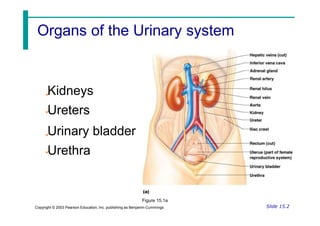
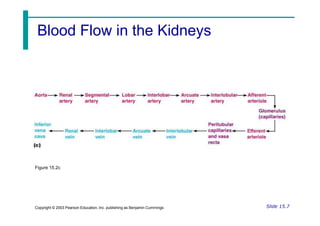
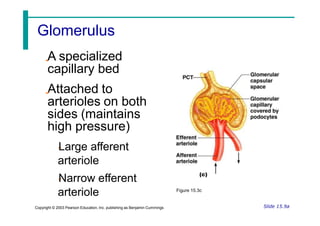
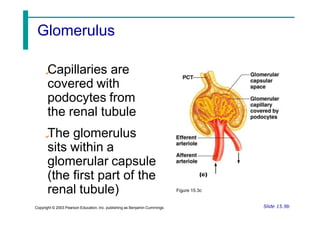
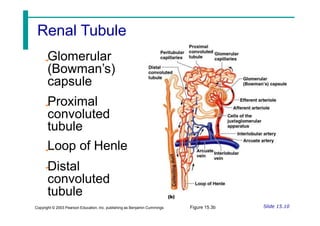
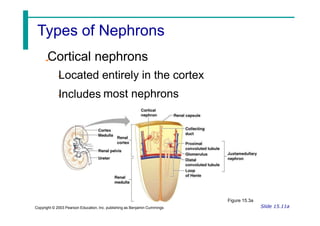
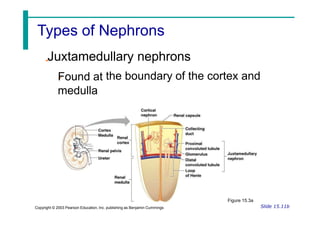
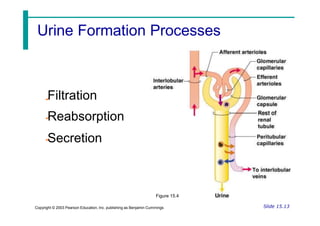
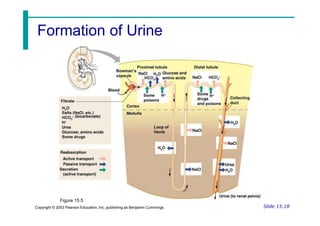
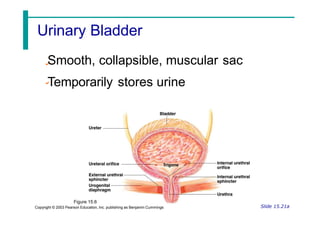
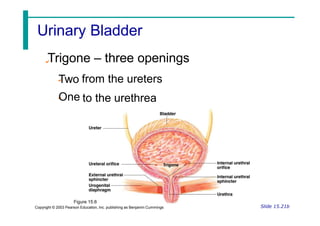
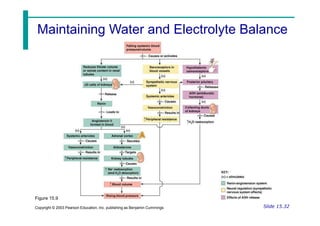
The urinary system functions to eliminate waste from the body in the form of urine, and to regulate water balance, electrolyte and acid-base levels. The main organs are the kidneys, ureters, urinary bladder and urethra. The kidneys contain millions of nephrons which are the functional filtering units, composed of a glomerulus and renal tubule. Urine is formed through the processes of filtration, reabsorption and secretion as fluid passes through the nephron. The urinary system also helps regulate water balance and maintain the body's acid-base and electrolyte levels through hormone control and kidney functions.