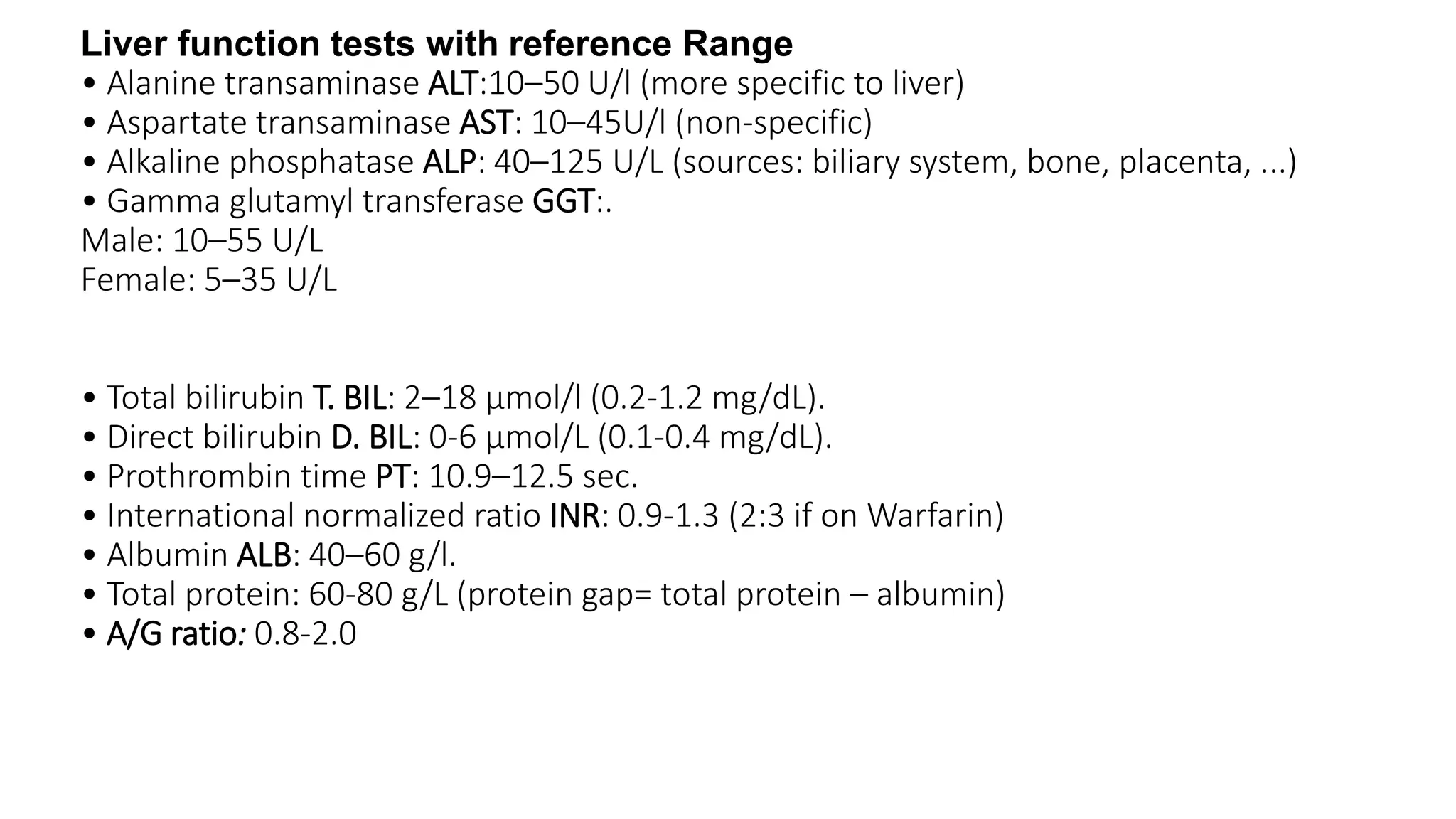
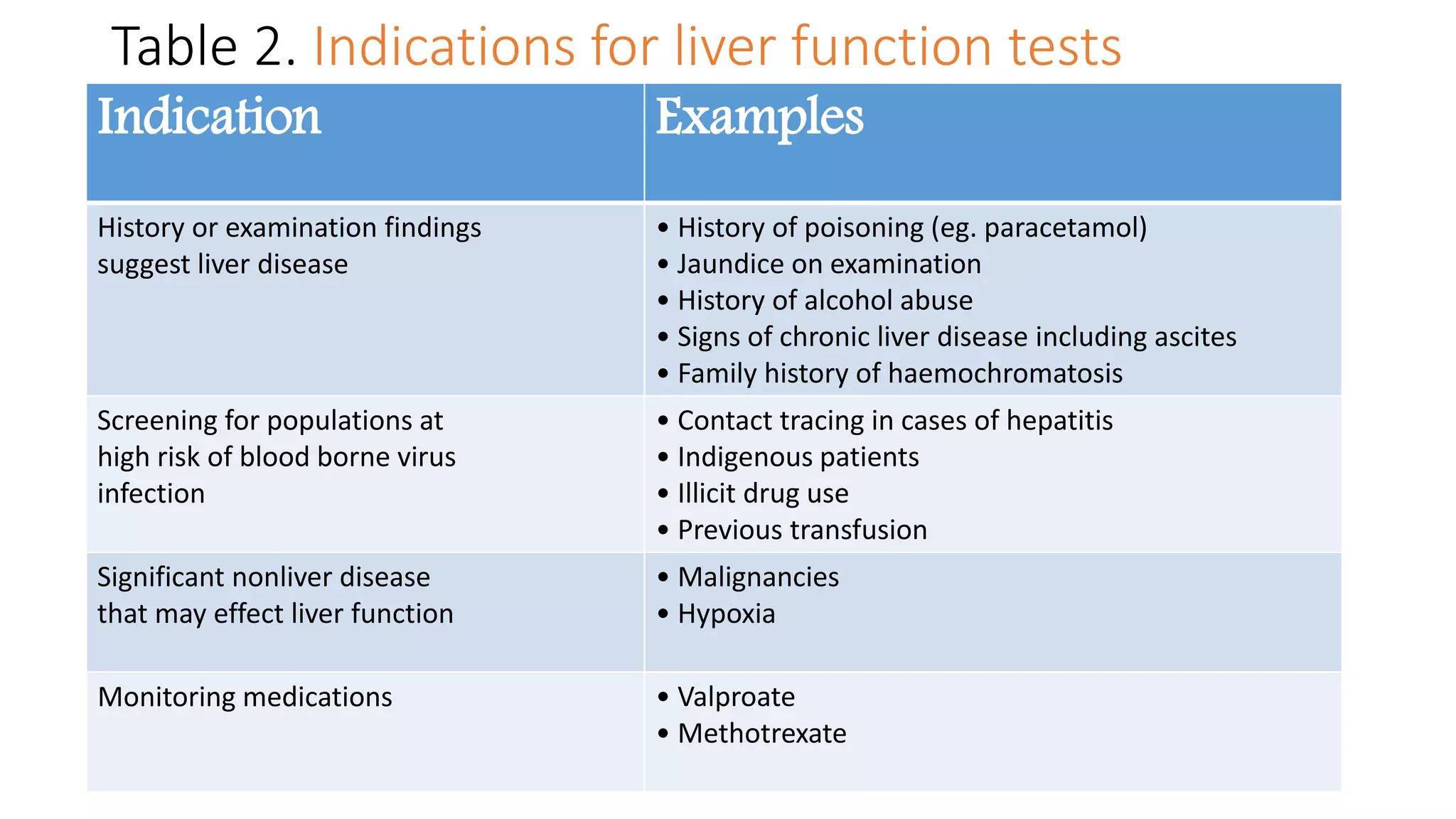
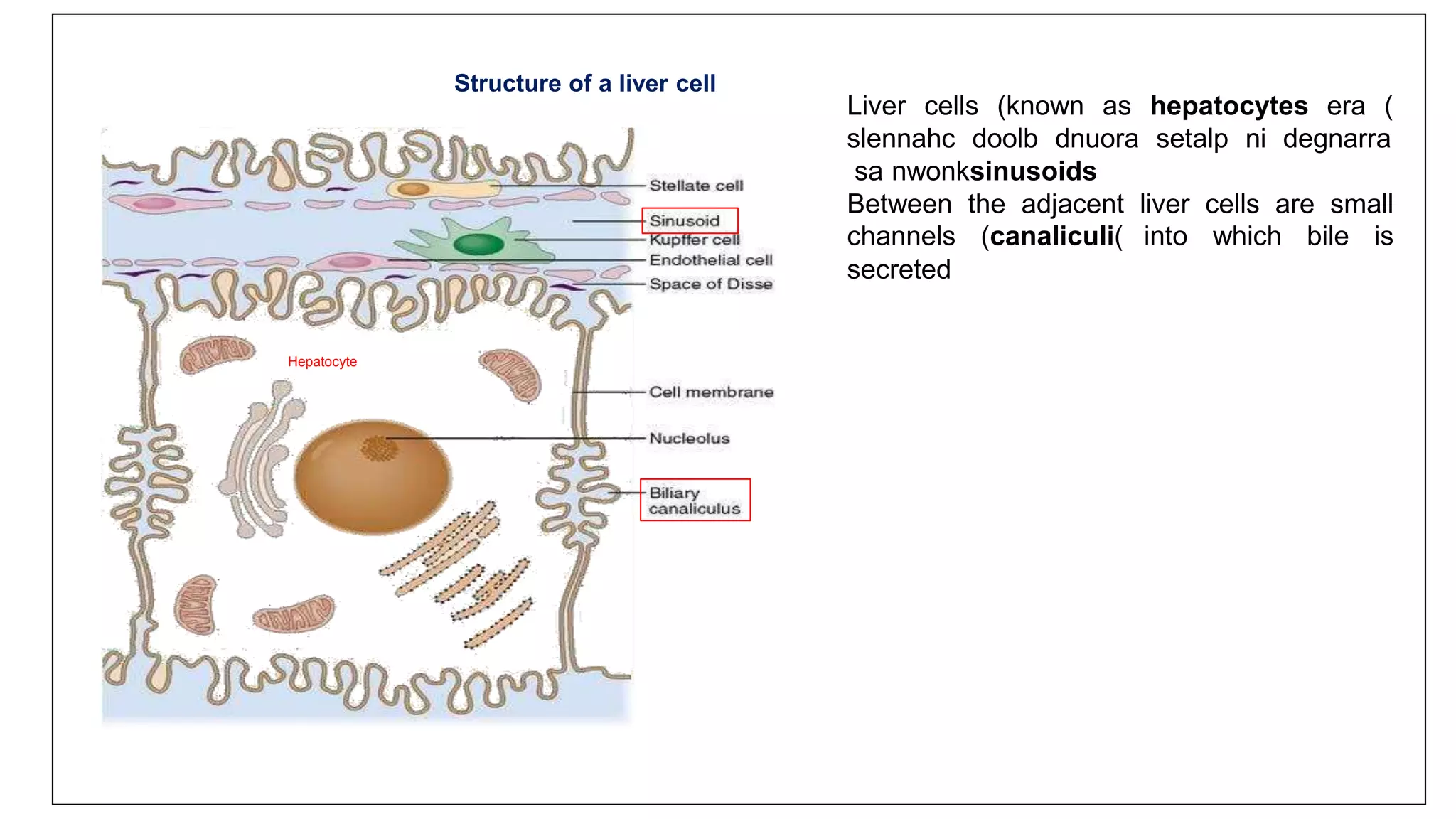
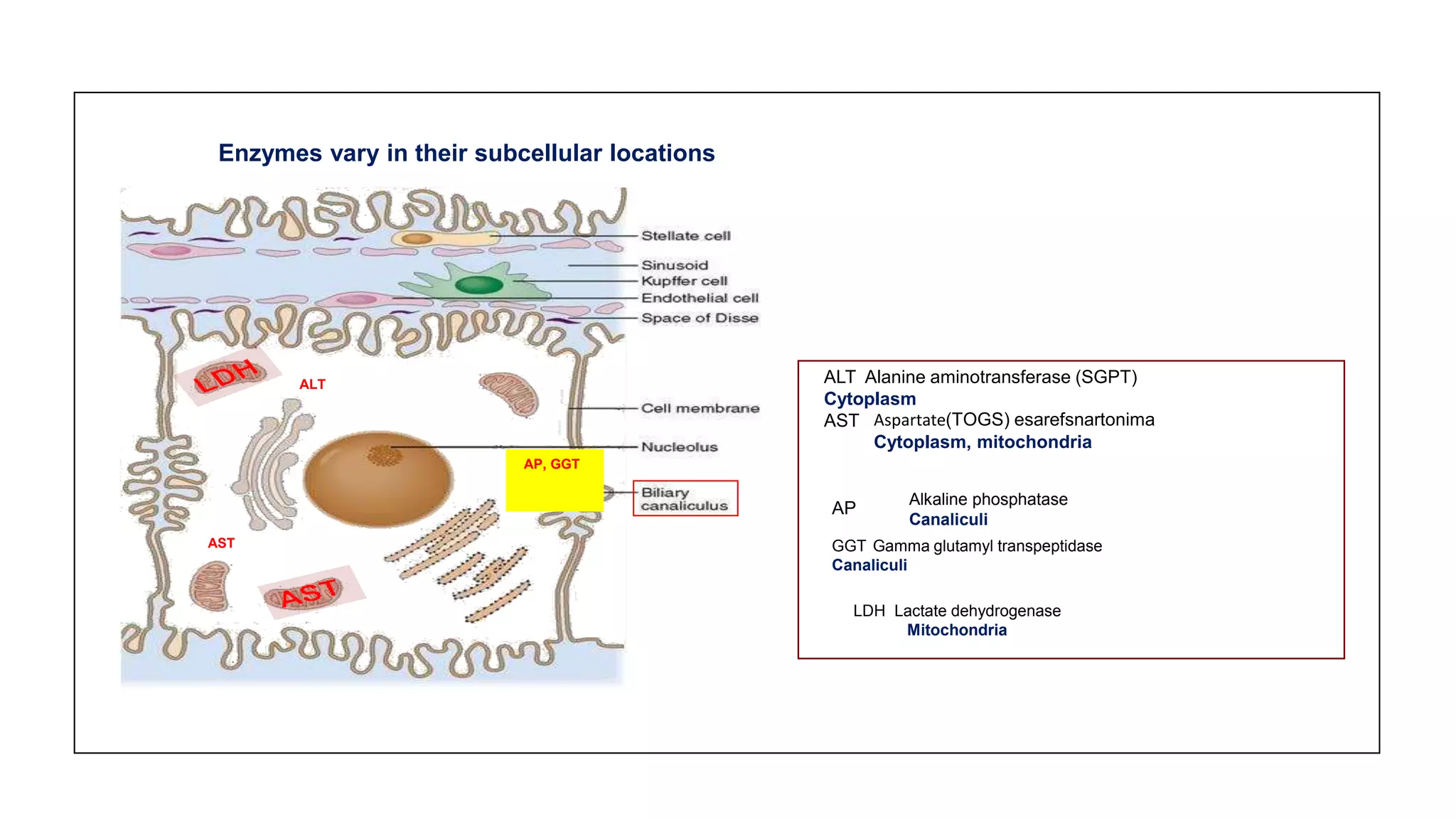
