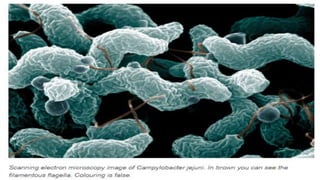
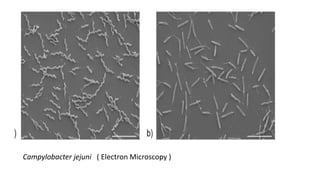
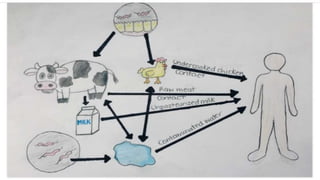
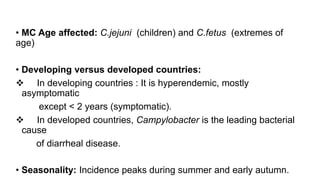
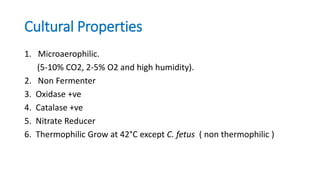
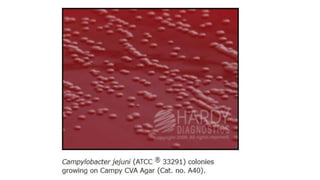
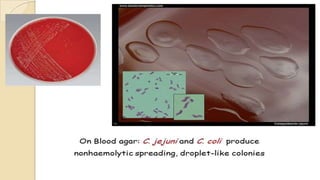
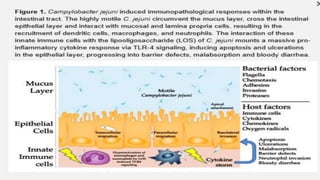
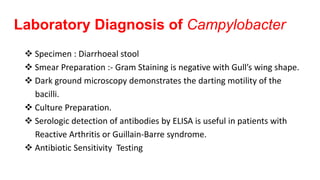
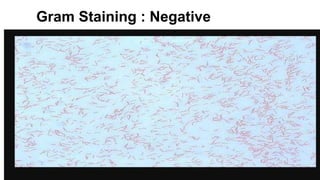
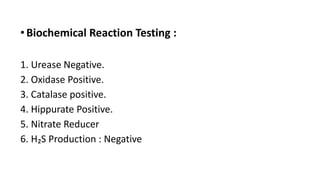
Campylobacter species are microaerophilic, curved gram-negative bacteria that are common causes of diarrheal disease. C. jejuni typically causes intestinal infections resulting in inflammatory diarrhea, abdominal pain, and fever, while C. fetus can cause more systemic infections. People most often acquire campylobacteriosis by ingesting undercooked contaminated poultry, raw milk, or water. The bacteria have a single polar flagellum that allows for darting motility and adherence to host tissues. Laboratory diagnosis involves culture on selective media under microaerophilic conditions and tests for oxidase and catalase production.