This document provides an overview of immunology and the immune system. It discusses key topics such as:
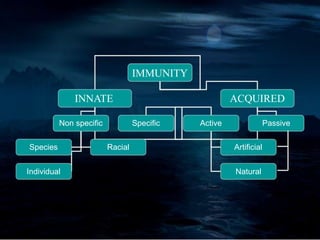
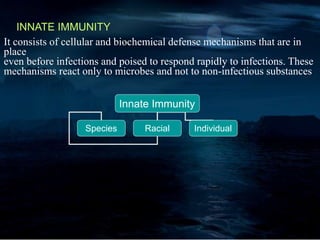
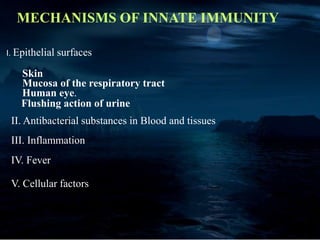
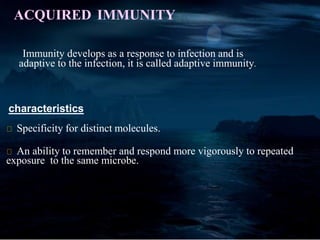
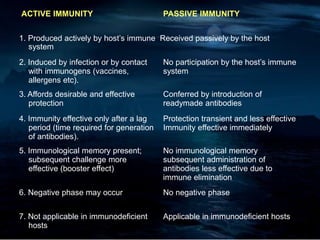
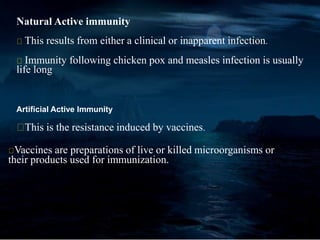
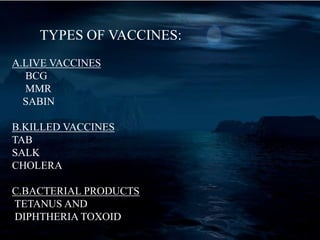
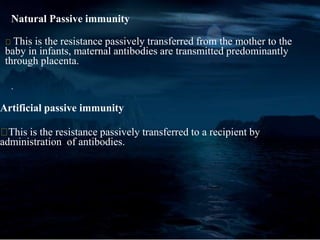
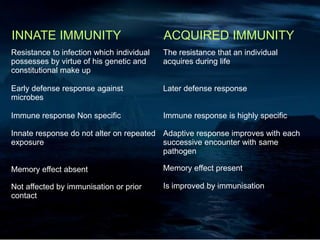
- Innate and acquired immunity, including active and passive immunity. Innate immunity provides non-specific protection while acquired immunity is adaptive and provides long-lasting protection.
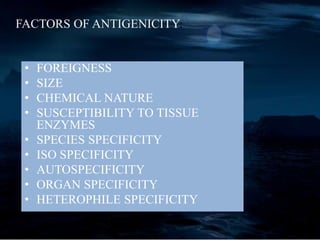
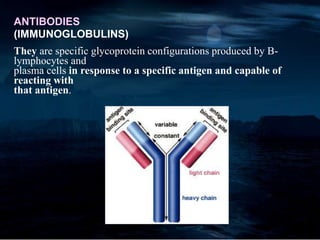
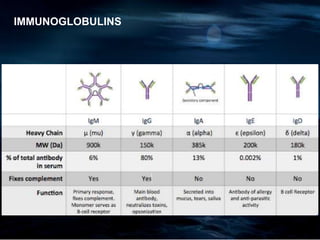
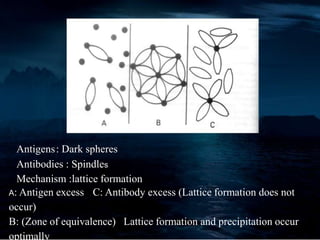
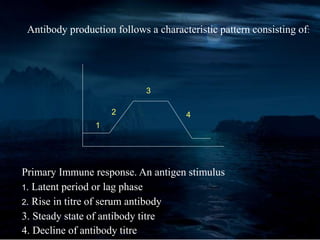
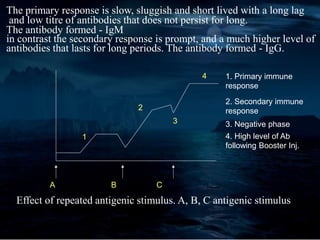
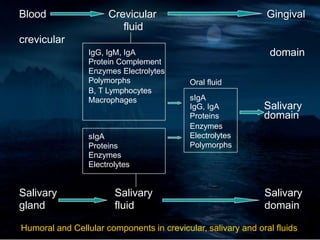
