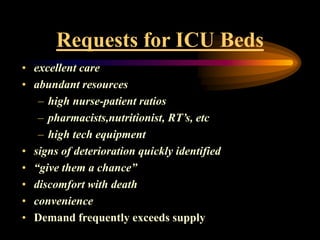
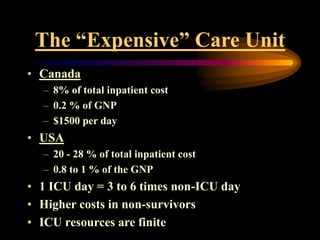
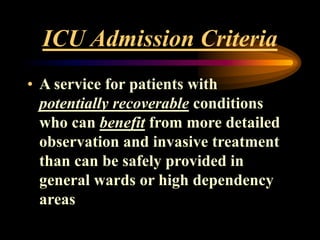
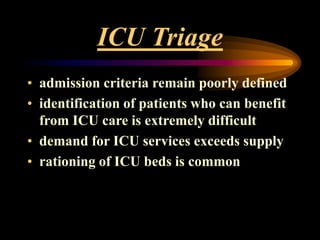
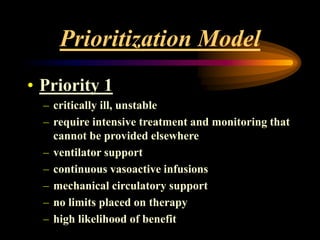
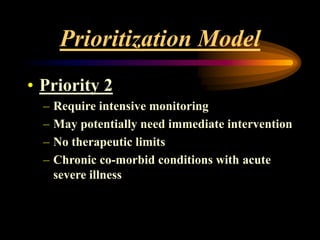
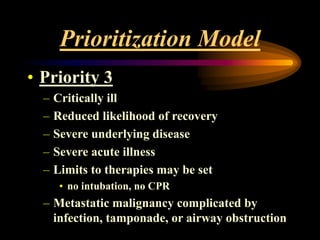
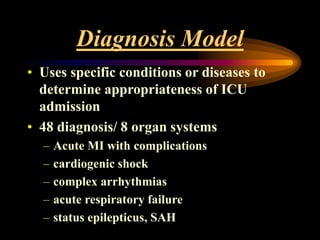
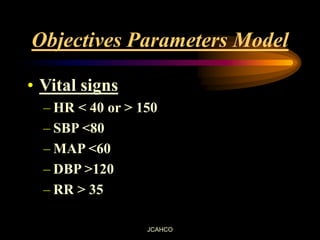
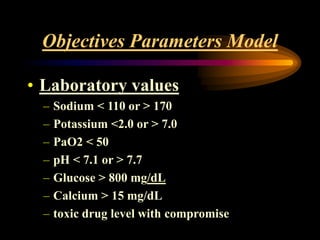
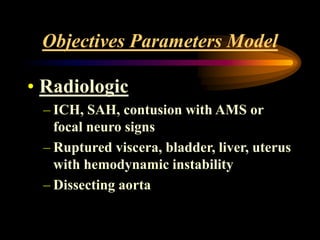
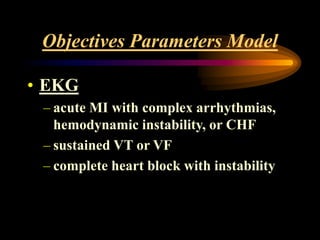
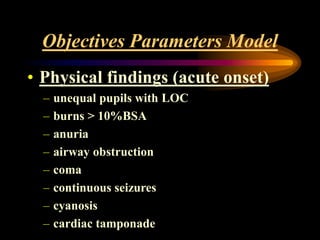
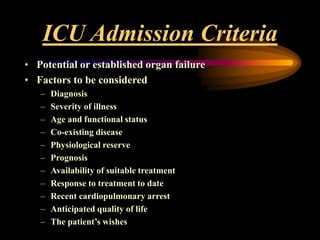
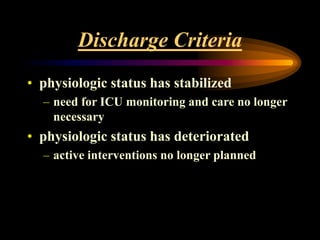
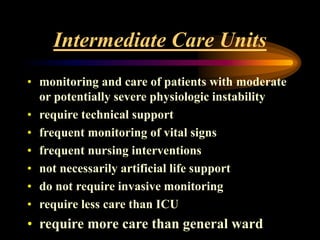
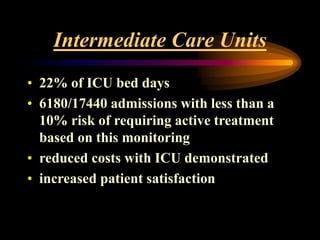
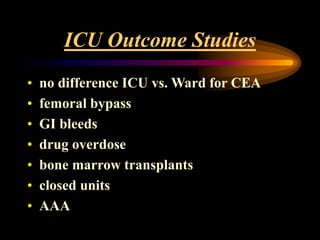
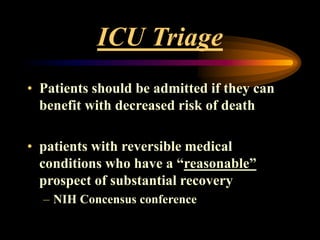
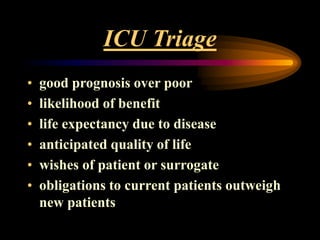
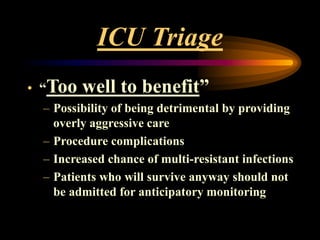
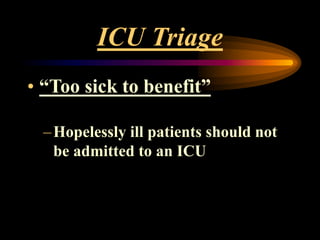
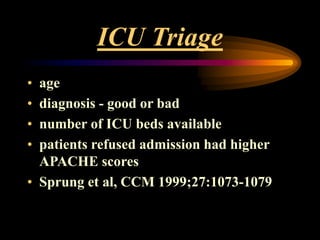
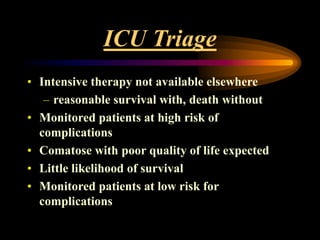
The document discusses criteria for admission and triage to the intensive care unit (ICU). It notes that demand often exceeds supply of ICU beds. It presents several models for prioritizing patients, including based on diagnosis and severity of illness. Factors considered for admission include prognosis, likelihood of benefit, and patient wishes. The document also discusses criteria for discharge and intermediate care units as alternatives to the ICU.