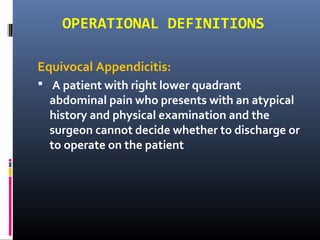
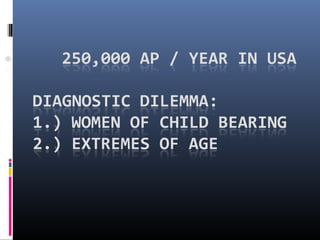
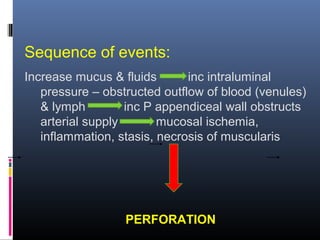
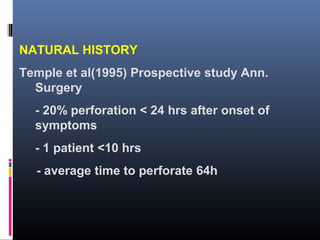
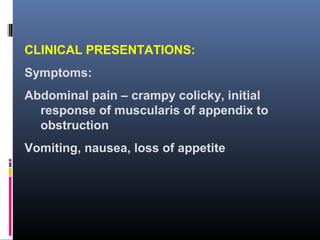
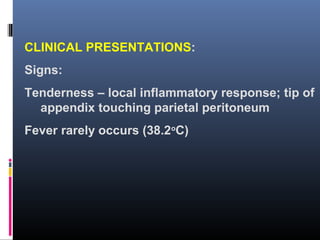
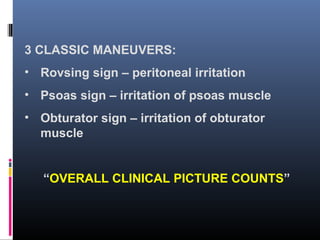
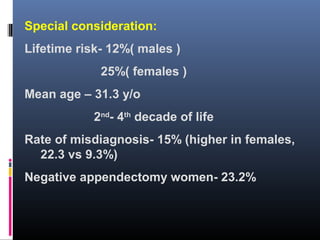
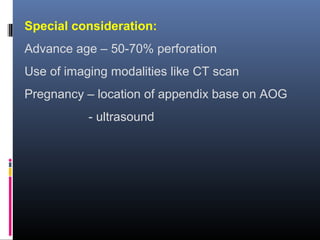
Acute appendicitis is the most common surgical emergency of the abdomen. It occurs when the appendix becomes blocked and inflamed. Without treatment, the appendix can perforate. While mortality from perforated appendicitis was near certain in the past, improved medical care has reduced mortality to 1% or less today. However, rates of unnecessary appendectomies and perforation remain high. Acute appendicitis is diagnosed based on symptoms, signs on examination, and sometimes imaging tests. The standard treatment is appendectomy to remove the inflamed appendix.