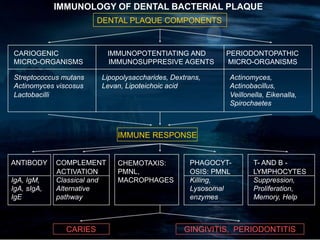
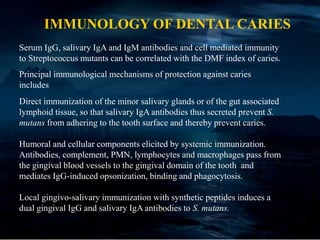
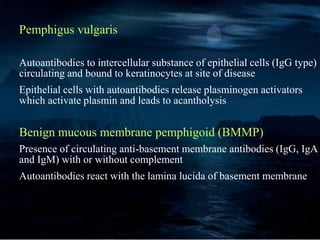
- Antigens and antibodies. Antigens stimulate antibody production while antibodies provide specific responses to antigens. Antigen-antibody reactions include precipitation and agglutination.
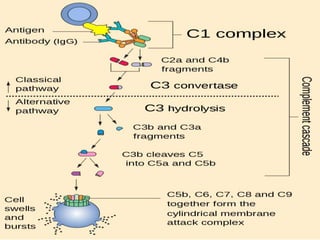
- The complement system, which enhances antigen-antibody reactions and mediates immune responses.
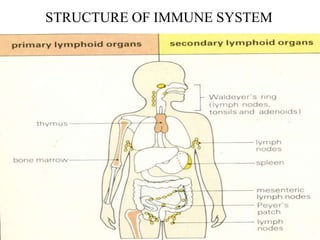
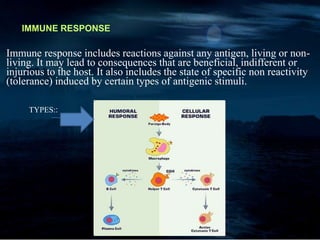
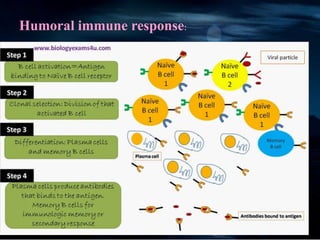
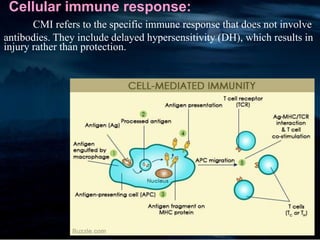
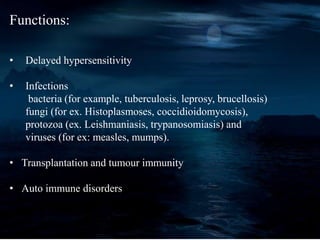
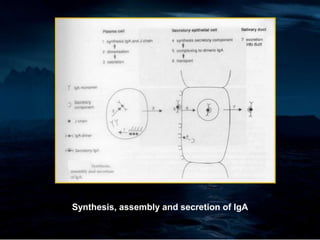
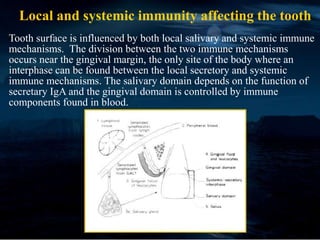
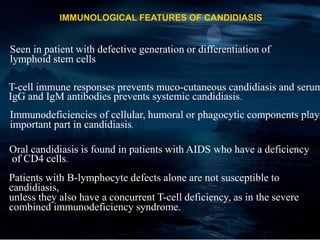
- Structure and function of the immune system, including humoral responses involving B cells and antibodies, and cellular responses involving T cells.
