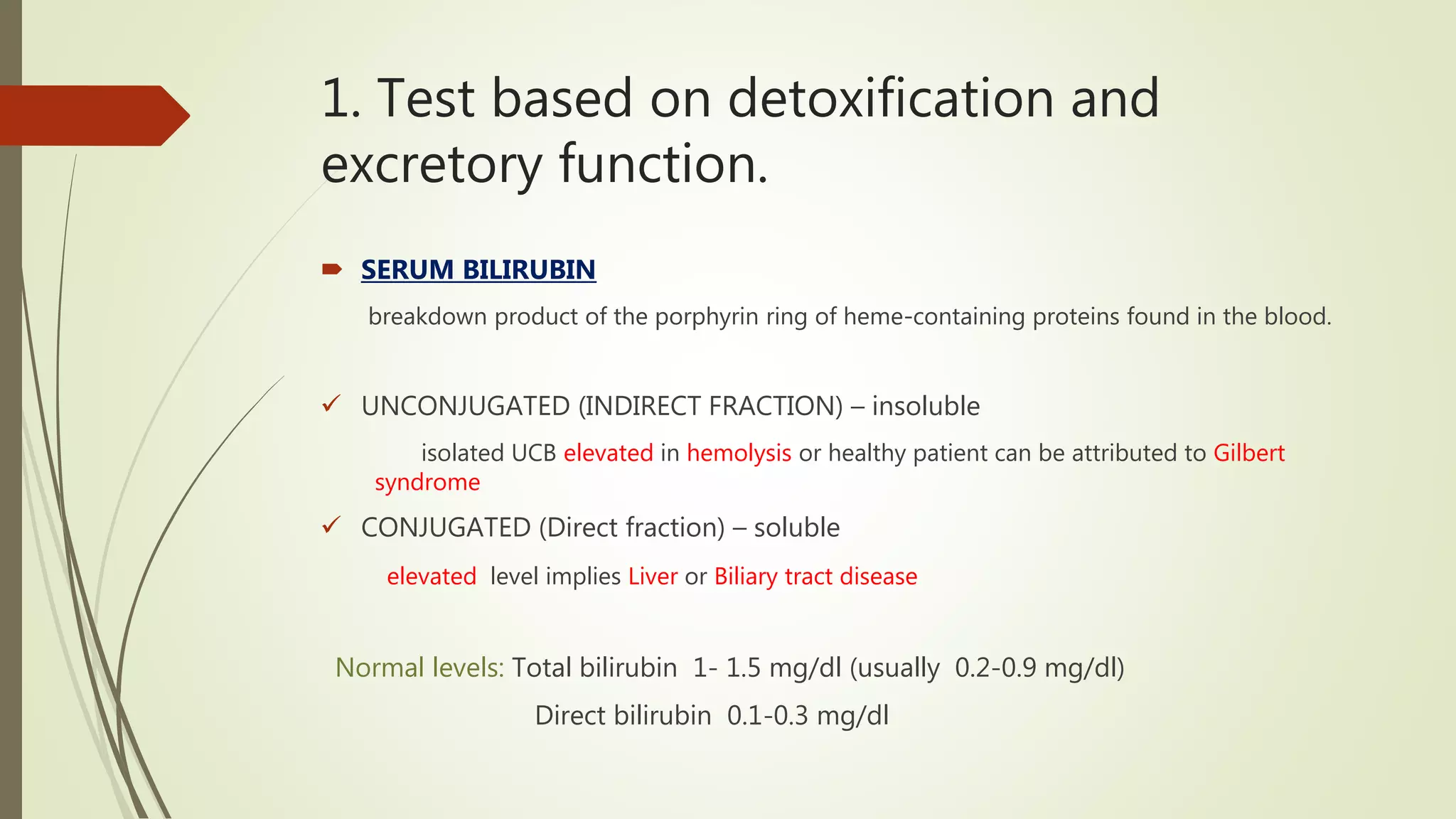
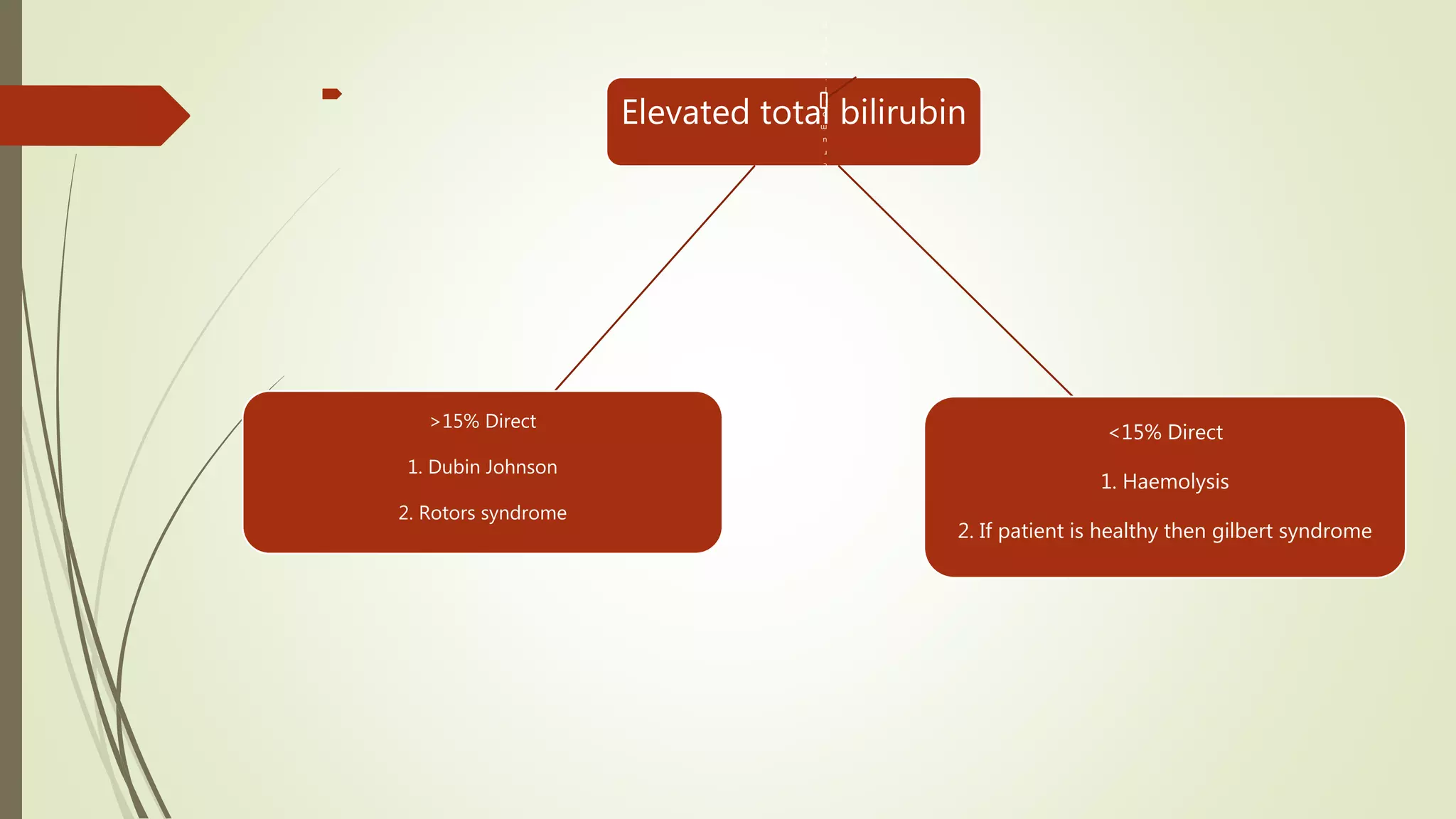
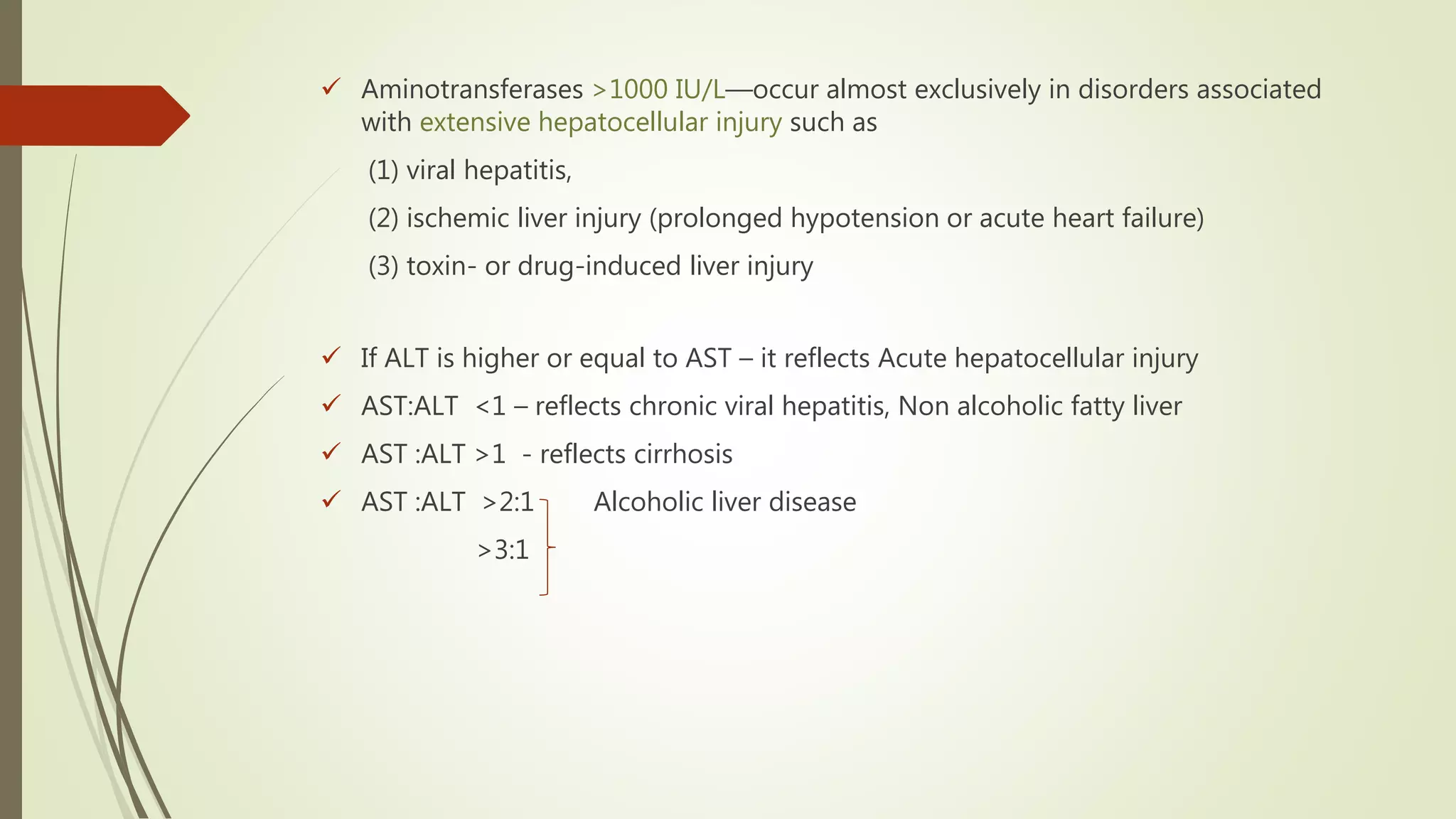
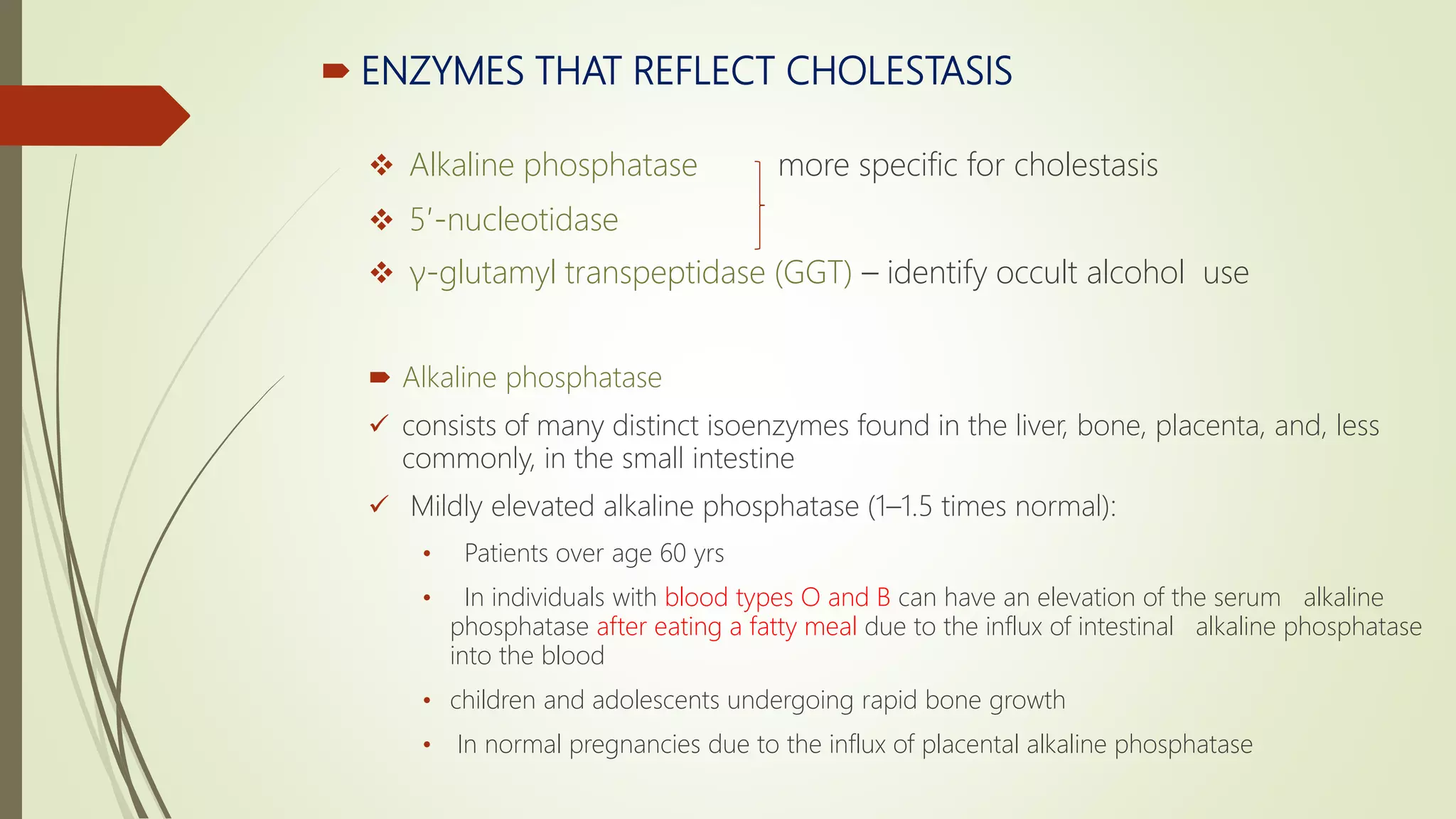