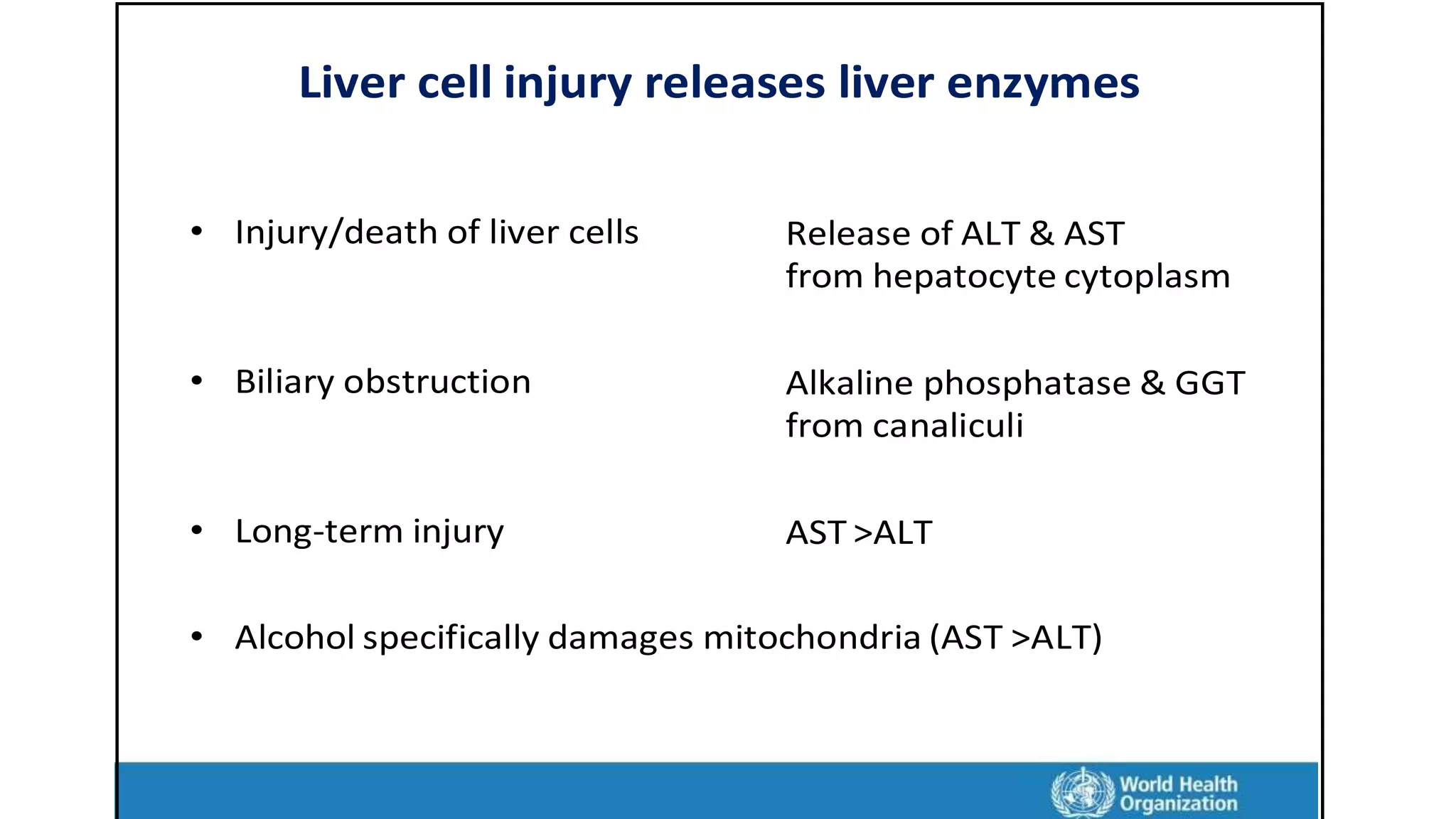
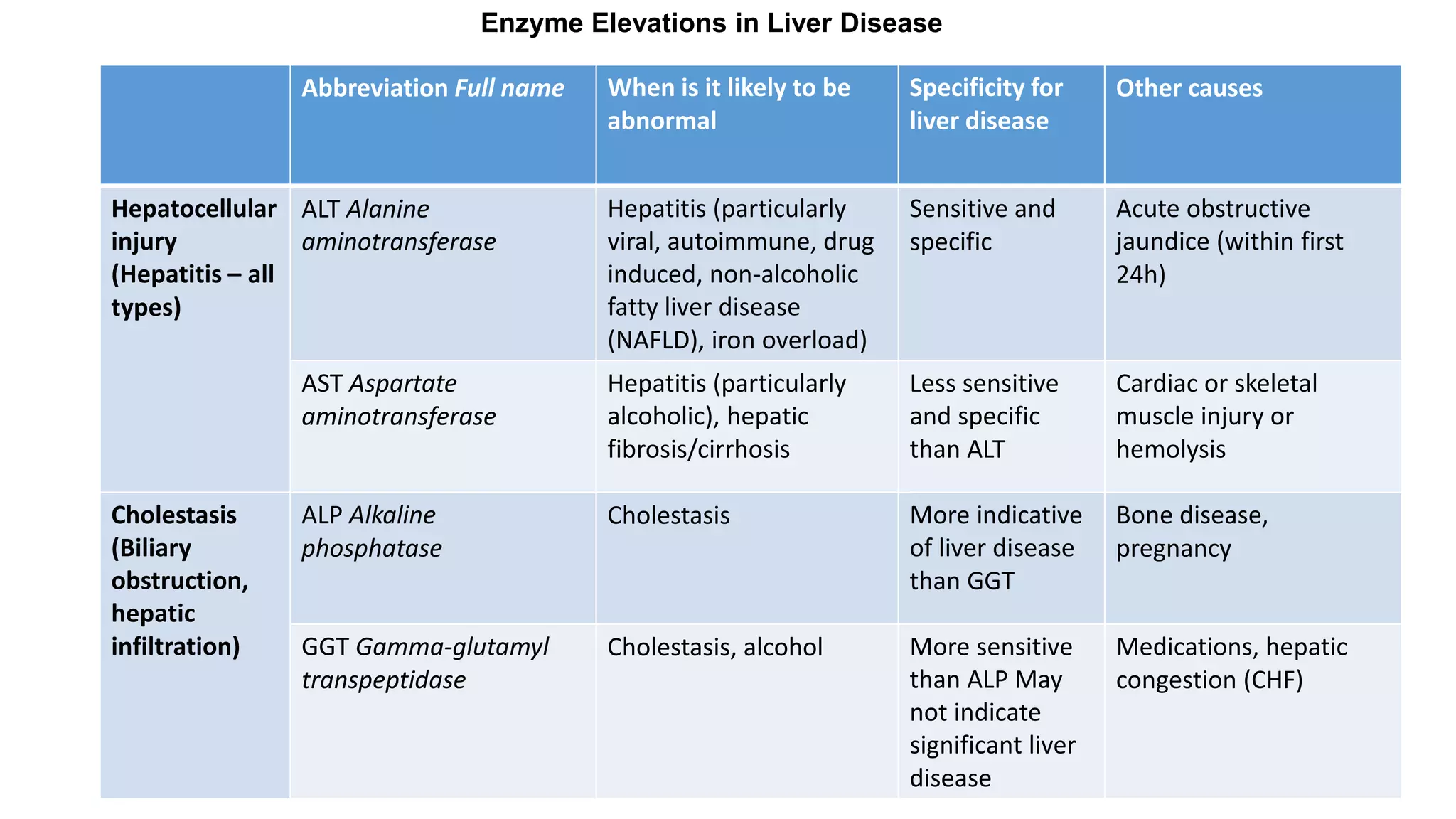
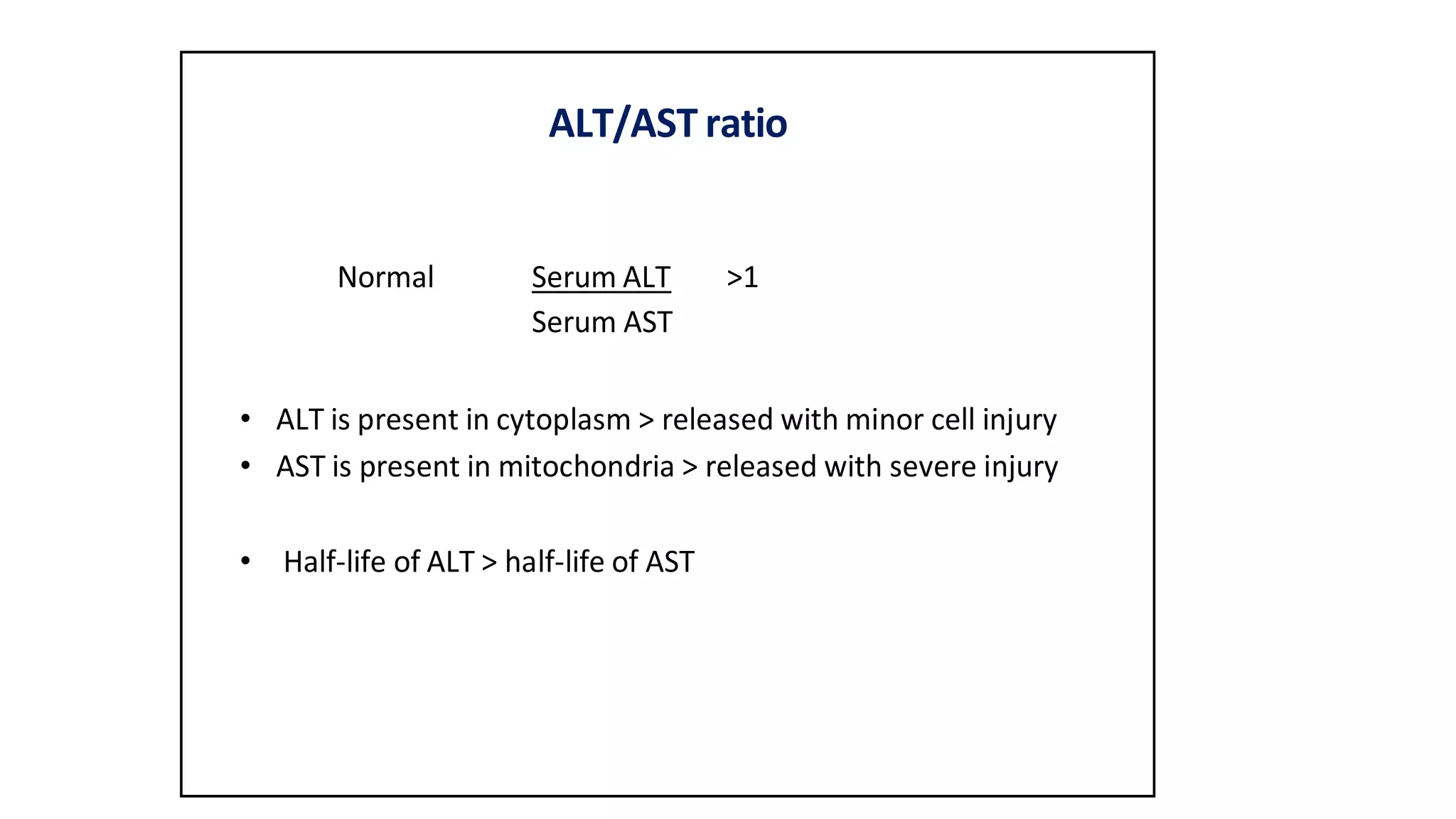
