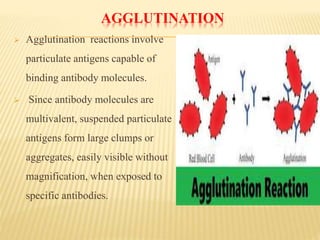
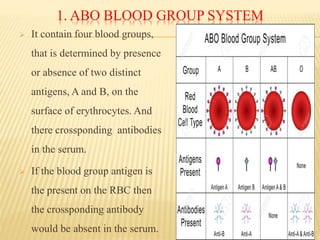
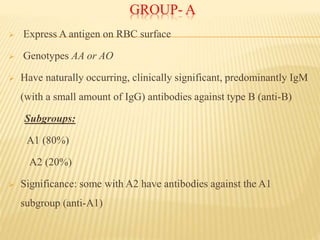
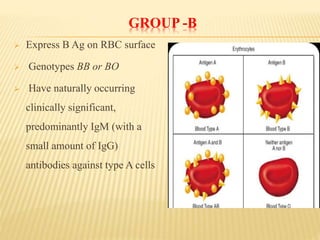
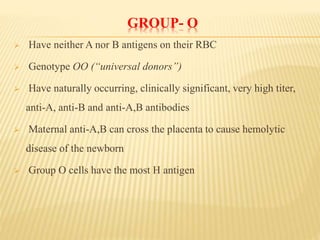
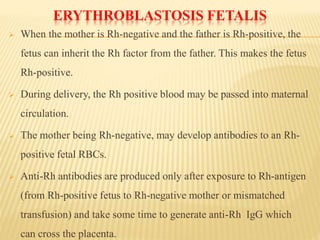
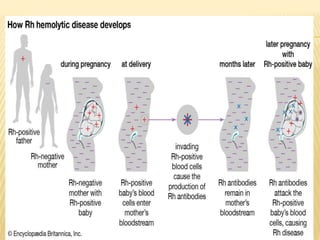
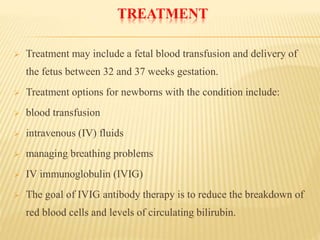
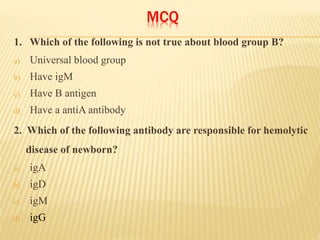
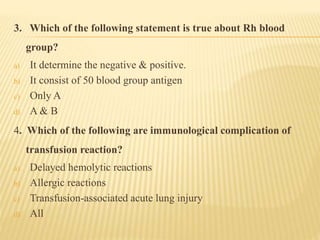
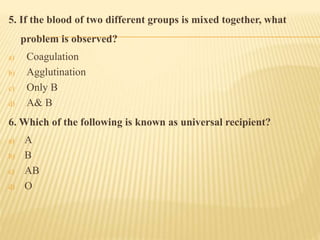
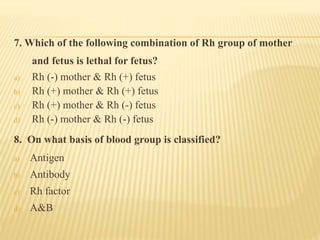
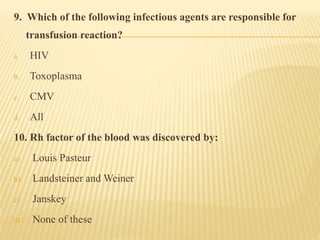
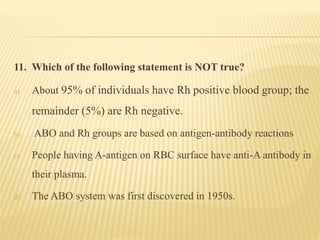
Immunohematology is the study of blood groups and blood transfusion. Karl Landsteiner discovered the ABO blood group system in humans. The major blood group systems are ABO and Rh. The ABO system consists of four blood groups - A, B, AB and O based on the presence or absence of A and B antigens on red blood cells. Rh system consists of Rh+ and Rh- blood based on presence or absence of D antigen. Erythroblastosis fetalis is a blood group incompatibility reaction between Rh- mother and Rh+ fetus. It can be prevented by Rh immunoglobulin administration. Blood transfusion requires matching of blood groups to avoid immune reactions.