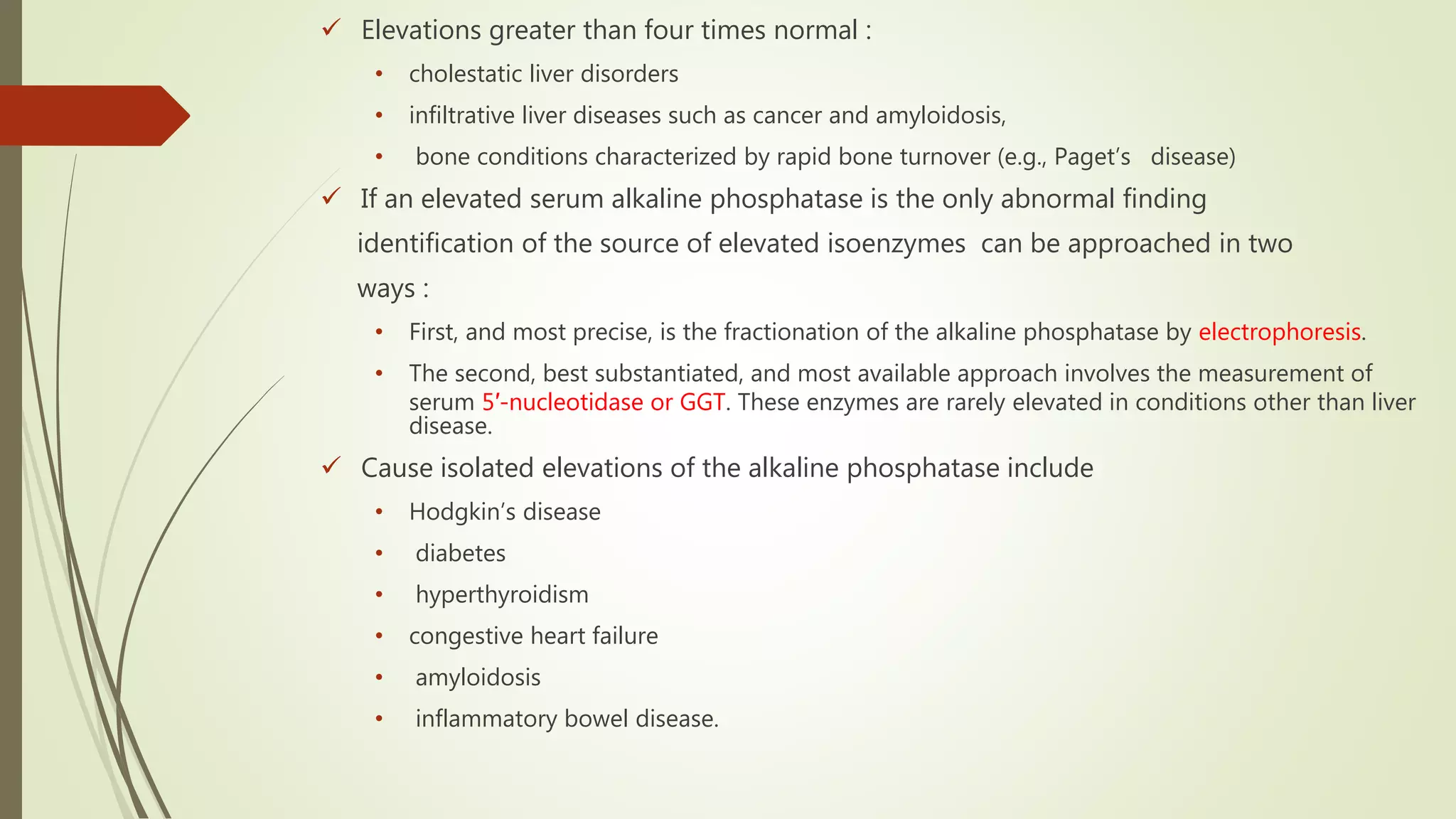
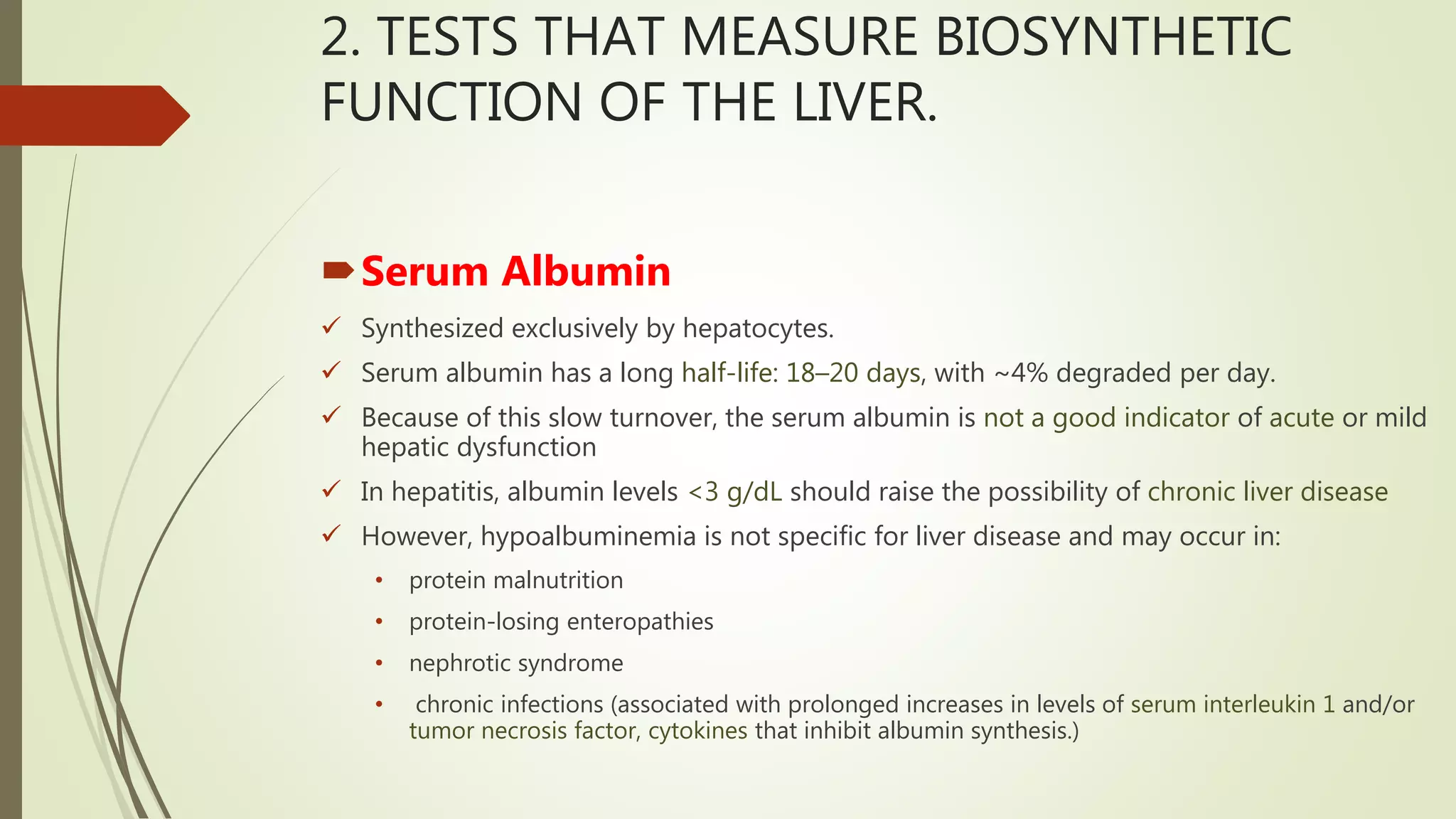
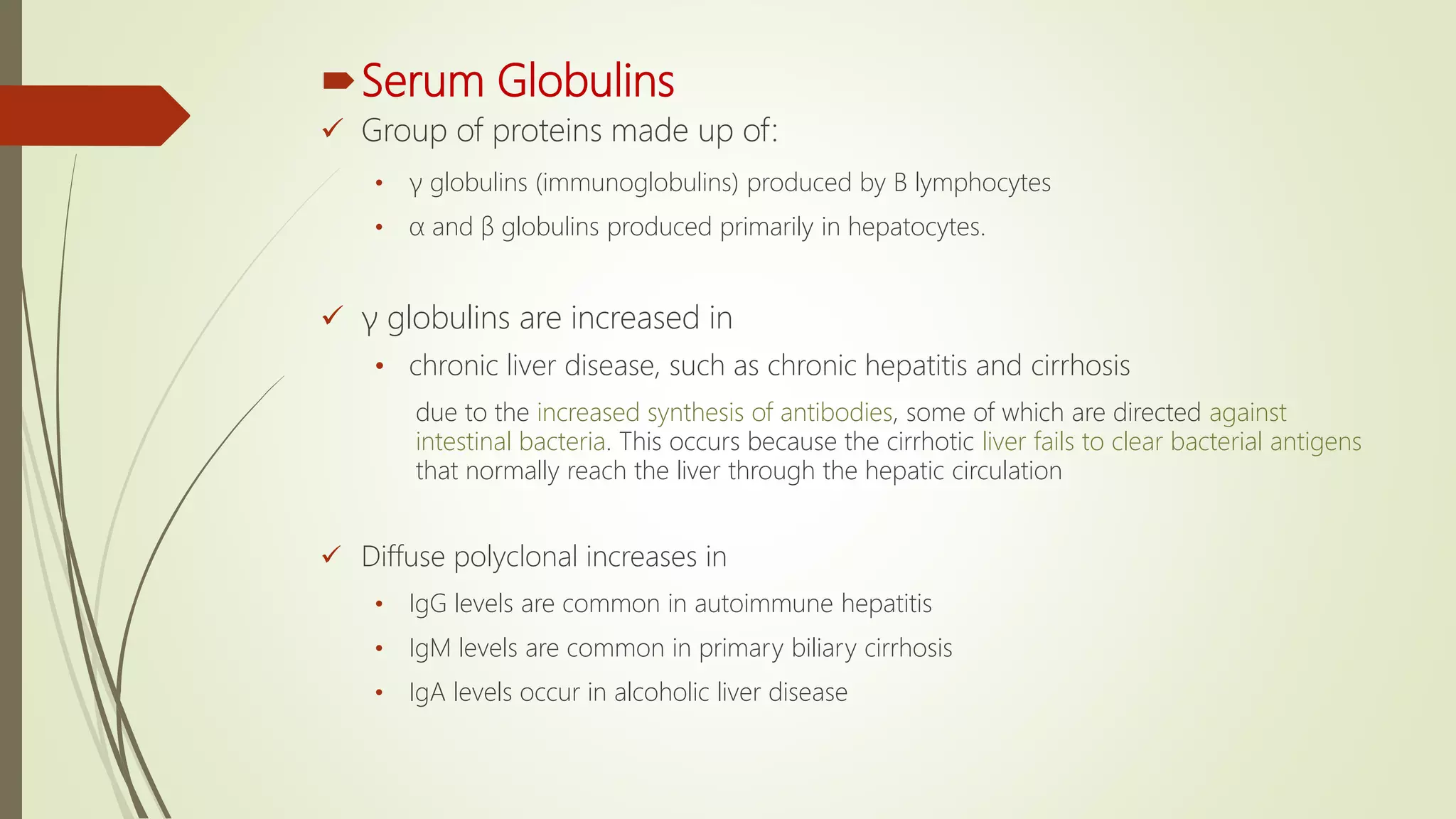
