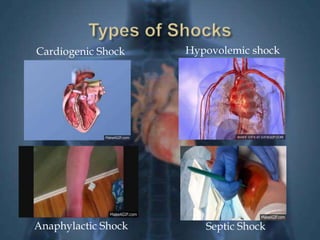
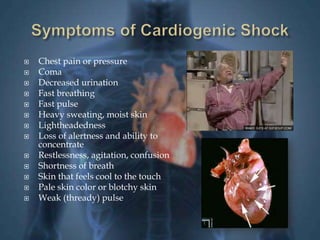
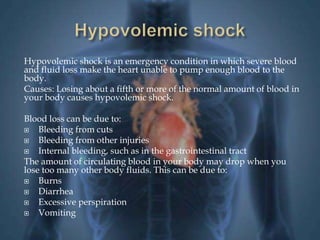
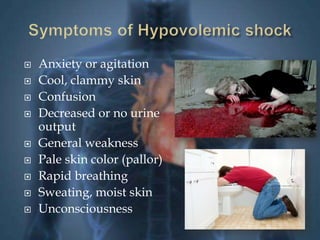
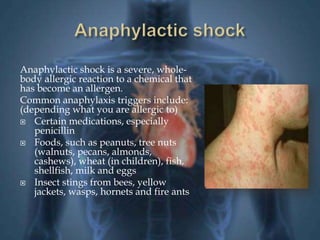
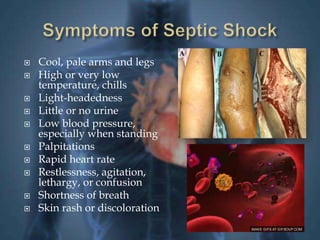
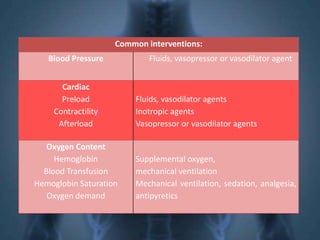
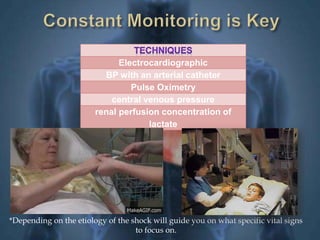
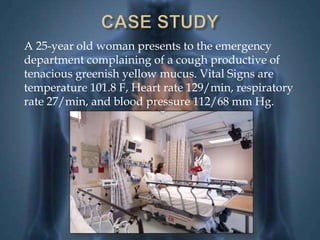
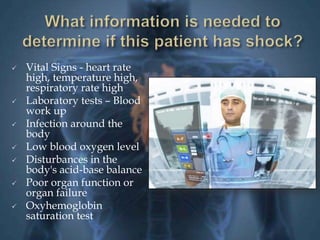
Shock is a critical medical condition characterized by insufficient blood flow to the body's organs, resulting in inadequate oxygen and nutrient delivery. It can be categorized into four types: cardiogenic, hypovolemic, anaphylactic, and septic shock, each with distinct causes and symptoms. Management focuses on restoring perfusion, stabilizing blood pressure through various medical interventions, and treating the underlying cause of shock.