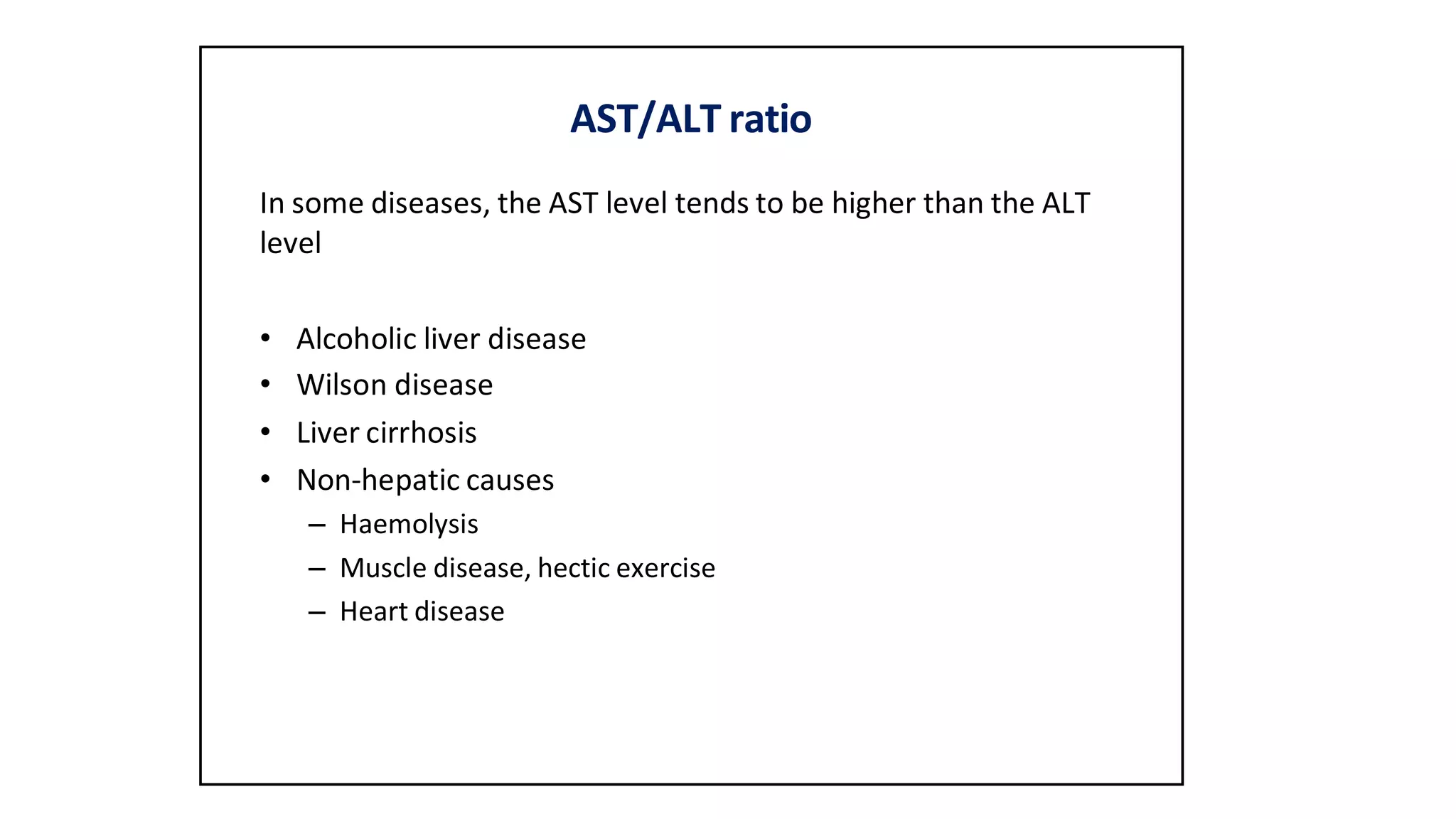
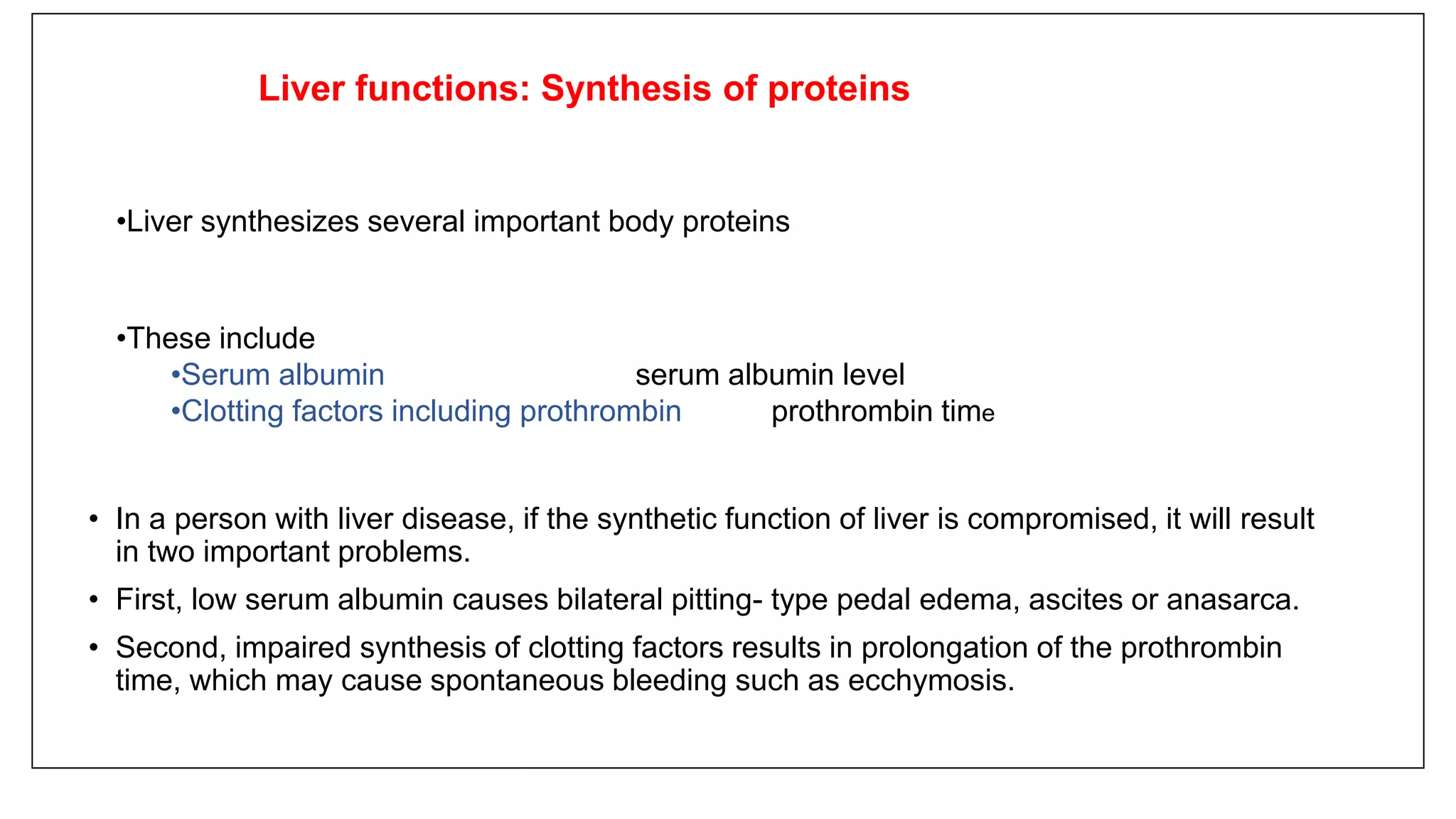
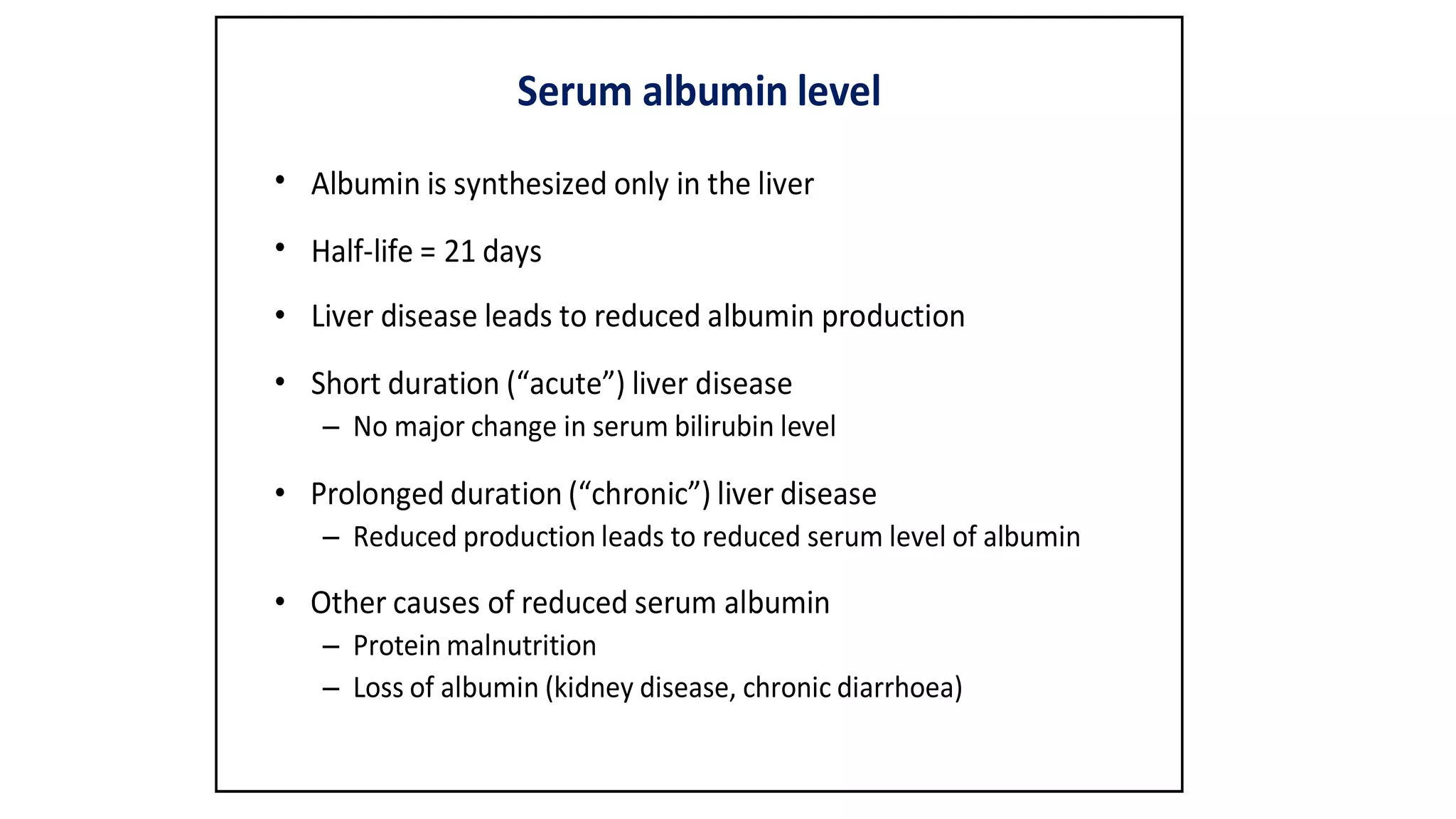
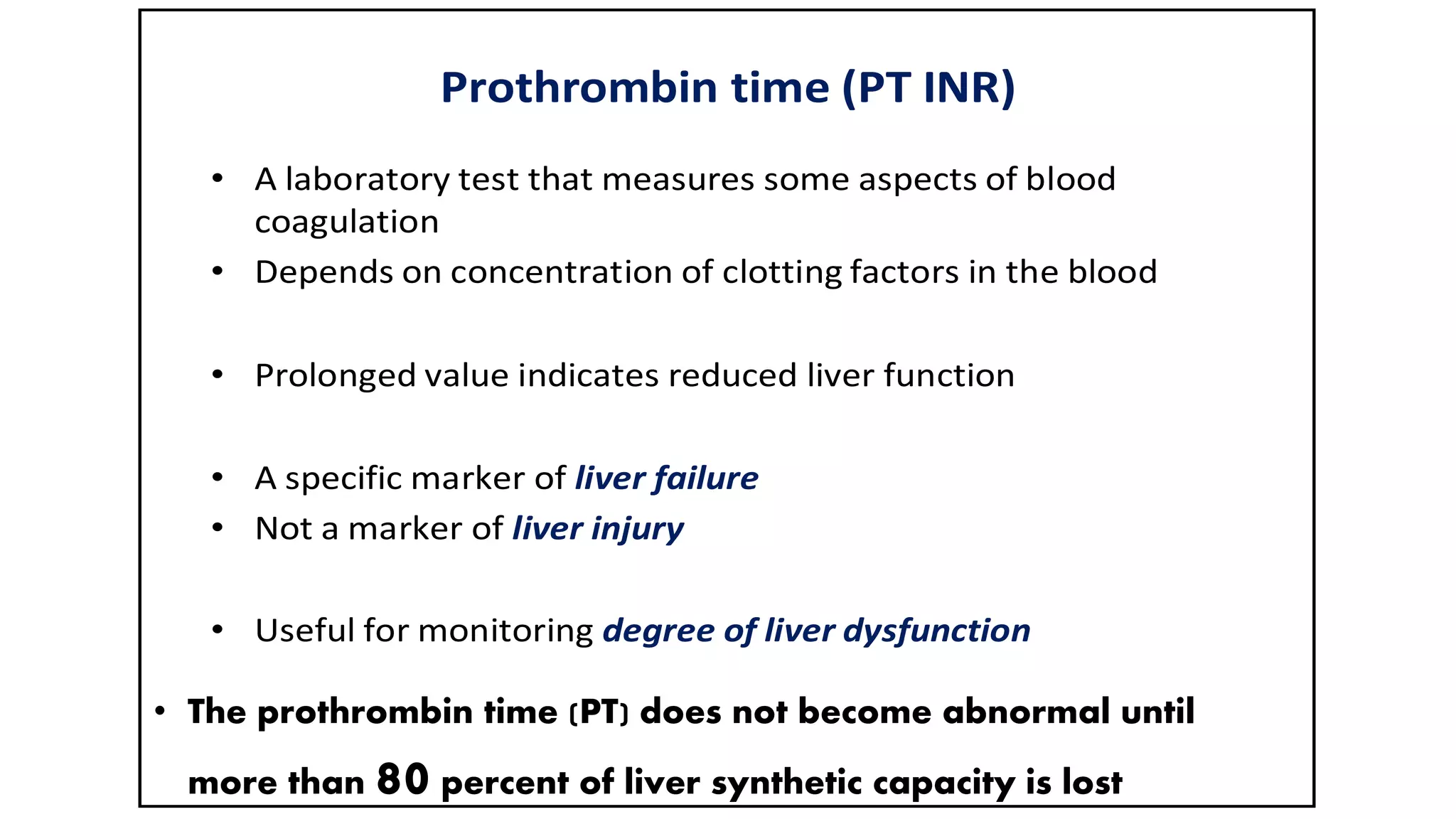
