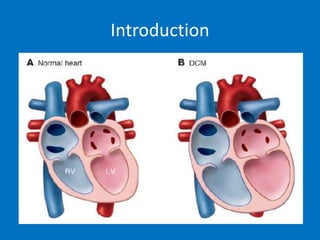
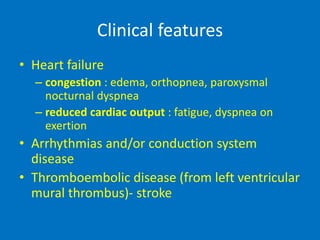
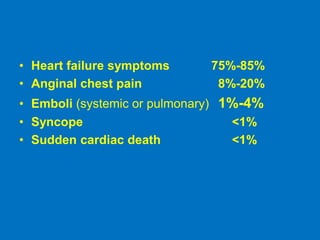
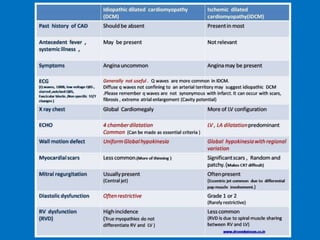
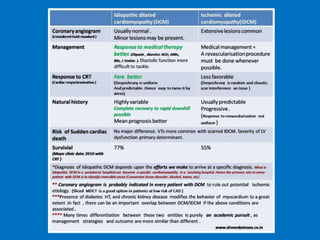
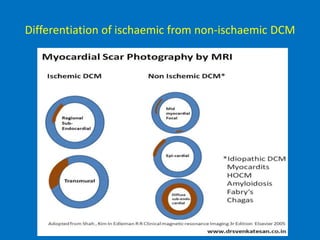
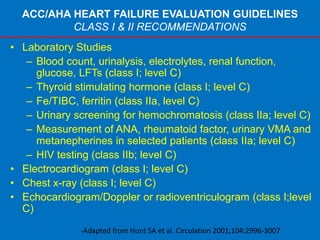
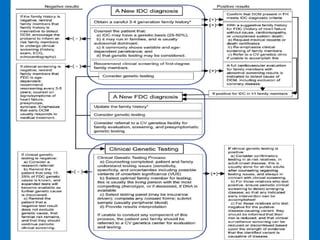
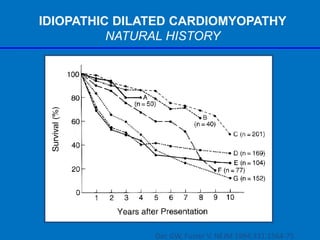
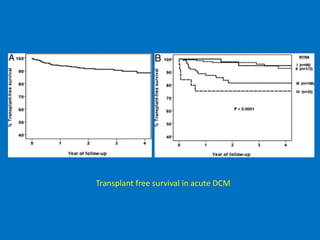
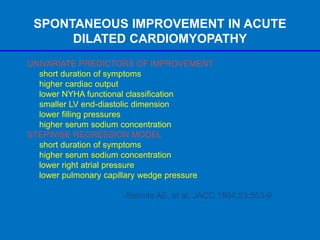
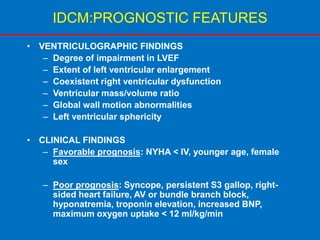
Dilated cardiomyopathy is defined as dilatation and impaired contraction of the left ventricle not caused by ischemic or valvular heart disease. The document discusses the epidemiology, etiology, pathology, genetics, clinical features, diagnosis, and management of idiopathic dilated cardiomyopathy. Key points include:
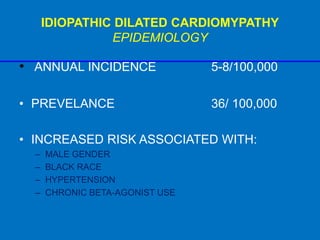
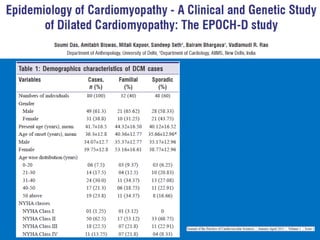
- The annual incidence is 5-8 per 100,000 people with increased risk in males, blacks, and those with hypertension or chronic beta-agonist use.
