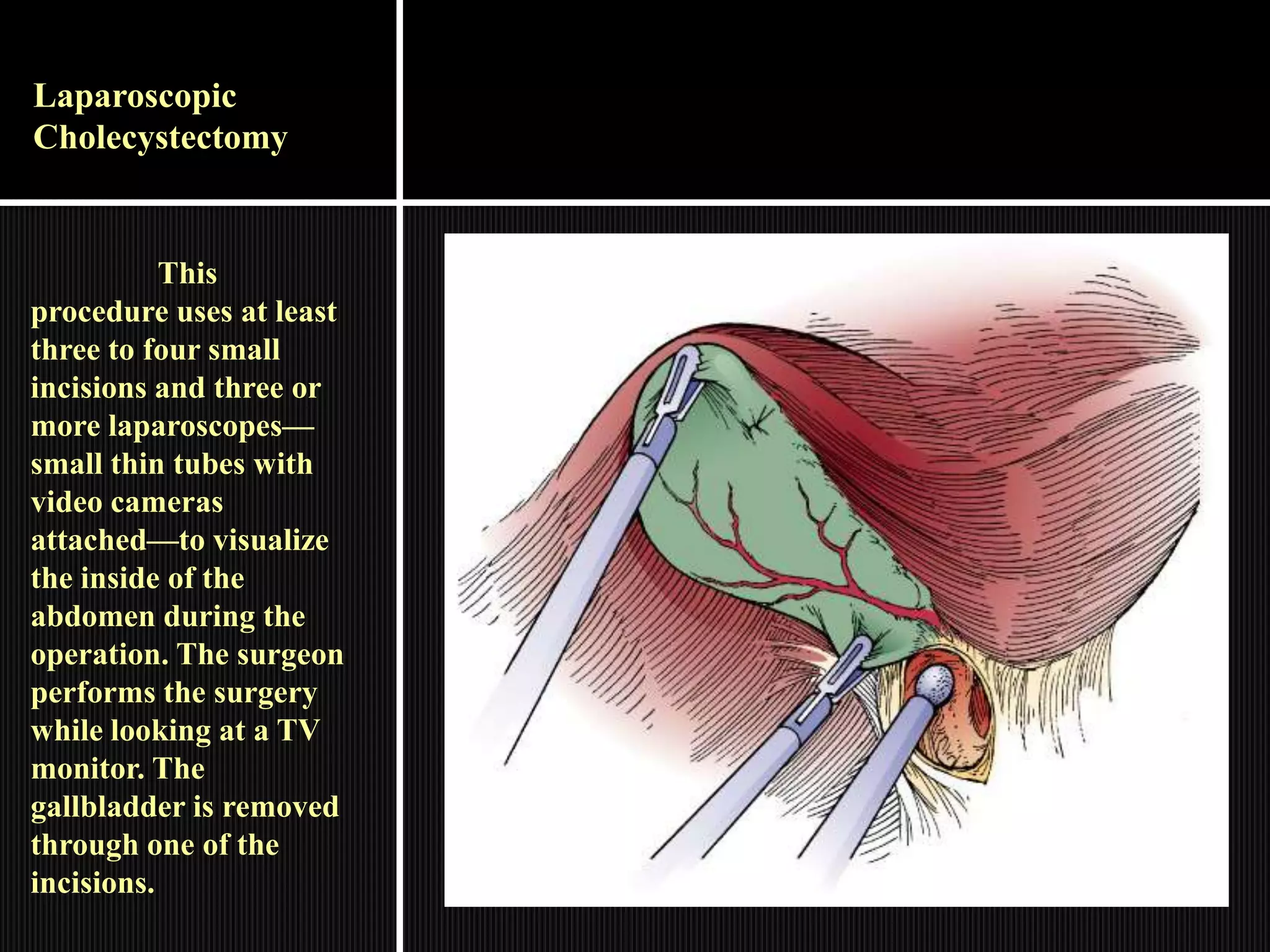
A cholecystectomy involves the surgical removal of the gallbladder. The gallbladder stores and concentrates bile produced by the liver to aid in fat digestion. Cholecystectomy is commonly performed to treat gallstones and related complications like gallbladder inflammation. The surgery can be performed through traditional open surgery or through laparoscopic methods involving small incisions. Conditions that may require open rather than laparoscopic cholecystectomy include severe inflammation, abdominal lining inflammation, liver cirrhosis, late-stage pregnancy, or bleeding disorders.


































![Risk factors may include
Losses from NG aspiration, vomiting
Medically restricted intake
Altered coagulation, e.g., reduced
prothrombin, prolonged coagulation time
Possibly evidenced by
[Not applicable; presence of signs and symptoms
establishes an actual diagnosis.]
Desired Outcomes
Display adequate fluid balance as evidenced by
stable vital signs, moist mucous
membranes, good skin turgor/capillary refill, and
individually appropriate urinary output.](https://image.slidesharecdn.com/cholecystectomy-140106003024-phpapp01/75/Cholecystectomy-39-2048.jpg)



