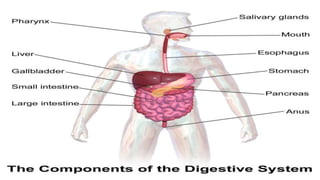
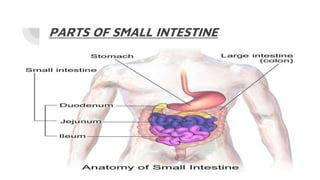
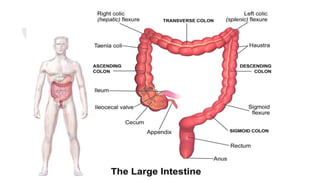
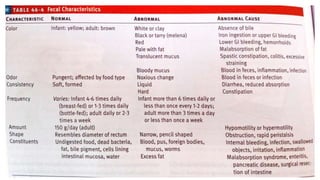
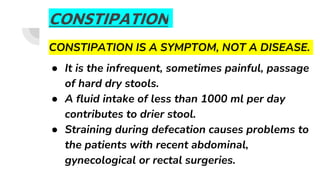
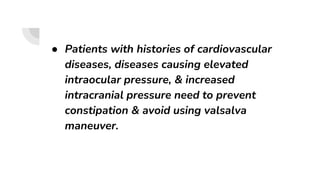
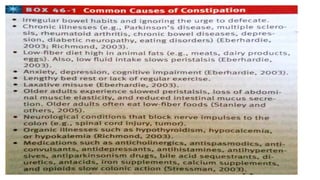
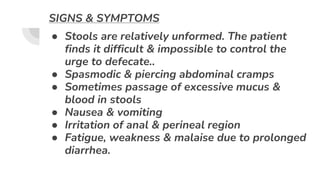
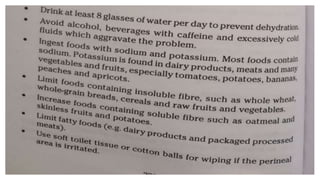
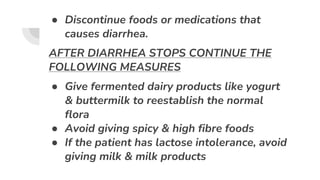
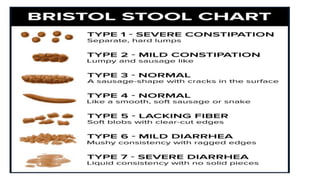
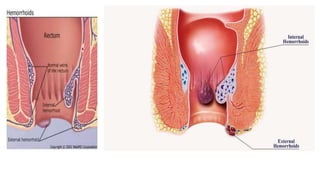
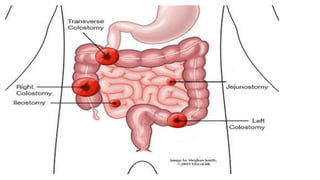
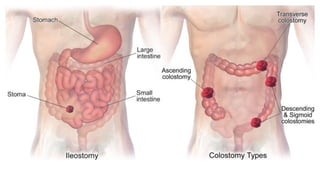
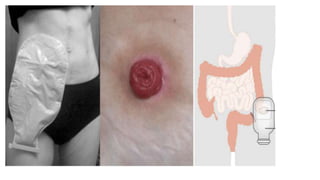
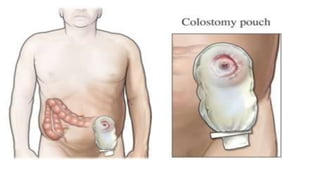
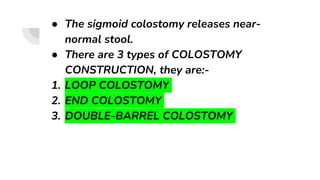
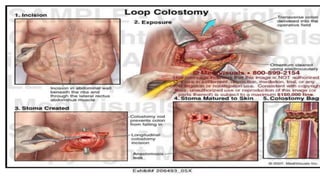
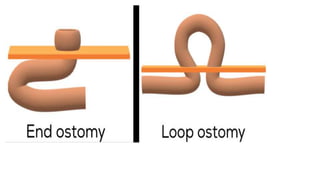
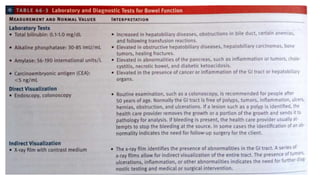
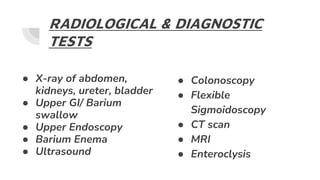
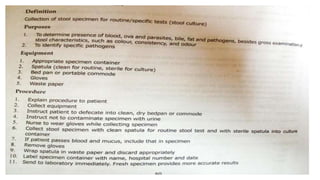
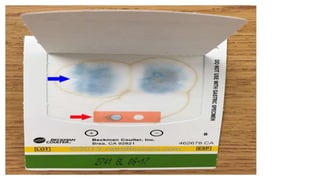
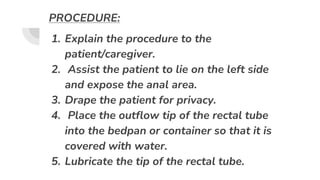
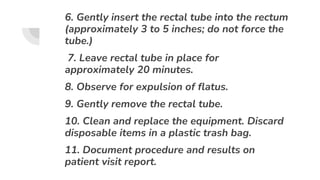
