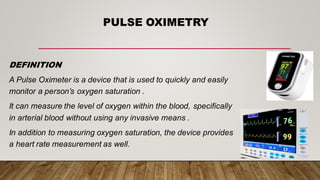
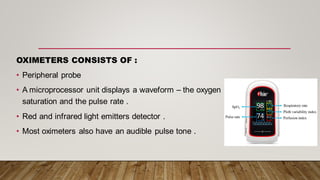
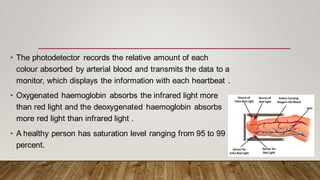
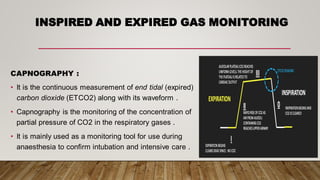
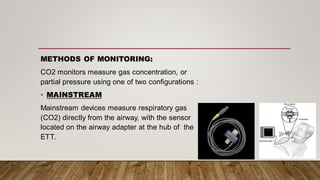
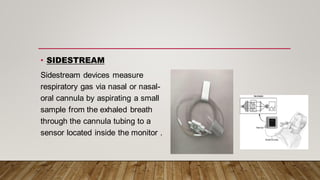
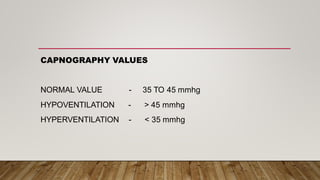
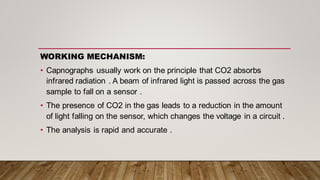
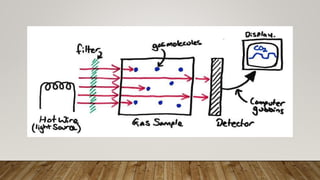
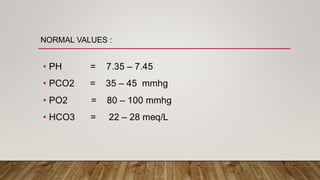
Monitoring devices such as pulse oximetry and inspired and expired gas monitoring are used to monitor a patient's oxygen saturation, respiratory rate, and end-tidal carbon dioxide levels. Pulse oximetry uses light absorption to noninvasively measure oxygen saturation and heart rate, while capnography monitors end-tidal carbon dioxide levels via mainstream or sidestream methods. Blood gas analysis directly measures pH, PCO2, PO2, and HCO3 levels in arterial blood to evaluate respiratory and metabolic function.