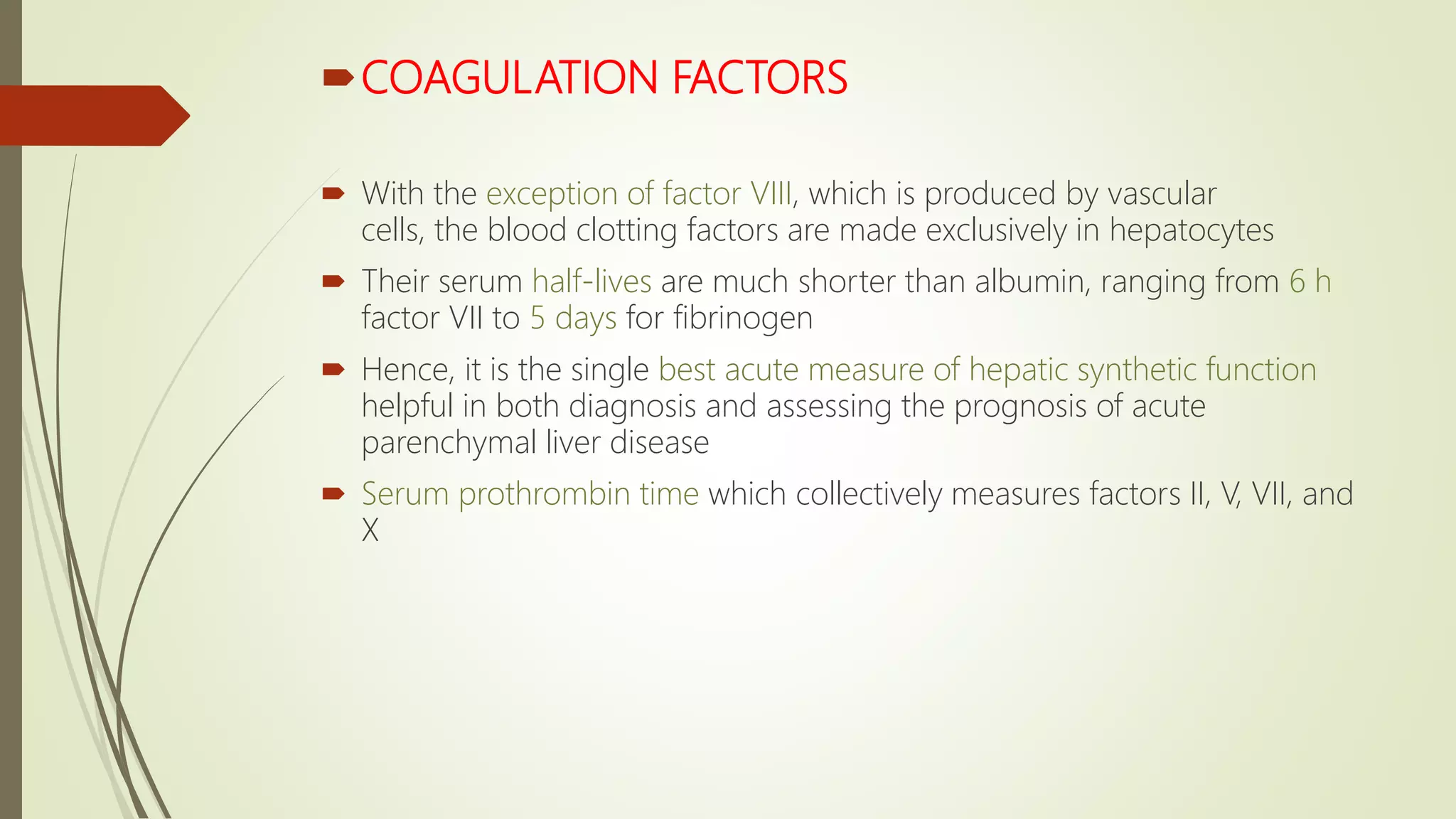
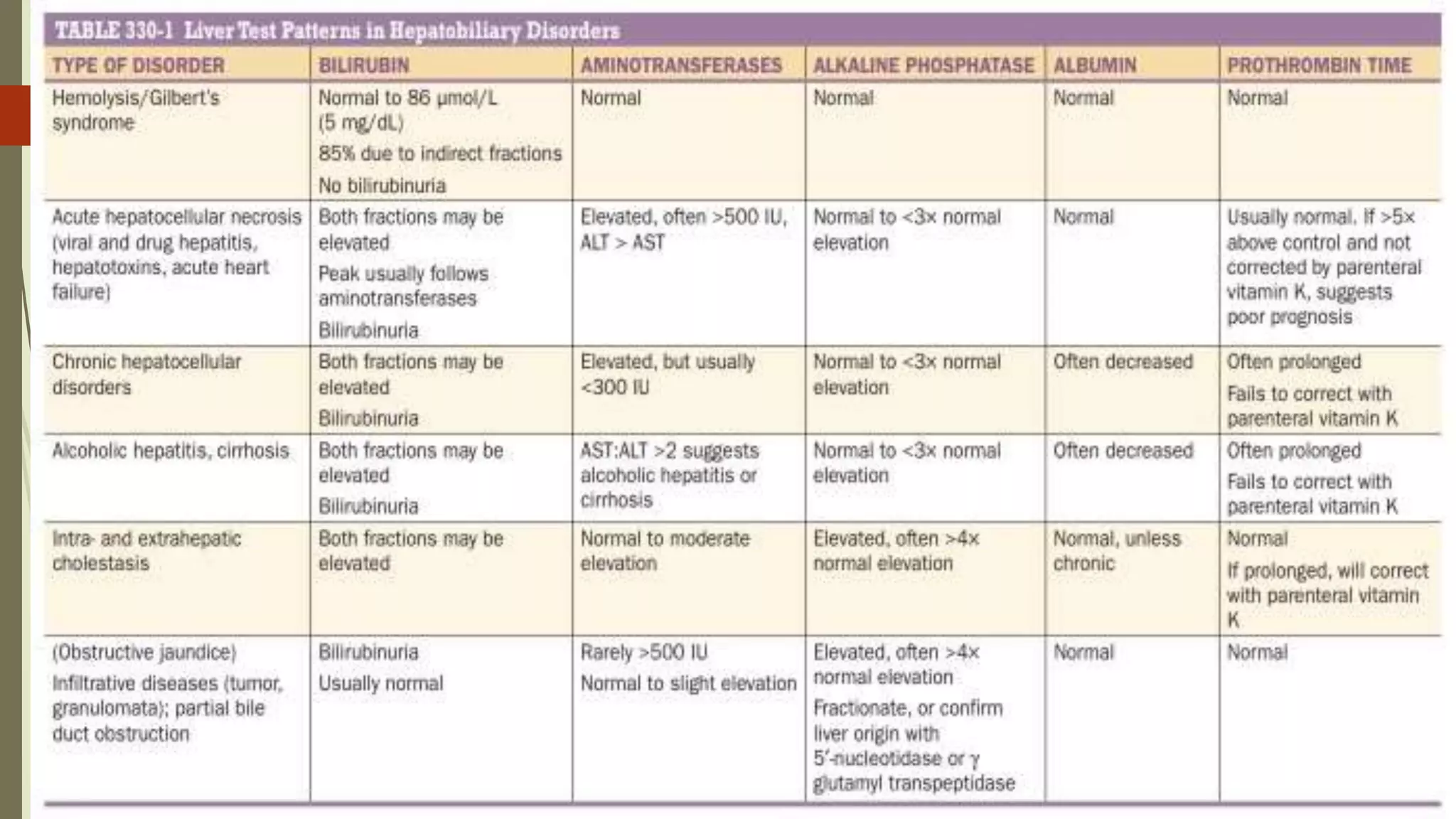
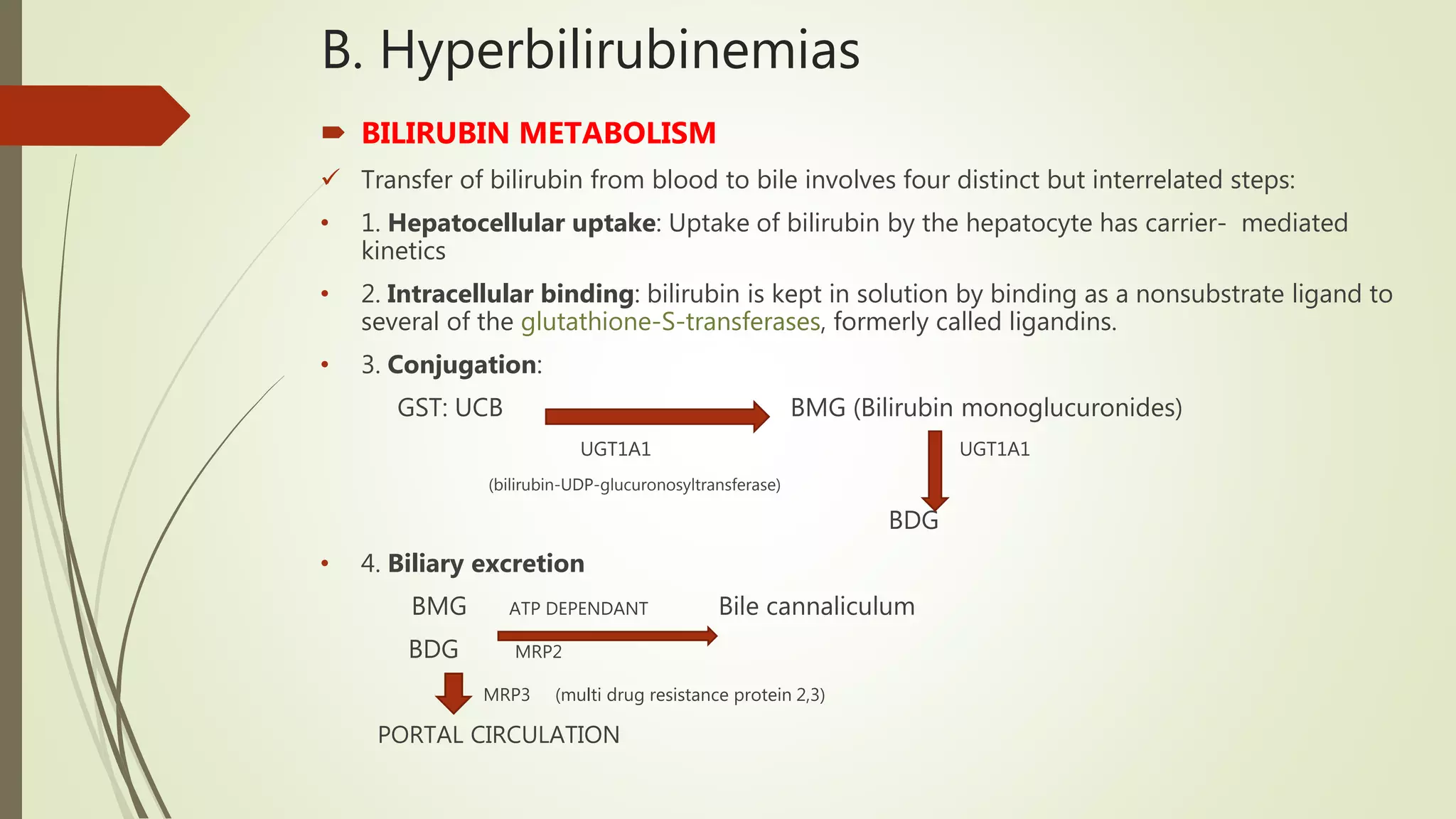
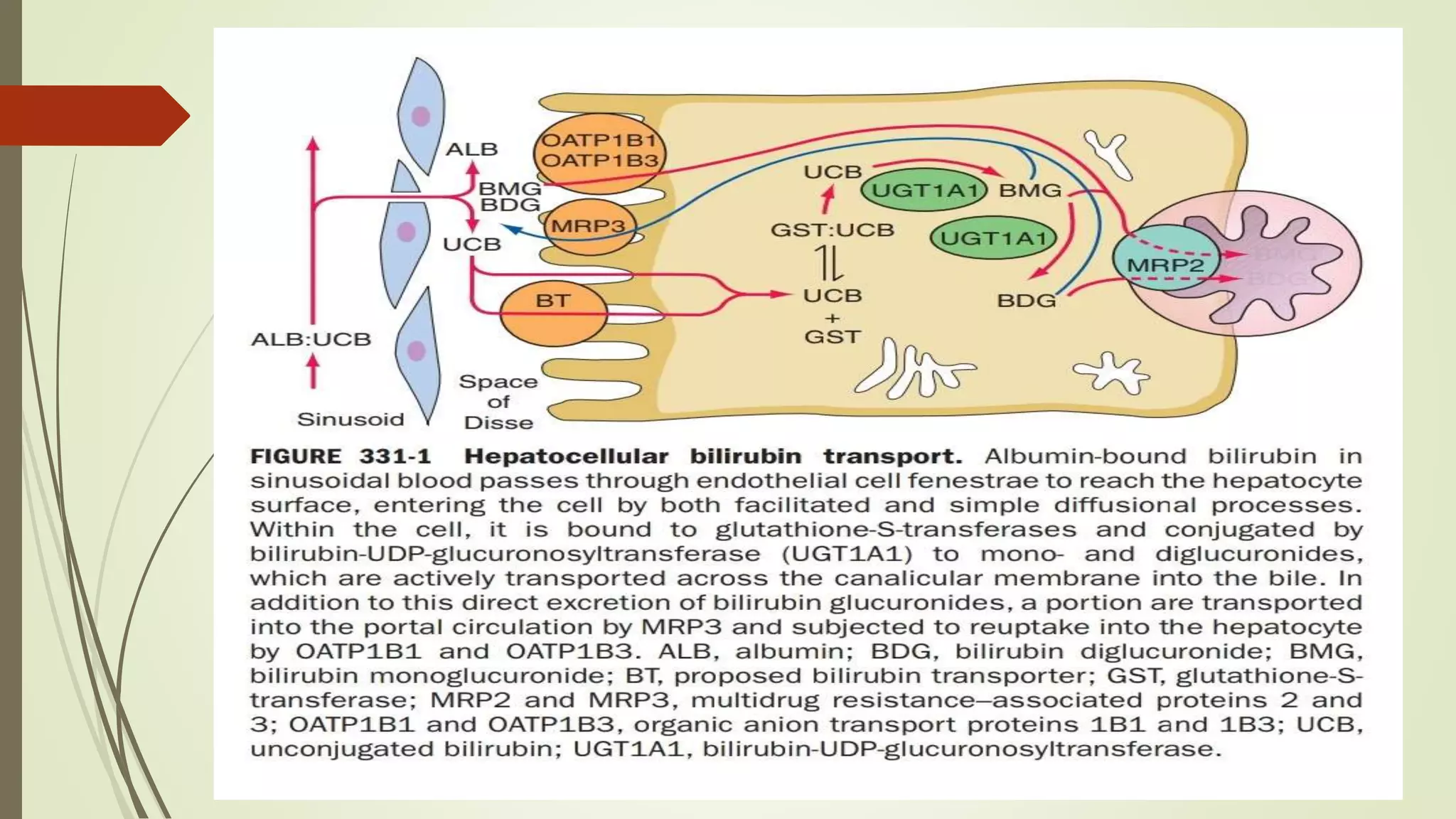
