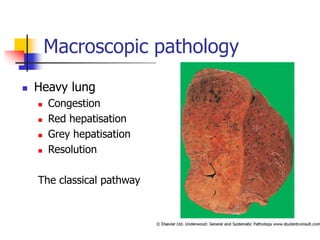
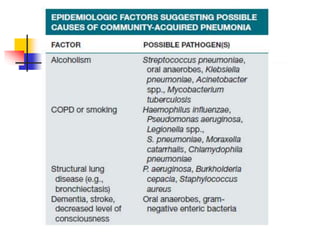
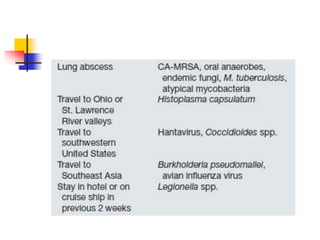
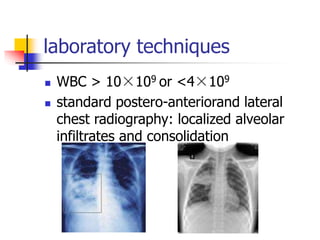
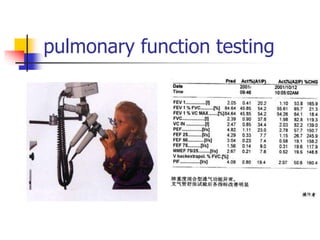
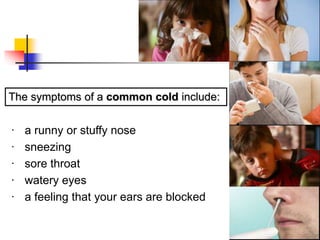
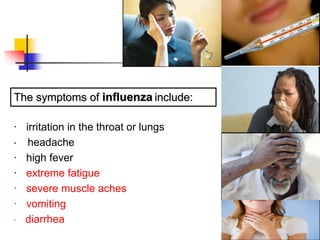
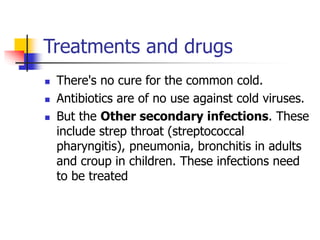
The document discusses respiratory diseases, highlighting their classification, diagnosis, and treatment methods. It covers key issues such as respiratory infections, including common colds and pneumonia, and provides information on symptoms, etiology, and diagnostic procedures. The importance of staying updated with evolving medical knowledge in pulmonary medicine is emphasized for effective patient care.
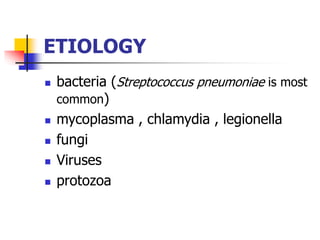
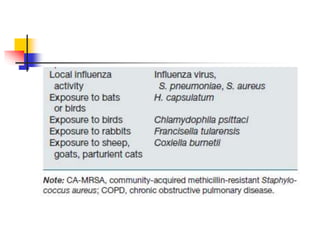
![Organisms
Viruses – influenza, parainfluenza,
measles, varicella-zoster, respiratory
syncytial virus (RSV). Common, often
self limiting but can be complicated
Bacteria
Chlamydia[klə'mɪdɪə] ,
mycoplasma[,maɪko'plɑzmə]
Fungi['fʌŋgi:]](https://image.slidesharecdn.com/pulmonarydiseases-240626214342-8d430bdd/85/Pulmonary-diseasDDDDDDDDDDDDDDDDDDes-ppt-64-320.jpg)
![Microorganisms gain access to the lower
respiratory tract in several ways
The most common way : aspiration from the
oropharynx [,ɔro'færɪŋks] .
Small-volume aspiration occurs frequently during sleep
(especially in the elderly) and in patients with decreased
levels of consciousness
via hematogenous spread
Contiguous extension from an infected
pleural or mediastinal space](https://image.slidesharecdn.com/pulmonarydiseases-240626214342-8d430bdd/85/Pulmonary-diseasDDDDDDDDDDDDDDDDDDes-ppt-68-320.jpg)