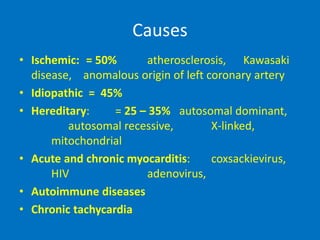
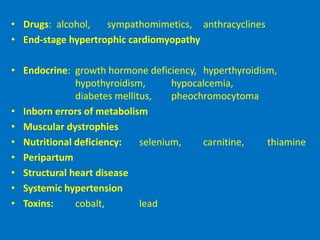
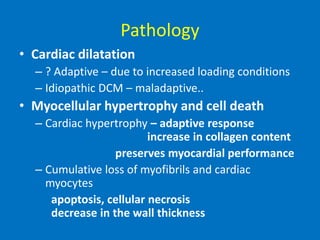
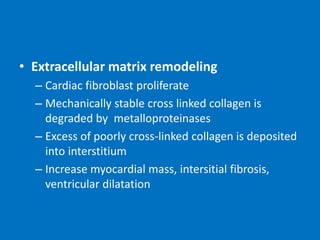
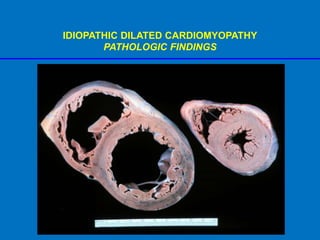
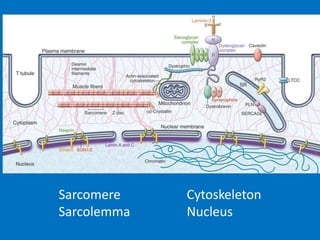
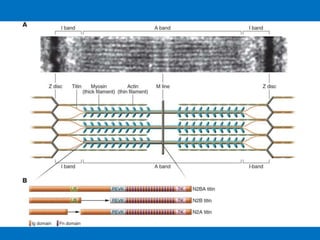
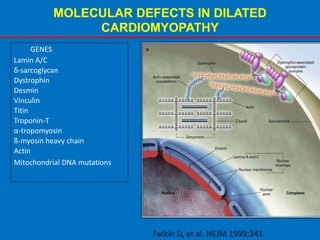
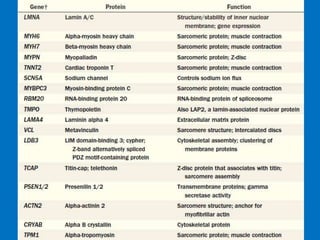
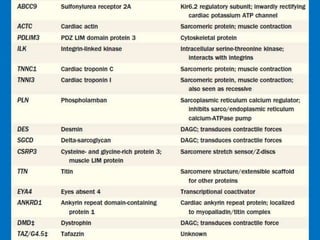
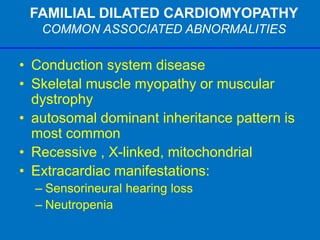
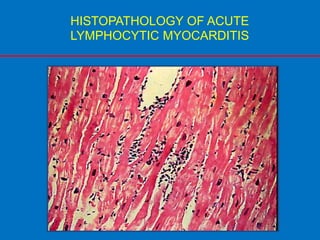
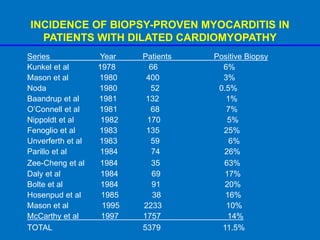
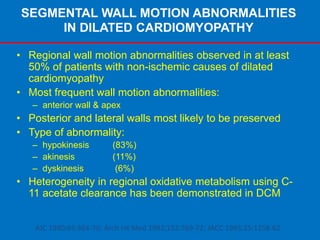
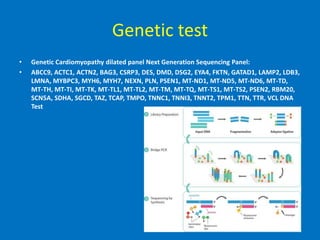
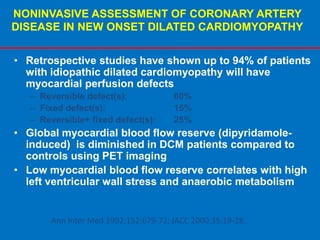
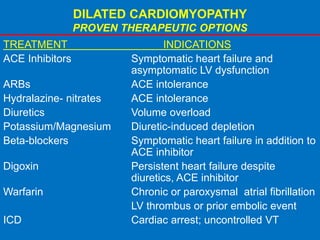
