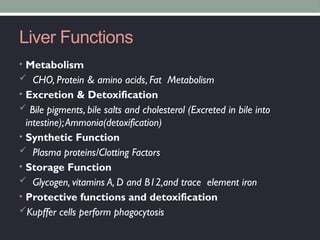
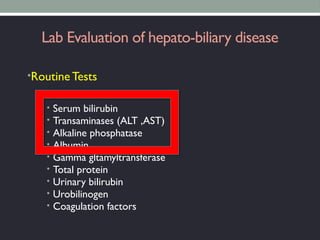
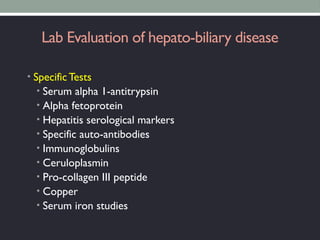
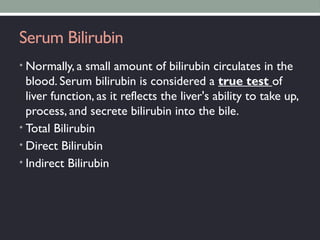
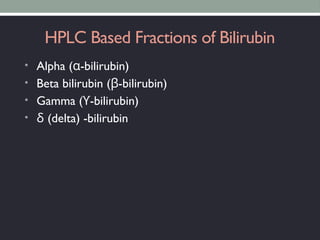
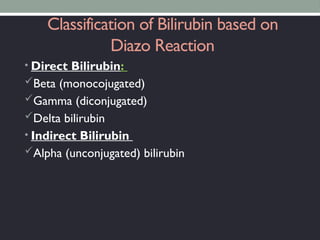
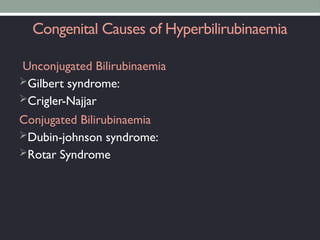
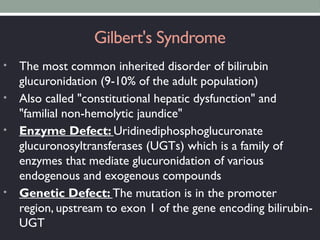
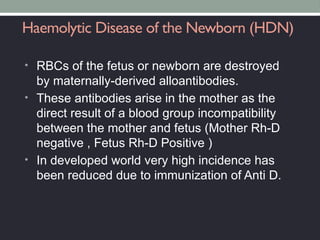
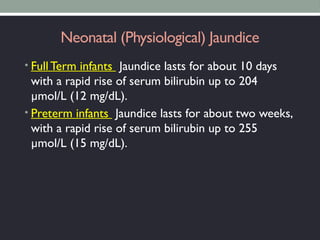
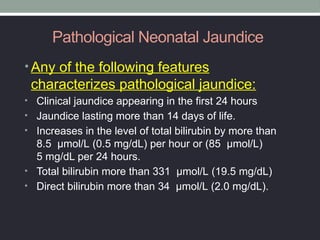
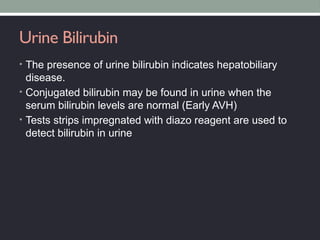
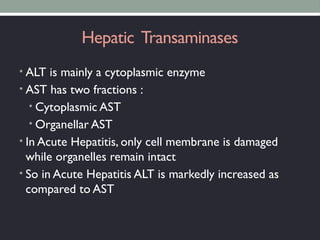
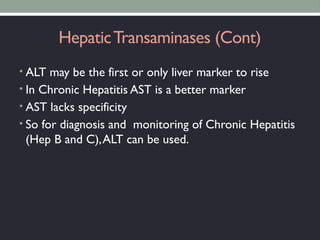
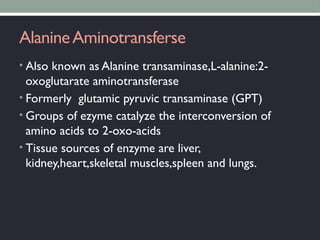
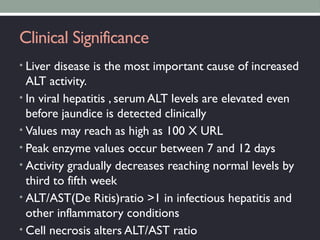
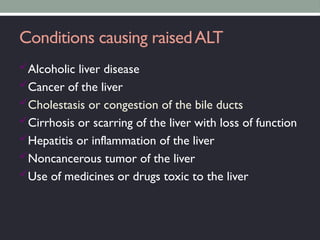
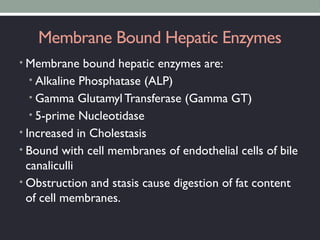
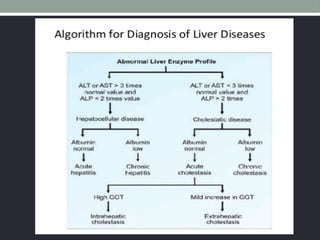
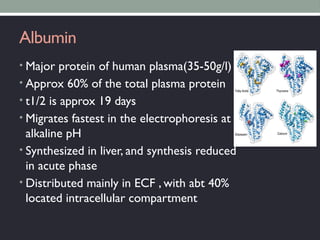
The document outlines liver function tests (LFTs) and their significance in evaluating liver health, covering its metabolic, excretory, synthetic, storage, and protective functions. It describes various laboratory tests for diagnosing hepatobiliary diseases, including serum bilirubin levels and liver enzymes, while highlighting conditions leading to liver dysfunction. Additionally, it addresses congenital bilirubin disorders and the importance of interpreting specific biochemical tests in assessing liver damage and function.