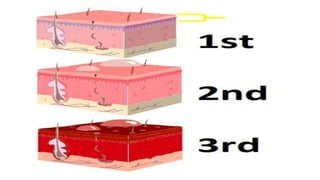
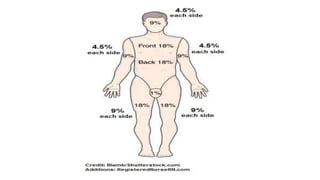
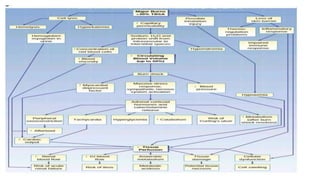
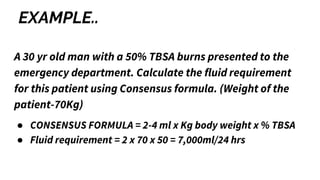
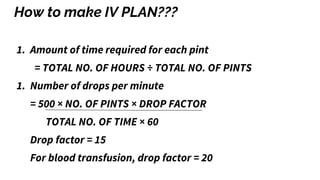
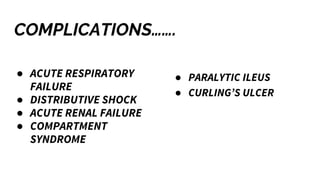
The document outlines the management of burn injuries, emphasizing prevention, early treatment, and rehabilitation to minimize disability and disfigurement. It classifies burns by depth, extent, and severity, detailing the pathophysiology and phases of burn care, including fluid management and infection prevention. Treatment strategies such as wound cleaning, debridement, and grafting using various types of biologic and synthetic dressings are also discussed.