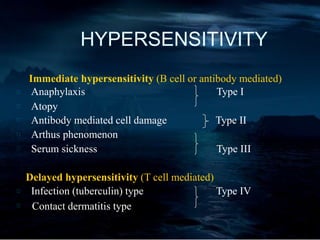
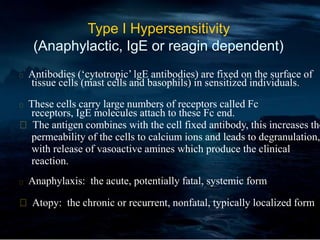
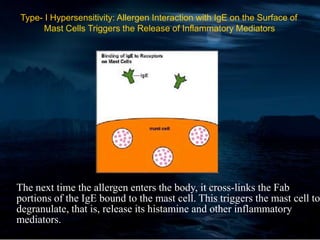
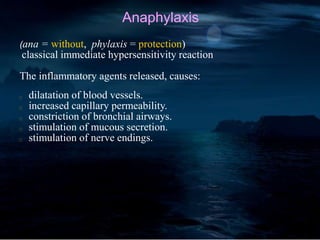
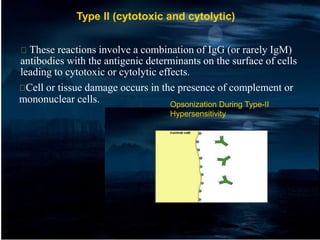
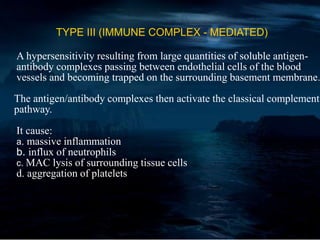
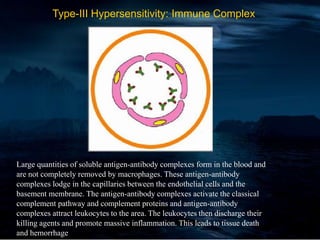
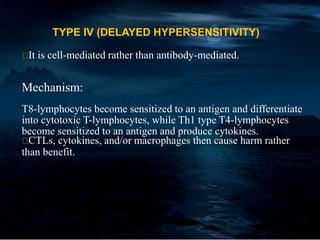
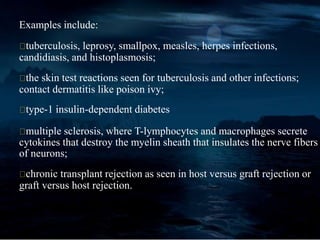
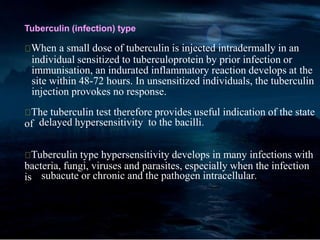
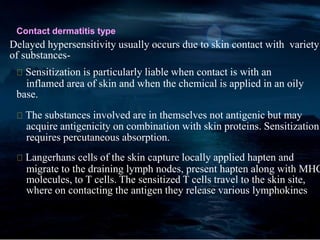
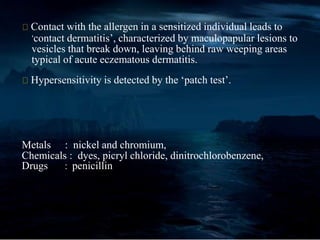
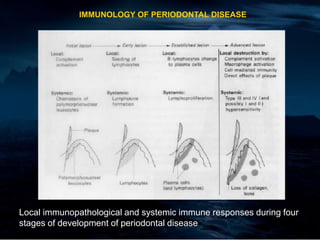
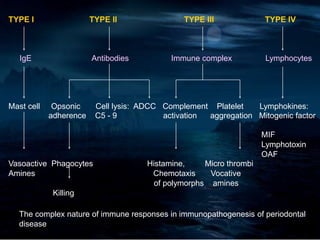
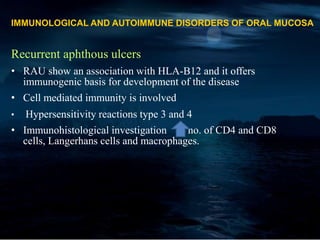
- Hypersensitivity reactions