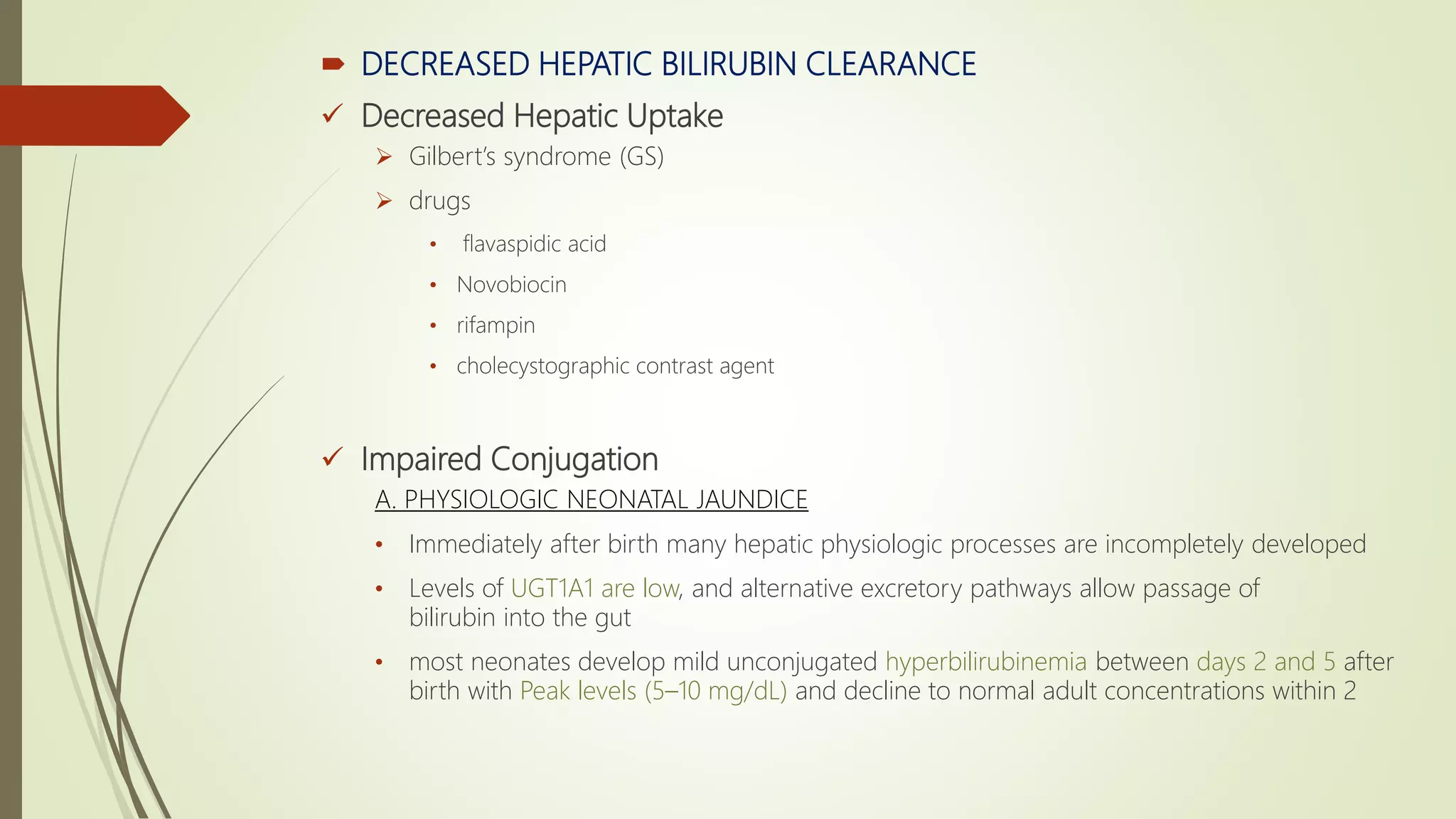
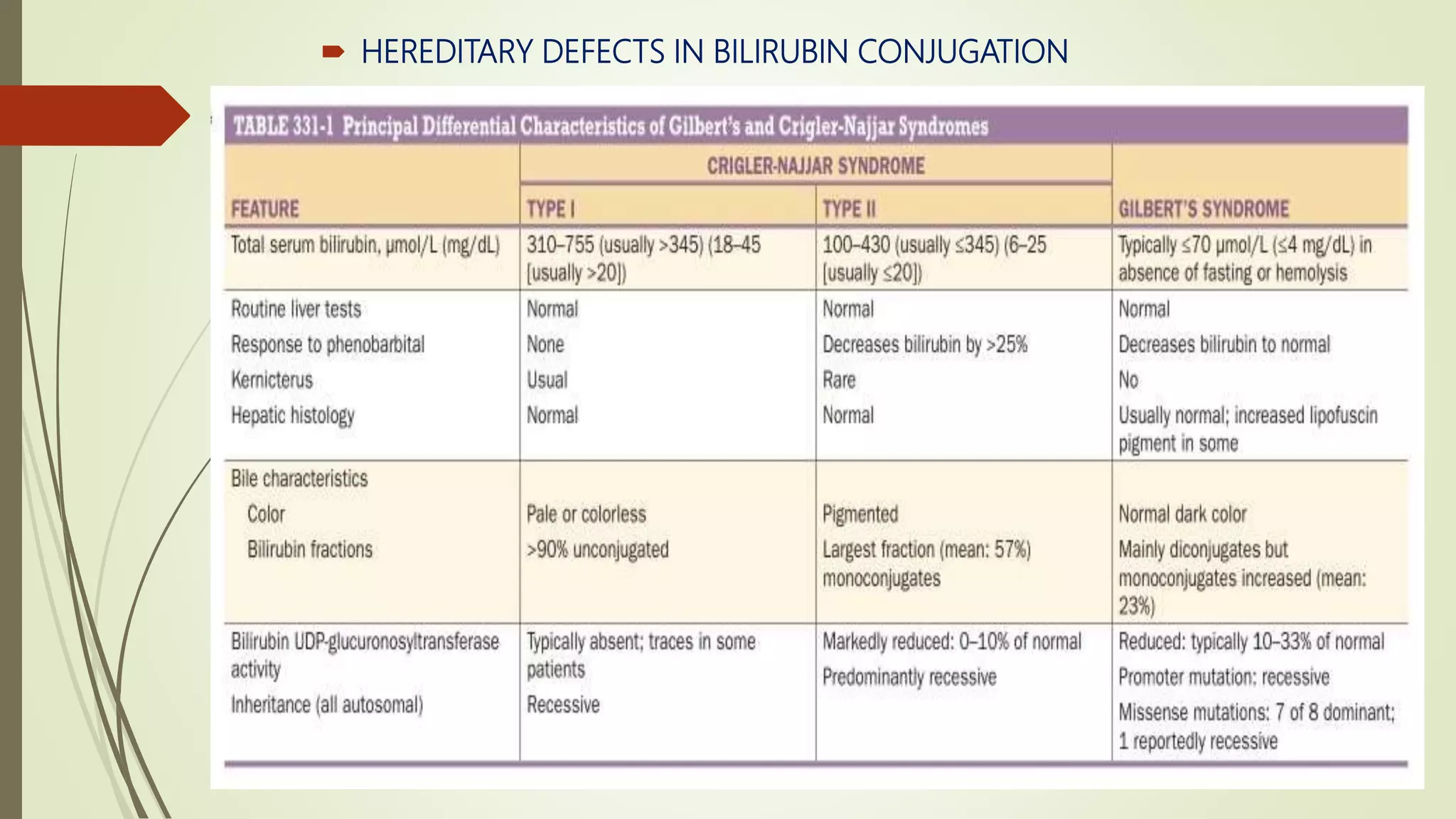
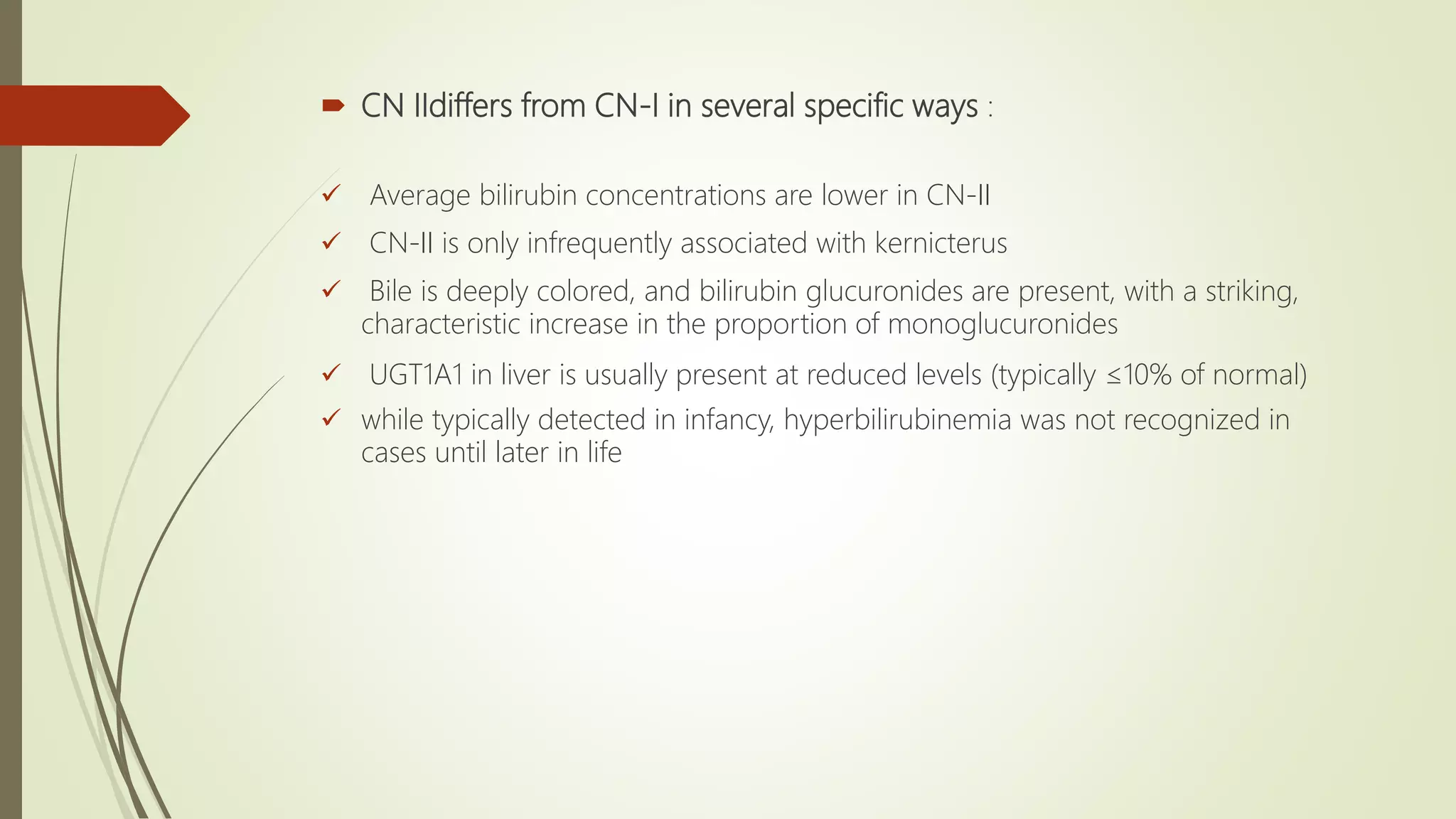
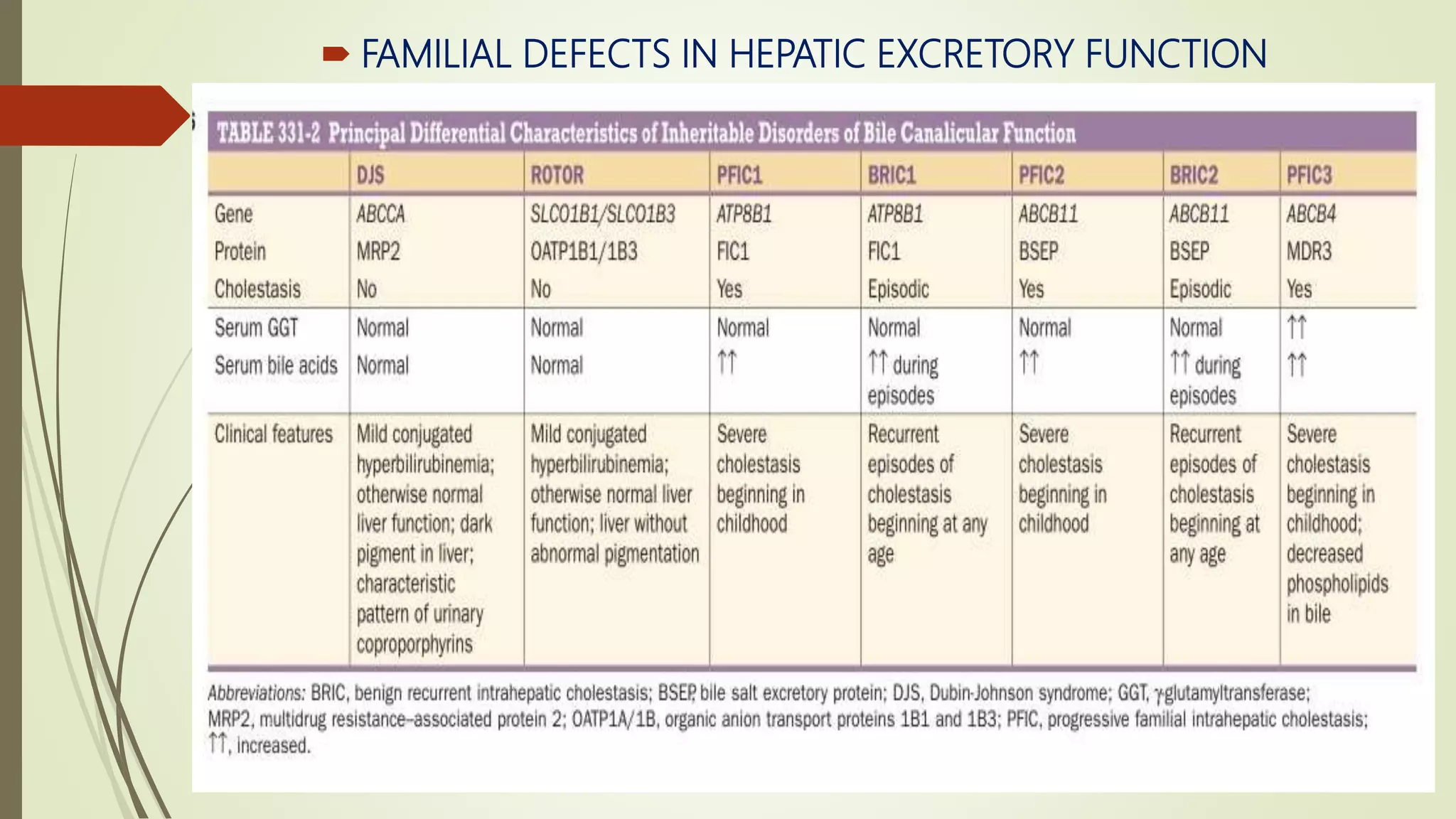
This document discusses the evaluation of liver function and hyperbilirubinemias. It covers liver function tests including serum bilirubin, urine bilirubin, blood ammonia, and serum enzymes. It discusses tests that measure the liver's biosynthetic function like serum albumin and coagulation factors. It also covers bilirubin metabolism and disorders that can lead to unconjugated hyperbilirubinemia through increased bilirubin production, decreased hepatic uptake, or impaired conjugation. Specific conditions mentioned include Gilbert's syndrome, neonatal jaundice, hepatitis, and inherited conjugation defects.