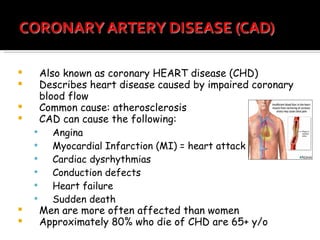
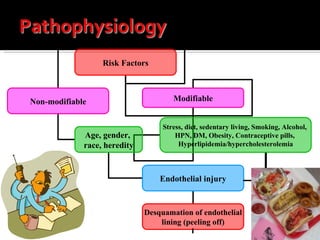
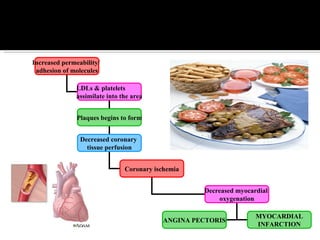
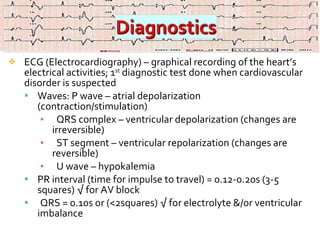
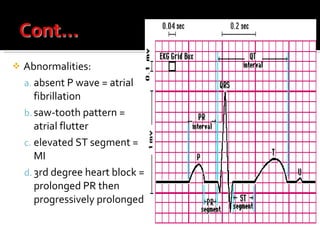
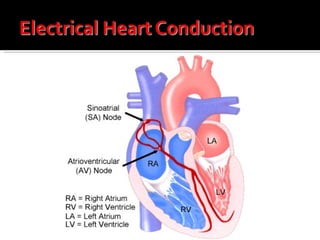
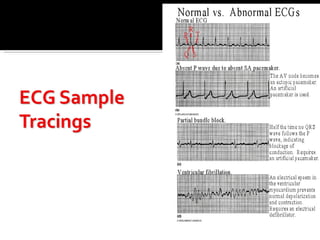
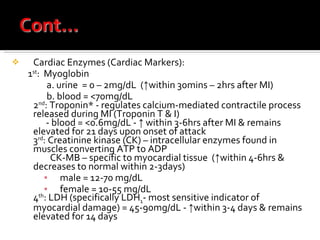
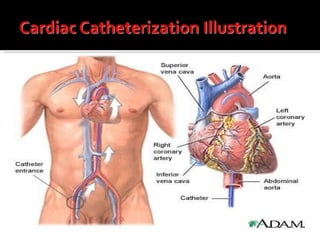
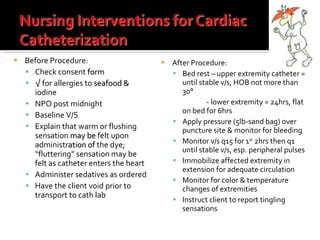
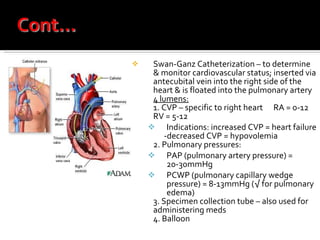
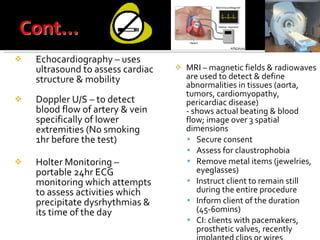
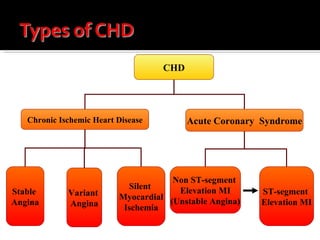
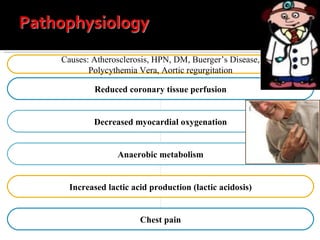
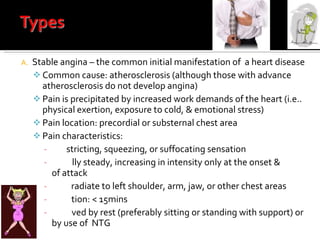
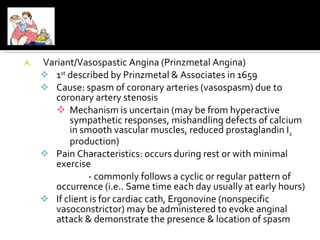
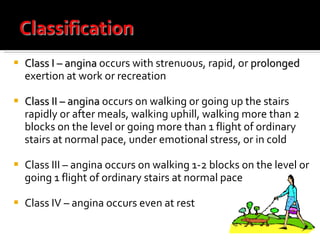
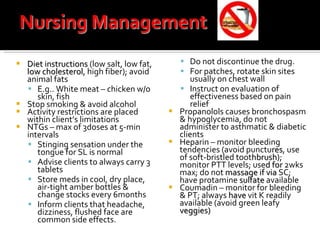
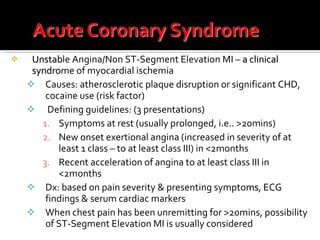
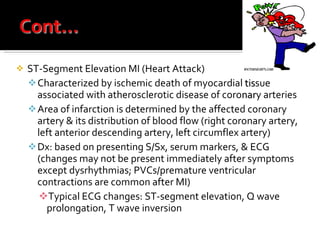
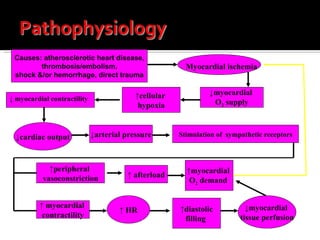
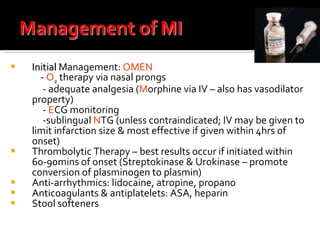
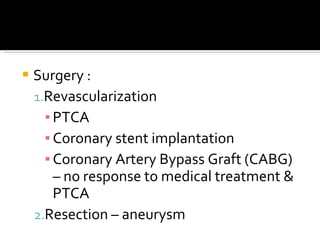
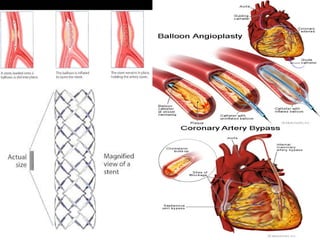
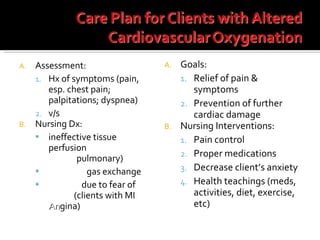
This document provides information on the management of clients with functional cardiac disorders, specifically coronary heart disease (CHD). It discusses the causes, risk factors, pathophysiology, diagnostic tests, and treatment for various types of CHD including stable angina, unstable angina, and myocardial infarction. Diagnostic tests covered include ECG, cardiac enzymes, stress testing, cardiac catheterization, and imaging modalities. Treatment focuses on lifestyle modifications, medications, activity restrictions, and diet instructions to prevent further cardiac events.