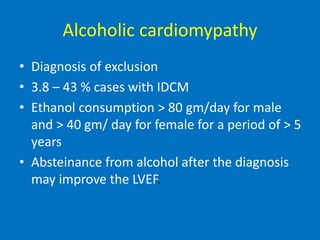
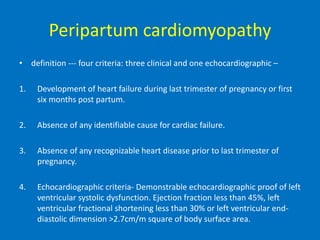
- Causes include genetic mutations, viral infections, autoimmune diseases, and drugs. Pathology shows dilatation, myocyte hypertrophy and death, and extracellular matrix remodeling.
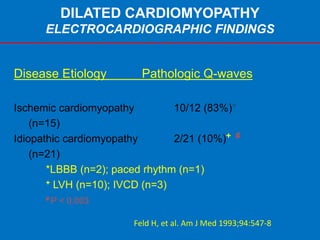
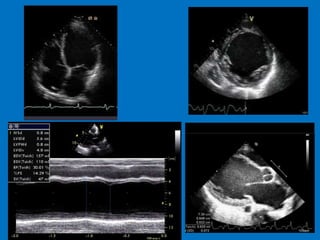
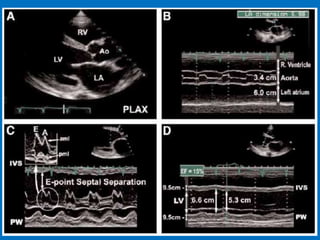
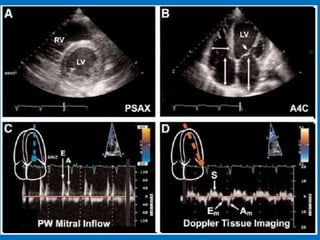
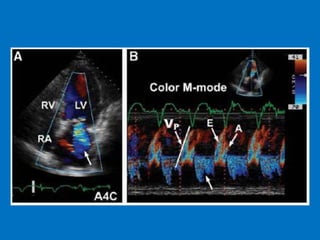
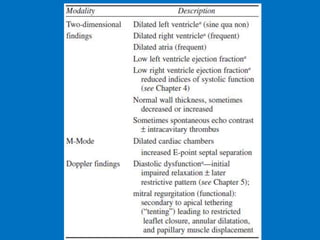
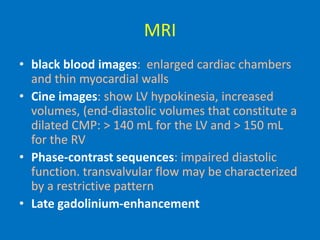
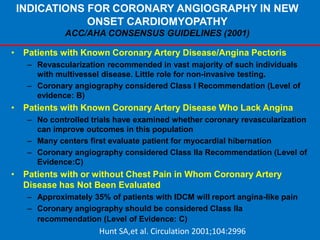
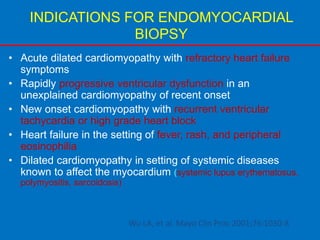
- Diagnosis involves ECG