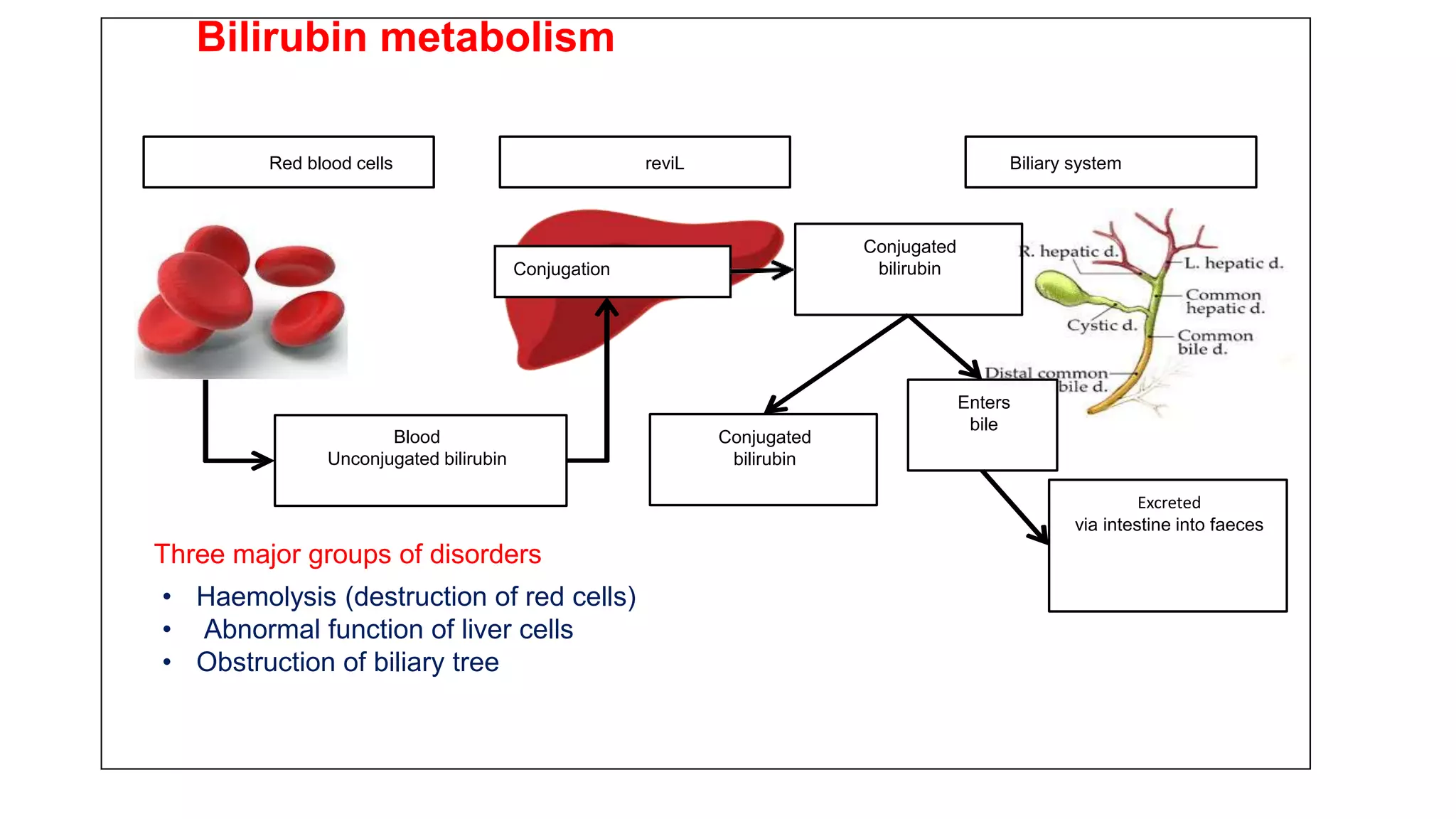
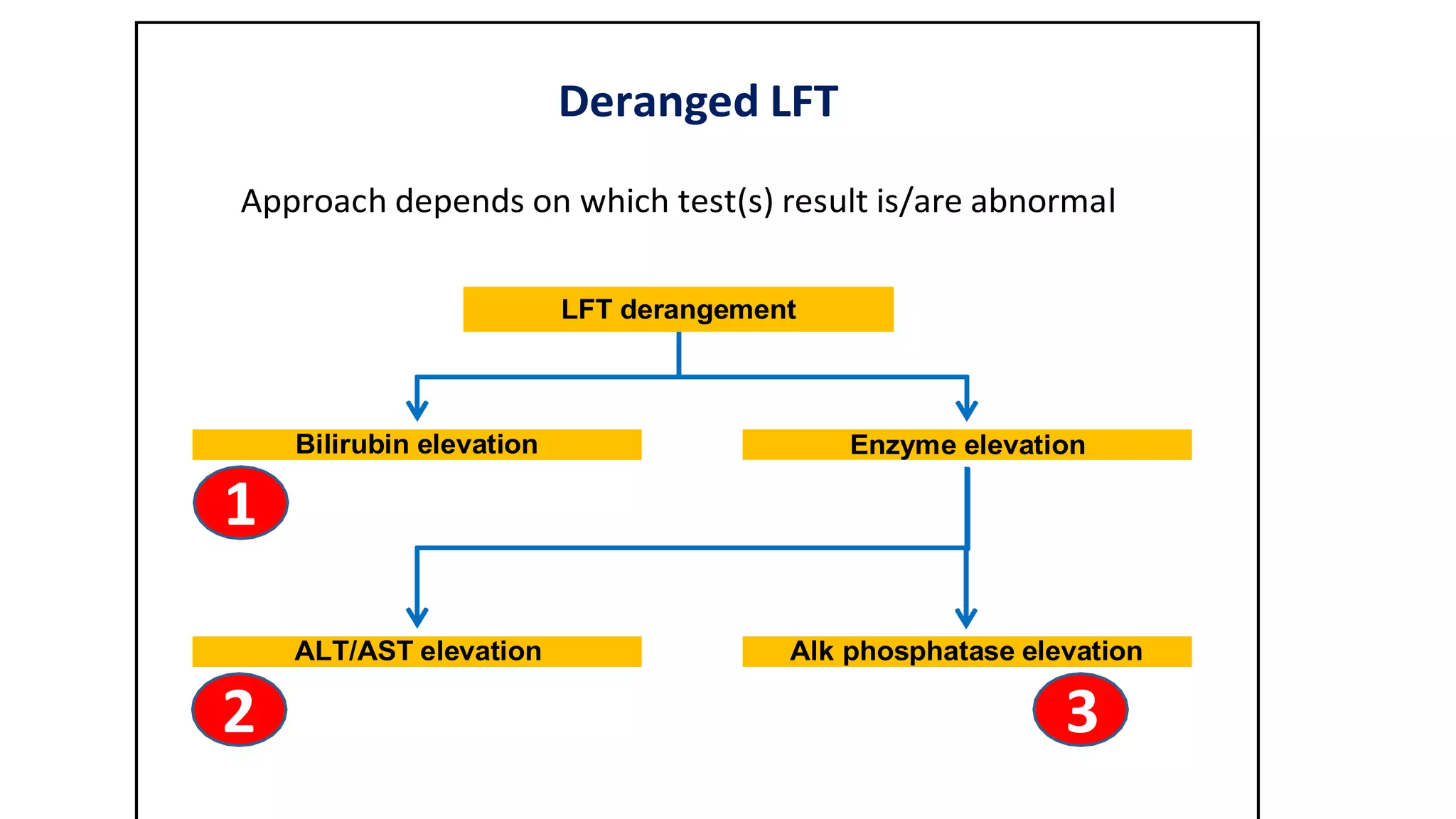
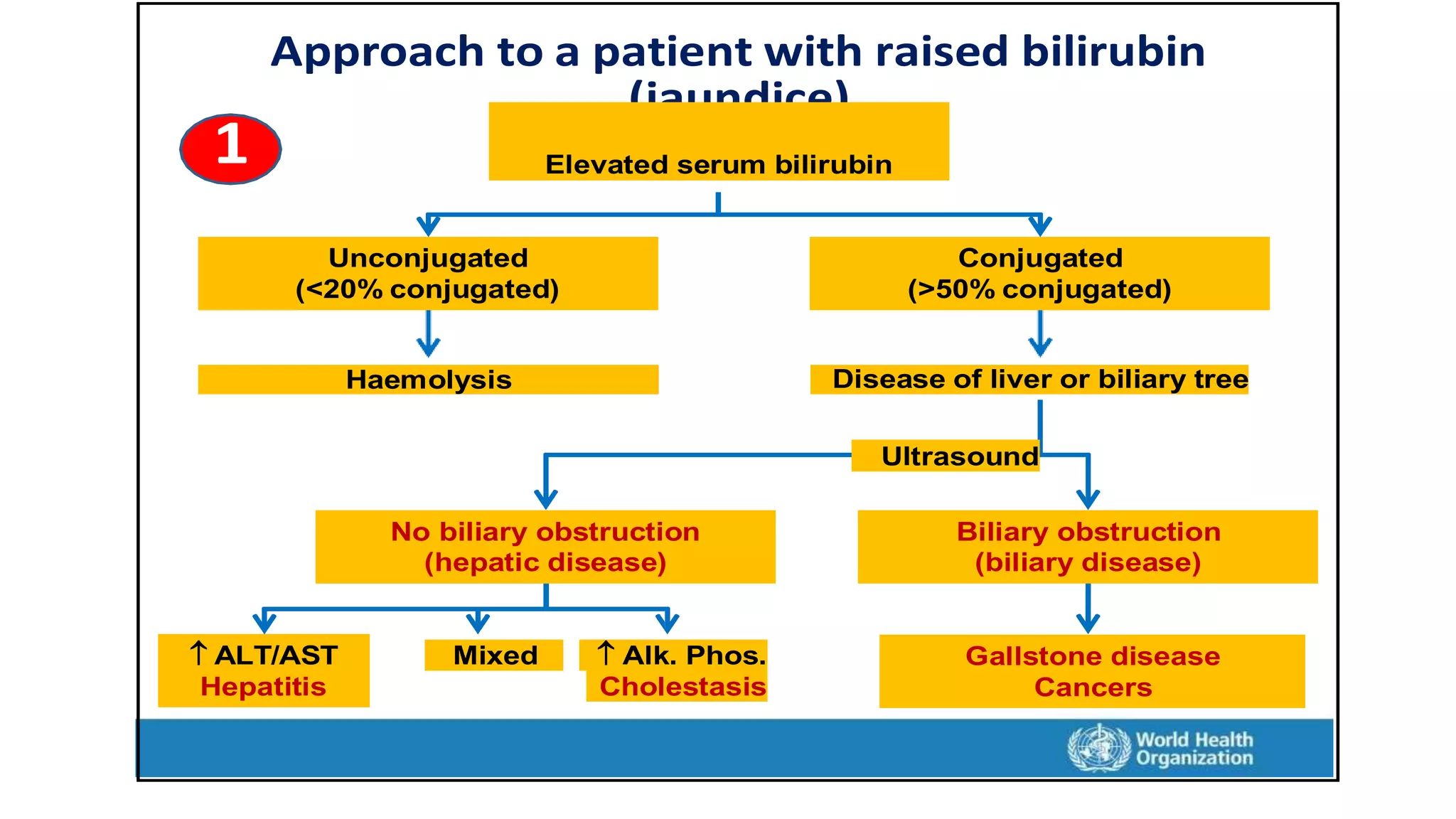
