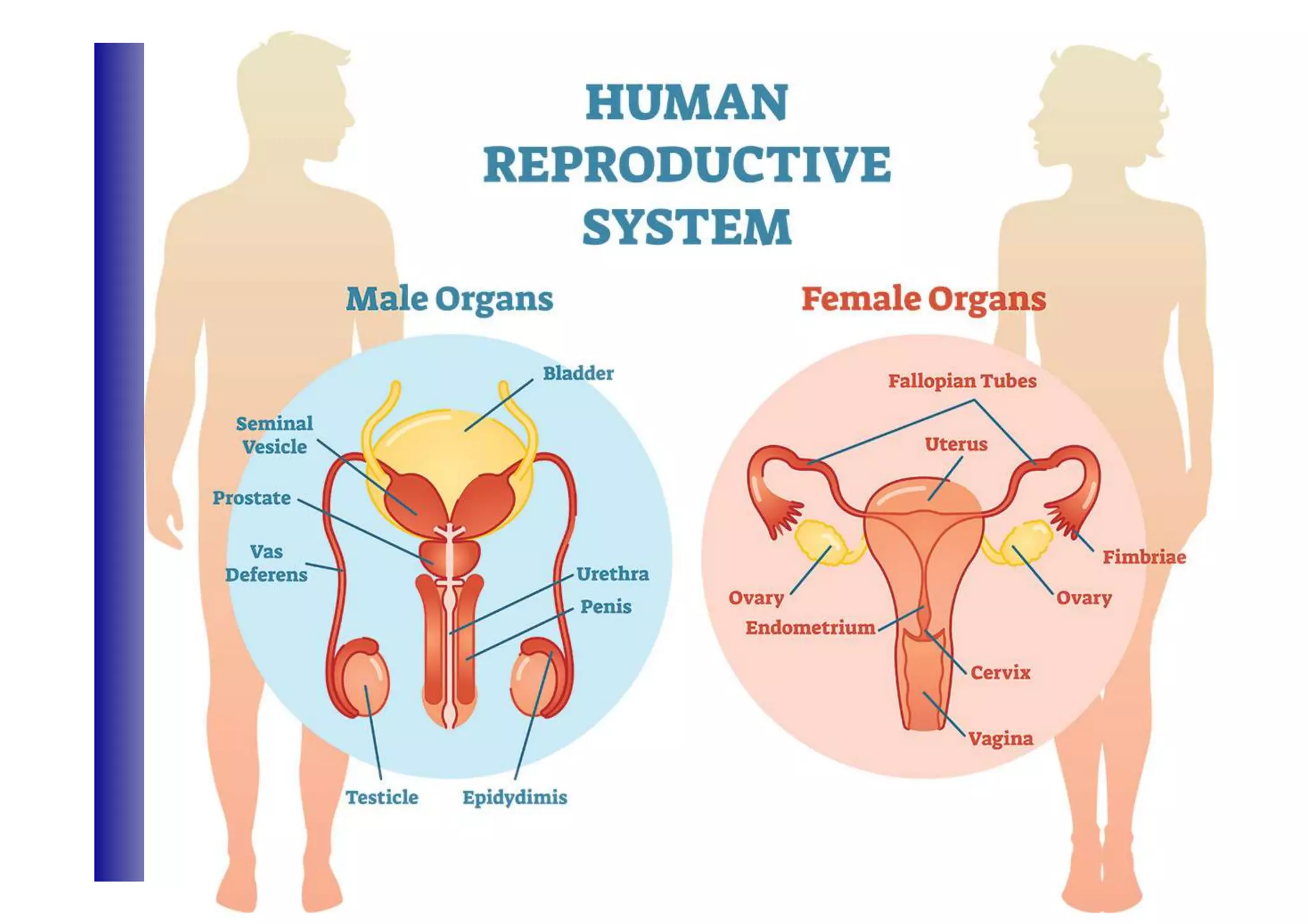
This document provides an overview of the male and female reproductive systems, including:
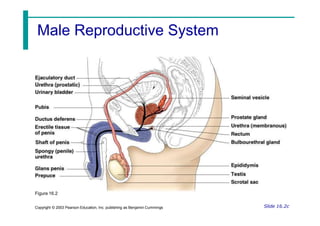
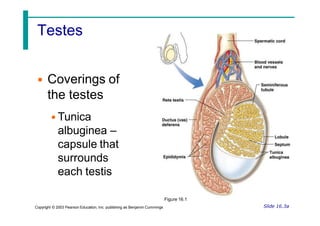
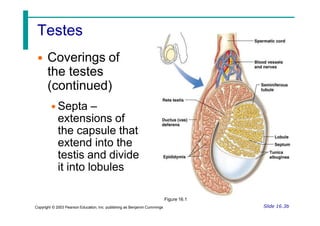
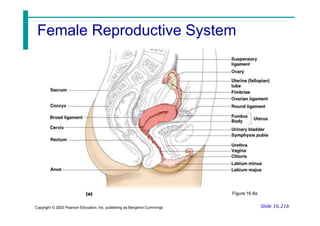
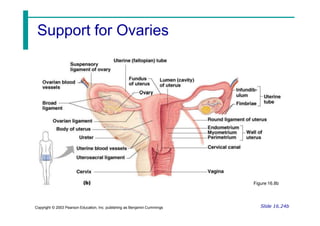
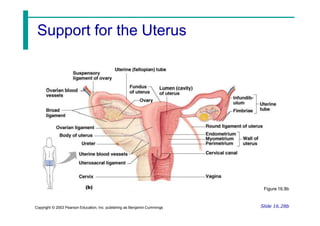
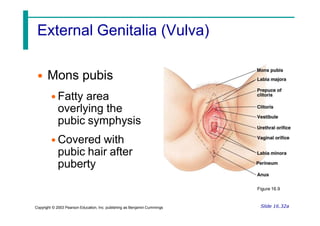
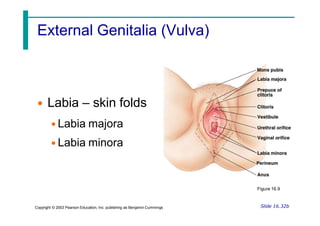
1) It describes the main organs involved in both systems such as the testes, ovaries, duct systems, and external genitalia.
