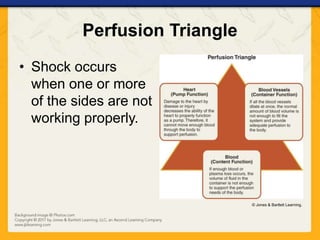
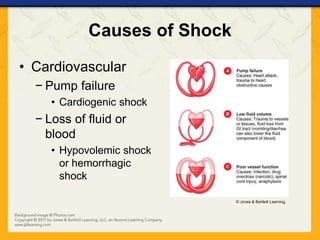
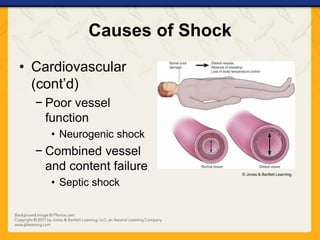
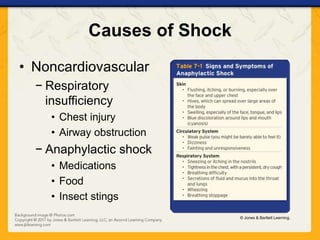
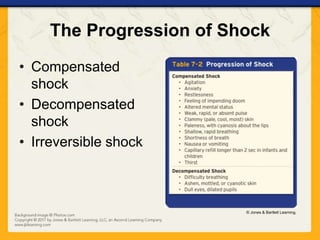
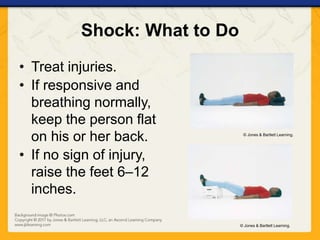
Shock is caused by inadequate blood flow and oxygen delivery to tissues. The causes include cardiovascular issues like heart failure or blood loss, as well as non-cardiovascular issues like respiratory problems, allergic reactions, or psychological stress. The signs of shock include altered mental status, pale skin, rapid breathing and heartbeat, and nausea. Treatment focuses on treating injuries, keeping the person lying down and warm, and calling for emergency help.