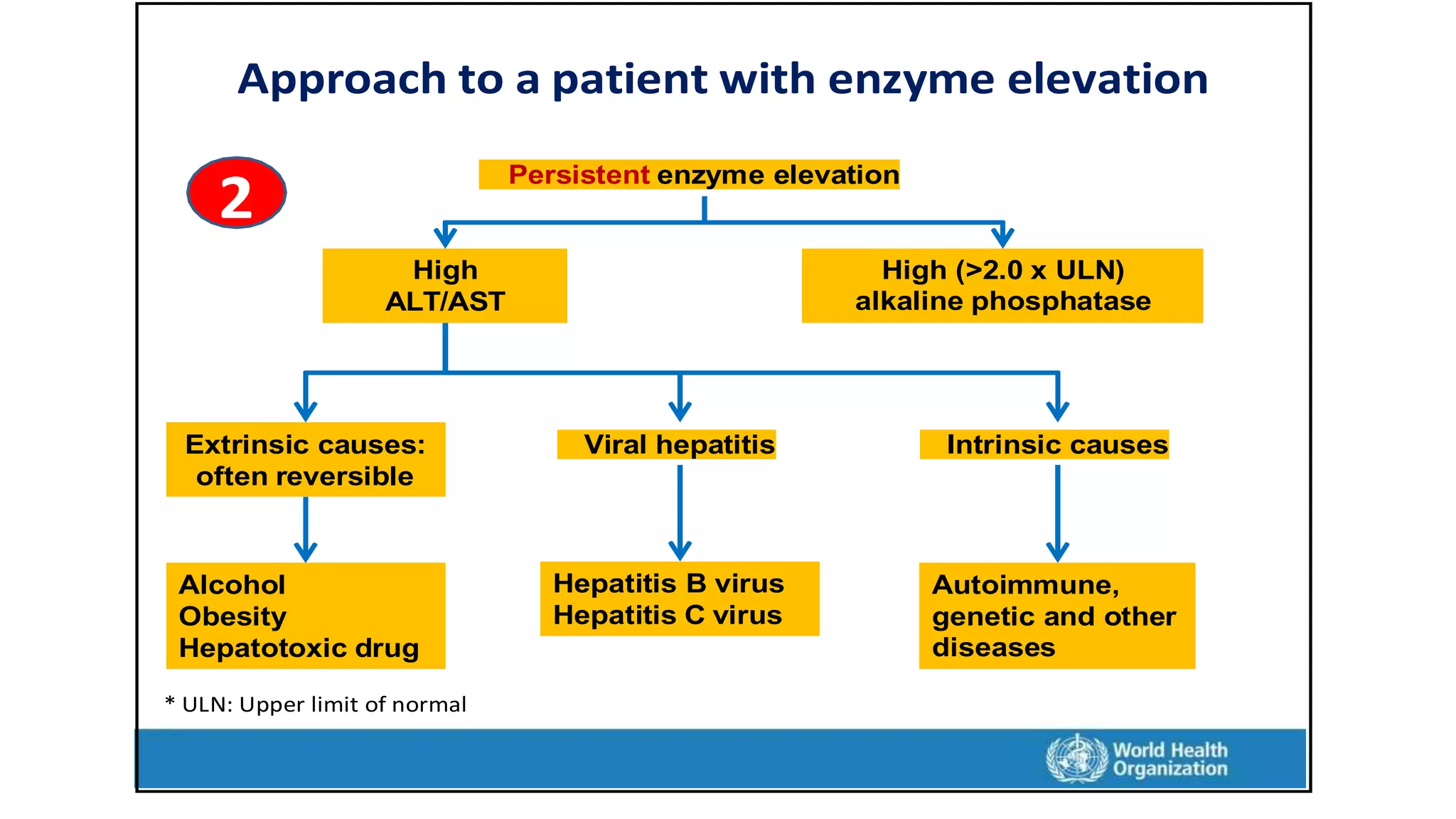
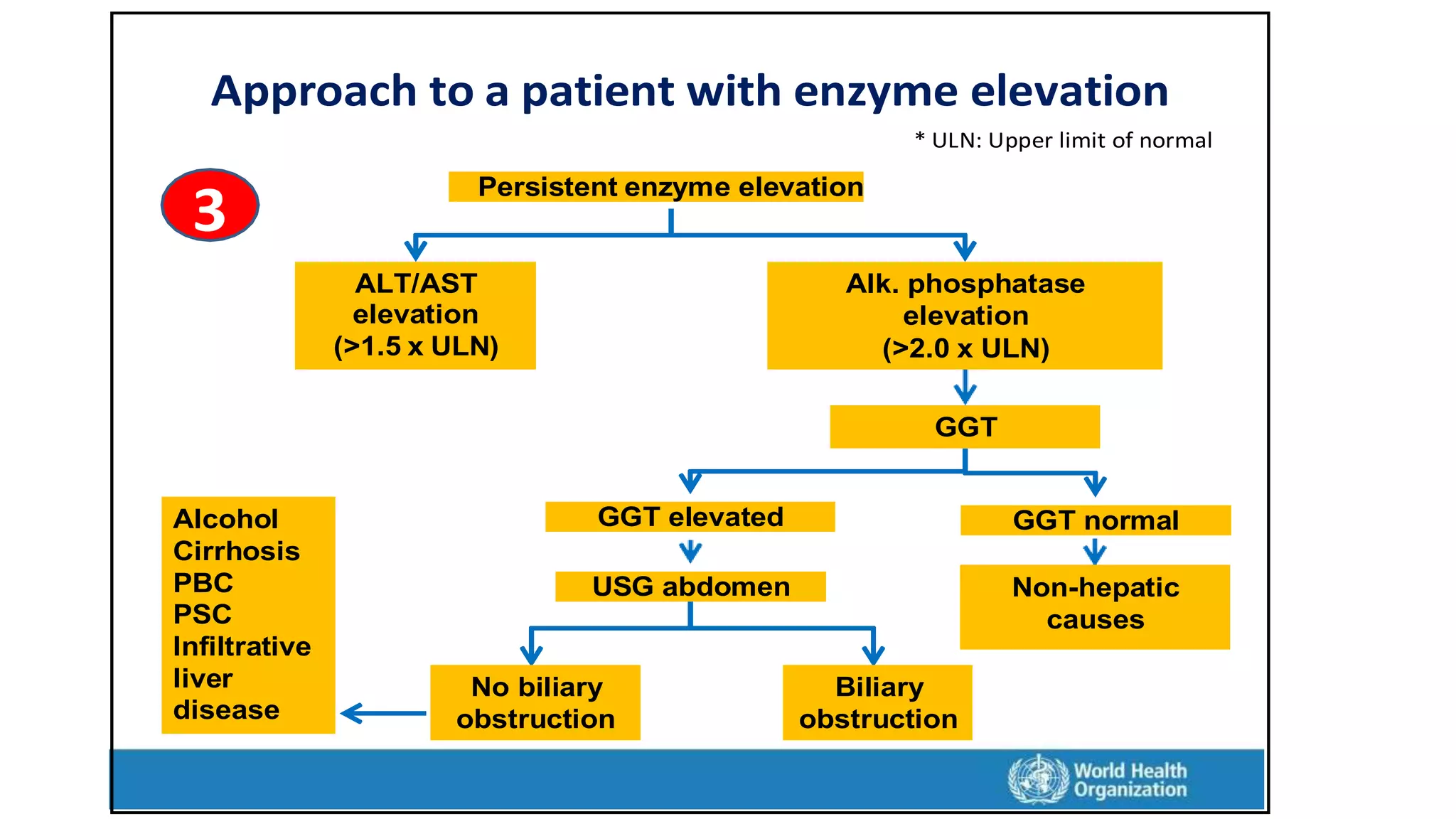
This document provides an overview of liver function tests, including definitions, normal ranges, and indications. It discusses the various types of liver enzymes and what each evaluates, such as ALT and AST for hepatocellular damage and alkaline phosphatase and GGT for cholestasis. Approaches to abnormal liver function test results are also covered, examining elevated bilirubin, enzymes, and the ratios between different values to determine the underlying cause of liver disease or damage.