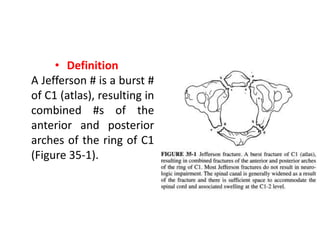
1. A Jefferson fracture is a burst fracture of the C1 vertebra (atlas) that results in a break of both the anterior and posterior arches of the ring.
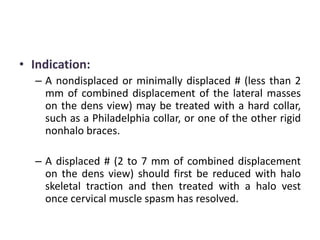
2. It is caused by axial compression, often from a fall on the head, and may not be evident on lateral x-rays but displacement of the lateral masses on open-mouth views suggests a Jefferson fracture.
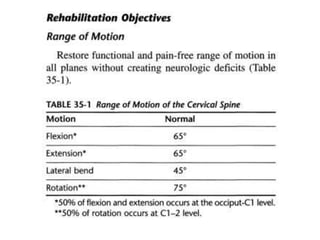
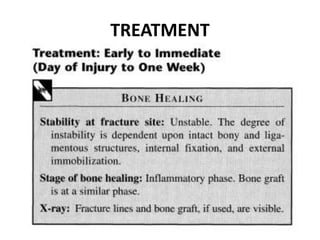
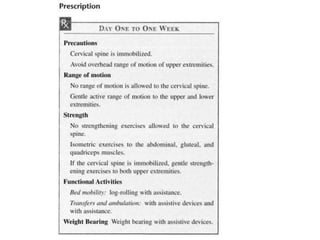
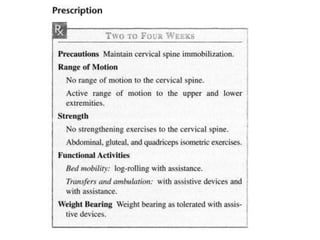
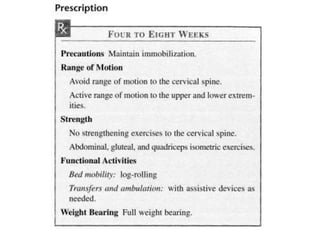
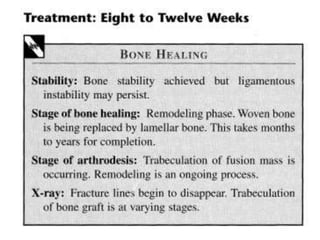
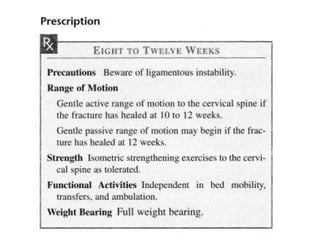
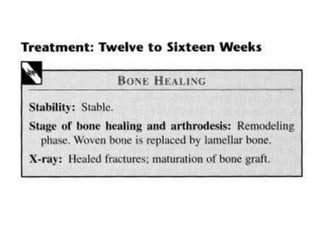
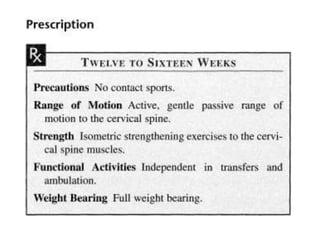
3. Treatment involves halo traction followed by a halo vest or posterior fusion to stabilize and fuse the fracture, with the goals of maintaining spinal alignment and preventing neurological injury.