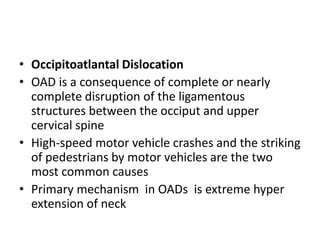
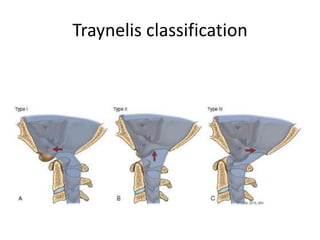
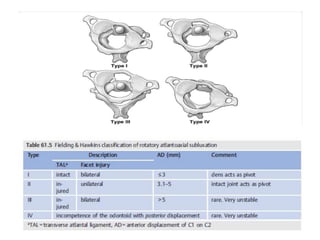
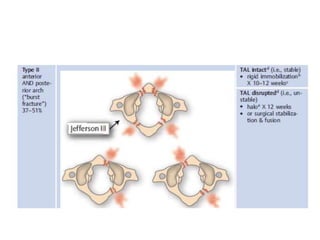
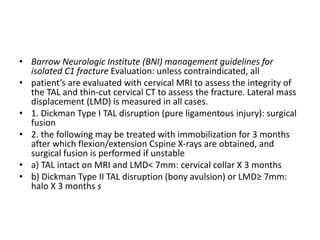
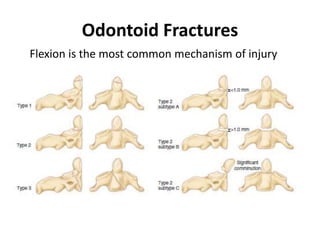
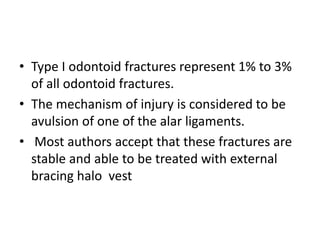
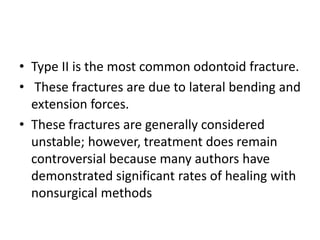
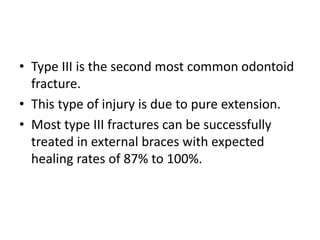
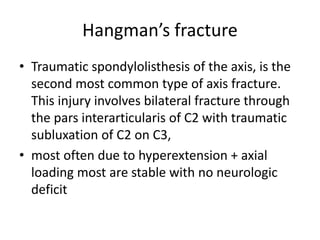
1. The document discusses various types of cervical spine injuries including occipitoatlantal dislocations, occipital condyle fractures, atlantoaxial subluxations, transverse ligament injuries, C1 and C2 fractures.
