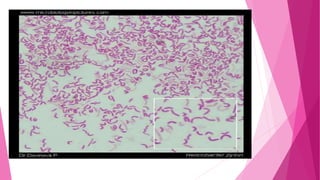
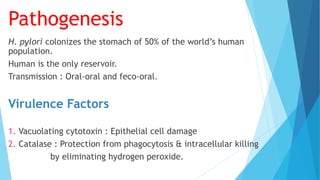
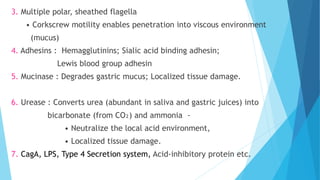
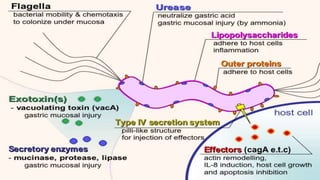
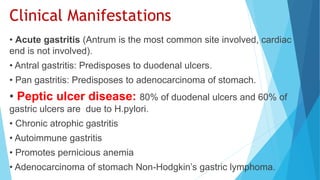
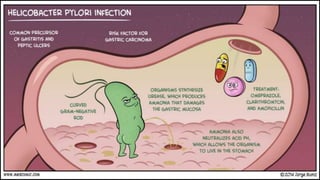
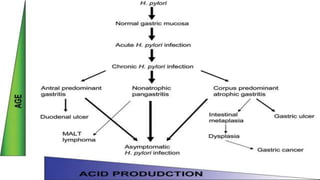
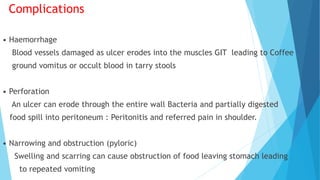
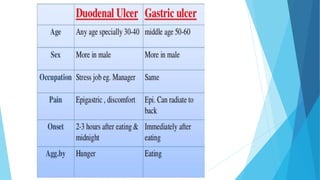
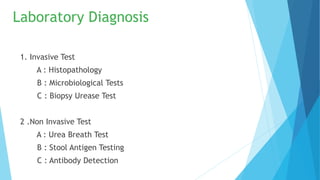
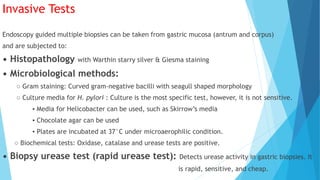
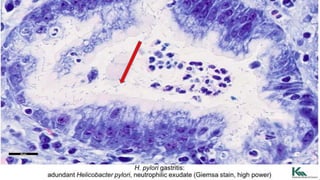
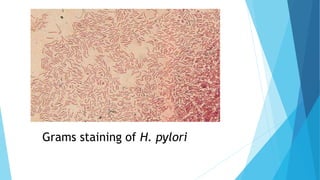
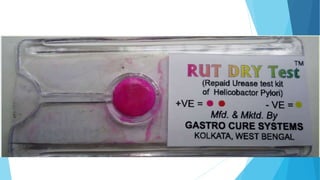
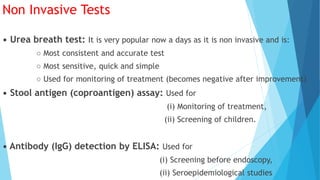
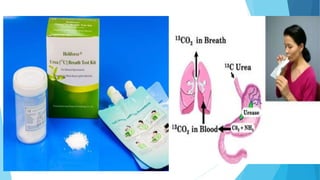
H. pylori is a gram-negative, microaerophilic bacterium that colonizes the stomach and is associated with gastritis, peptic ulcers, and gastric cancer. It is spiral-shaped with multiple sheathed flagella that enable movement. H. pylori infection is transmitted orally and causes inflammation and damage to the gastric mucosa through virulence factors like urease and cytotoxin. Diagnosis involves invasive tests on gastric biopsy or non-invasive breath, stool, and blood tests. Eradication of H. pylori can cure peptic ulcers.