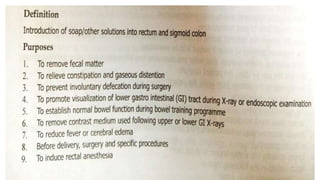
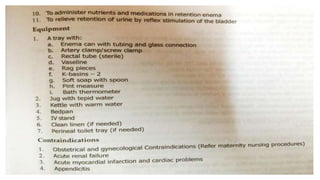
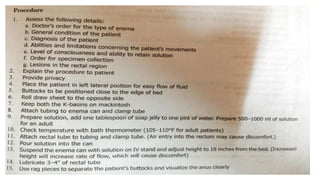
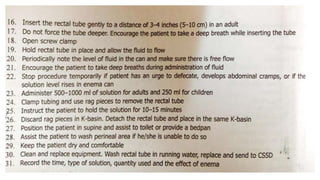
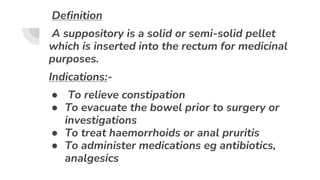
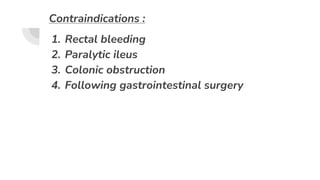
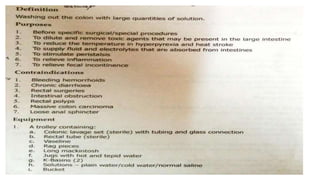
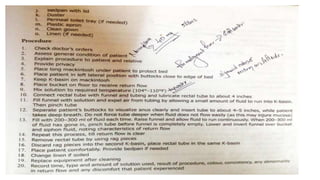
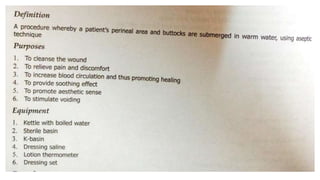
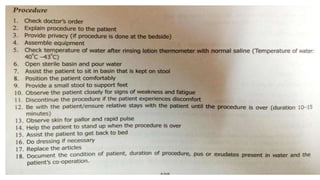
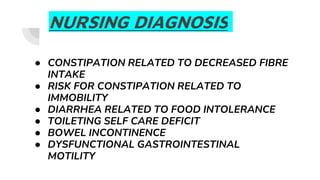
The document provides an overview of bowel elimination, emphasizing its importance for normal body functioning, the anatomy involved, and the mechanisms of stool formation and defecation. It explains common bowel issues such as constipation, diarrhea, fecal incontinence, and the management strategies including dietary changes, medications, and procedural interventions like enemas and digital removal. Additionally, it covers the care required for patients with bowel diversions and the necessary diagnostic tests for assessing bowel function.