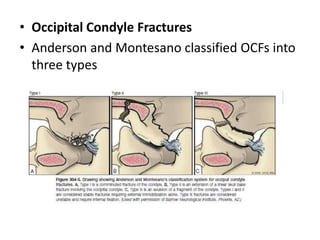
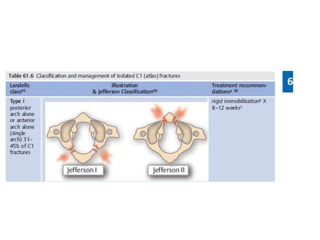
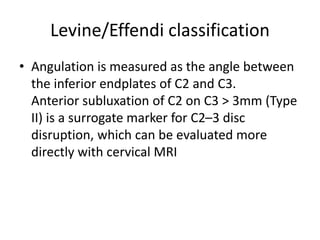
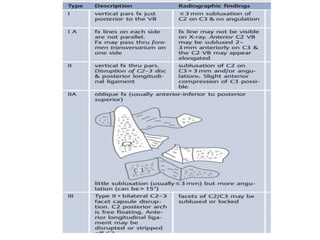
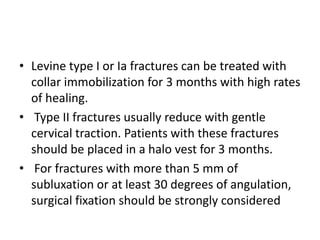
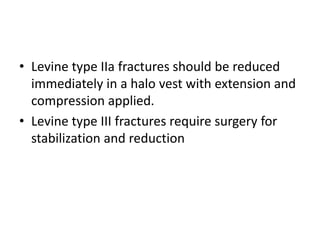
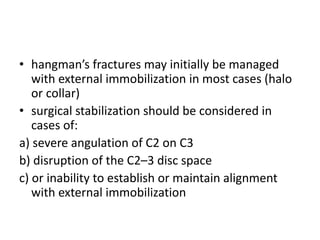
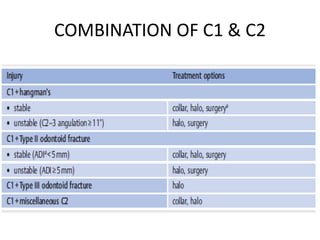
2. It provides details on mechanisms of injury, classification systems, diagnostic criteria, non-surgical and surgical treatment options for each type of injury.
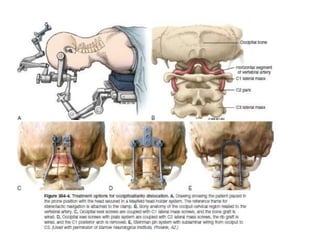
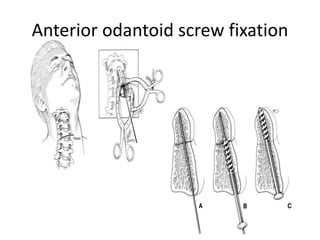
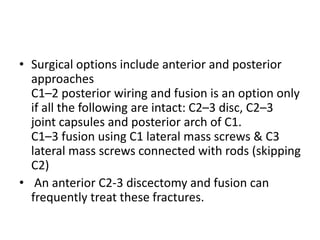
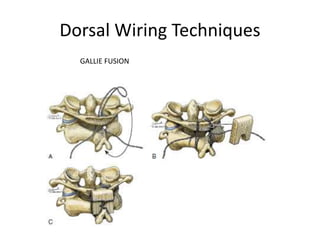
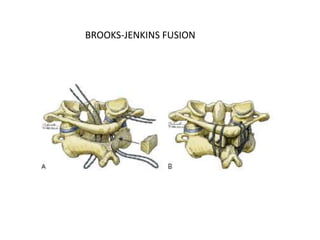
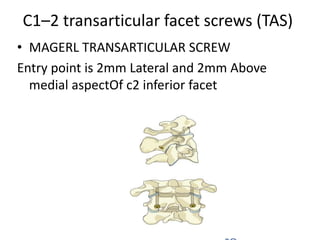
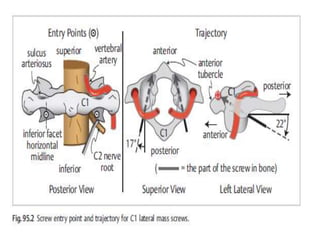
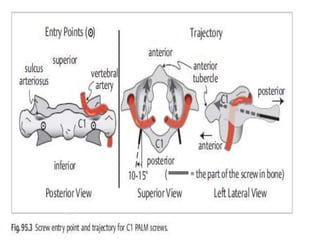
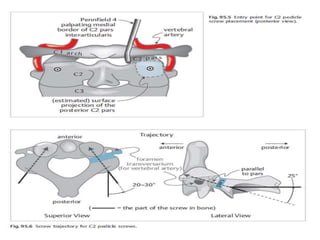
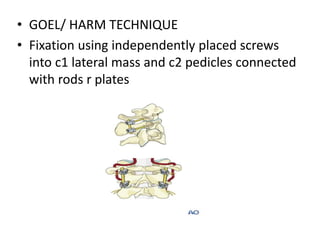
3. Surgical treatment may involve various fusion techniques from occiput to C2 or C3 including wiring, plating, and screw fixation depending on the instability and bones involved in the injury.