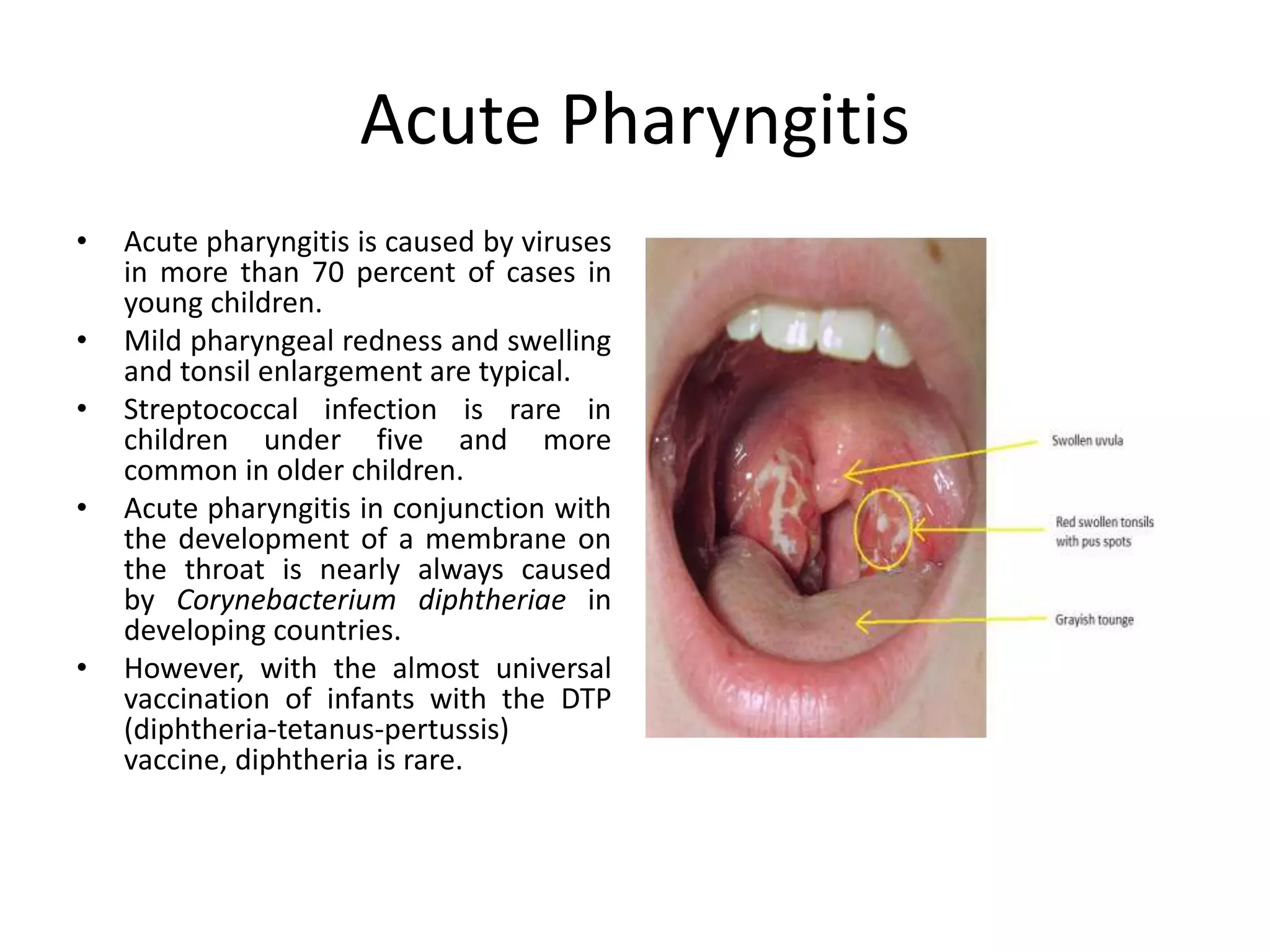
The document discusses respiratory infections in children, including upper respiratory tract infections like sinusitis, pharyngitis, and ear infections, as well as lower respiratory tract infections like pneumonia and bronchiolitis. It describes the anatomy of the upper and lower respiratory tract, signs and symptoms of different infections, common causative agents, and treatment approaches.