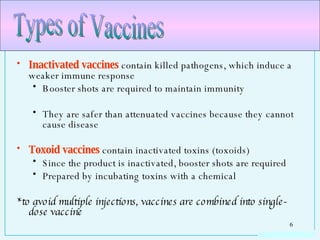
The document discusses different types of immunity and serological reactions. It describes the two main types of immunity - innate immunity and acquired immunity. Acquired immunity includes active immunity, which can be naturally or artificially acquired through vaccination, and passive immunity, which can also be naturally or artificially acquired through antibodies from another source. The document then goes into detail about different types of vaccines and serological reactions used to detect pathogens.



















![In the lab, antibodies recognizing one epitope (monoclonal antibodies [mAb]) are produced using myelomas Myeloma cells are fused to and activated B cell to form a hybridoma A hybridoma producing the desired mAb can be cloned MAbs can be used in: disease prevention immunomodulation (controlling overactive inflammatory responses)](https://image.slidesharecdn.com/chap20immunology-serology-1217836007473113-9/85/Chap20-Immunology-Serology-26-320.jpg)
