- A bursa is a fluid-filled sac that acts as a cushion between bones, muscles, and ligaments near joints. Injury to a bursa can cause pain, limited motion, and decreased mobility.
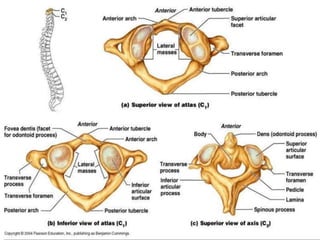
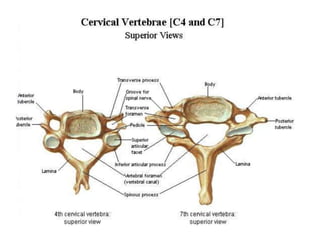
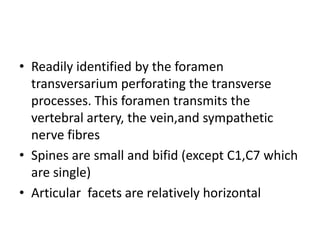
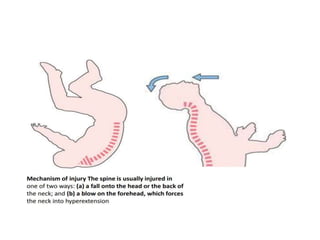
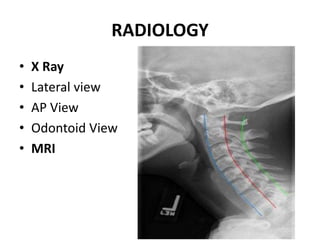
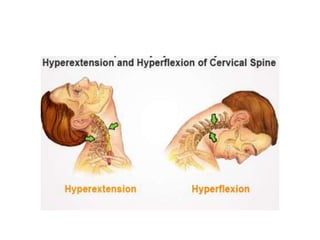
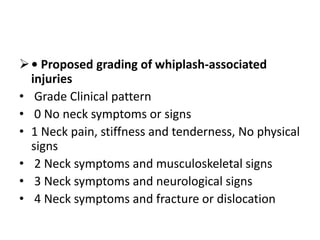
- The cervical vertebrae are the smallest and most movable part of the spine. Injuries can occur from direct or indirect trauma and include fractures, dislocations, and ligament injuries.
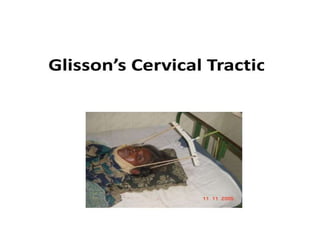
- Treatment depends on the injury but may include immobilization, traction, steroids, and surgery to stabilize or fuse the spine to preserve neurological function and spinal stability.