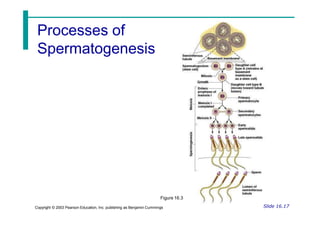
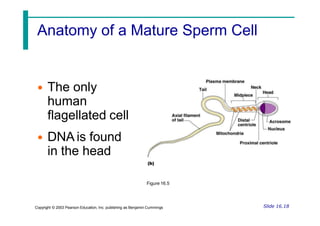
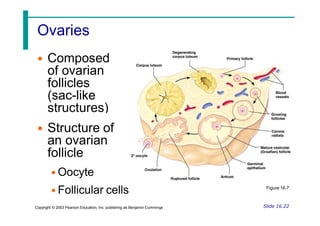
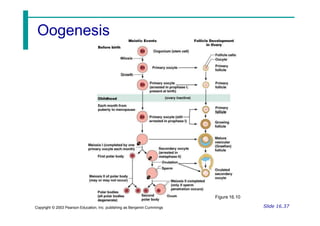
2) It explains the processes of sperm and egg production, including spermatogenesis and oogenesis.
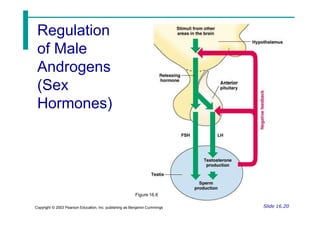
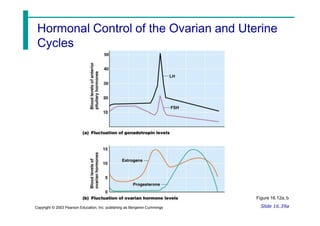
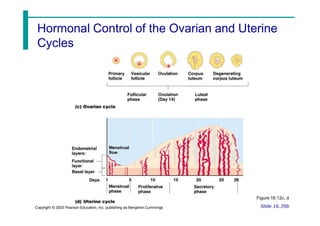
3) It outlines the hormonal control of the ovarian and uterine cycles in females and testosterone production in males.